Abstract
Objective
The objective of this study was to identify the predictors of incident delirium in this high-risk population.
Methods
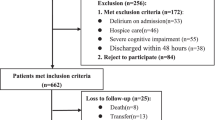
This study was a planned sub-analysis of the INDEED multicentre cohort study. We recruited patients aged ≥ 65, independent/semi-independent, with an emergency department (ED) length of stay ≥ 8 h and admitted to any hospital ward. Patients were followed up during their ED stay up to 24 h after ward admission. Sociodemographic characteristics, comorbidities, functional status (OARS), illness severity, level of frailty, cognitive status (TICS-m) and ED/patient environment evaluation were collected during initial interview. Patients were screened for delirium twice a day using the Confusion Assessment Method. Multivariate logistic regression was performed to identify the predictors of delirium.
Results
Incident delirium was detected in 68 patients of the 612 patients included (11%). Initially, seven candidate predictors were included in a regression model, of which four were retained using a stepwise selection procedure. Presence of cognitive impairment at baseline (OR 3.6, p < 0.001), absence of mobilization during the whole ED length of stay (OR 3.3, p = 0.002), longer ED length of stay (OR 1.02, p = 0.006) were associated with a higher risk of incident delirium while higher functional status was associated with a lower risk (OR 0.8, p < 0.001).
Conclusion
More work is needed to determine which tool(s) are most appropriate for the ED use to increase delirium screening compliance among health professionals working in this department. It is really the first step to be able to suggest interventions to decrease delirium incidence.
Résumé
Objectif
L'objectif de cette étude était d'identifier les prédicteurs du délirium incident dans cette population à hautrisque.
Méthodes
Cette étude était une sous-analyse planifiée de l'étude de cohorte multicentrique INDEED. Nous avons recruté des patients âgés de ≥ 65 ans, indépendants/semi-indépendants, ayant une durée de séjour au département d'urgence (DU) ≥ 8 h et admis dans n'importe quel service. Les patients ont été suivis pendant leur séjour aux urgences jusqu'à 24 h après leur admission. Les caractéristiques sociodémographiques, les comorbidités, l'état fonctionnel (OARS), la gravité de la maladie, le niveau de fragilité, l'état cognitif (TICS-m) et l'évaluation de l'environnement des urgences/patients ont été recueillis lors de l'entretien initial. Les patients ont été soumis à un dépistage du délirium deux fois par jour à l'aide de la méthode d'évaluation de la confusion. Une régression logistique multivariée a été effectuée pour identifier les prédicteurs de délirium.
Résultats
Le délirium incident a été détecté chez 68 des 612 patients inclus (11%). Au départ, sept prédicteurs candidats ont été inclus dans un modèle de régression, dont quatre ont été retenus par une procédure de sélection par étapes. La présence d'un déficit cognitif initial (RC 3,6, p < 0,001), l'absence de mobilisation pendant toute la durée du séjour à l'urgence (RC 3,3, p = 0,002), une durée de séjour plus longue à l'urgence (RC 1,02, p = 0,006) étaient associées à un risque plus élevé de délirium incident, tandis qu'un état fonctionnel plus élevé était associé à un risque plus faible (RC 0,8, p < 0,001).
Conclusions
Des travaux supplémentaires sont nécessaires pour déterminer quel(s) outil(s) sont les plus appropriés au DU afin d'accroître le dépistage du délirium par les professionnels de santé travaillant dans ce service. C'est vraiment la première étape pour pouvoir proposer des interventions visant à diminuer l'incidence du délirium.

Similar content being viewed by others
References
Statistics Canada. Seniors. 2018. Available from: https://www150.statcan.gc.ca/n1/pub/11-402-x/2011000/chap/seniors-aines/seniors-aines-eng.htm. Accessed 10 Aug 2020.
Shah TI, Milosavljevic S, Bath B. Determining geographic accessibility of family physician and nurse practitioner services in relation to the distribution of seniors within two Canadian Prairie Provinces. Soc Sci Med. 2017;194:96–104.
Bonin-Guillaume S, Durand AC, Yahi Curiel F, Berruyer M, Lacroix O, Cretel-Durand E, et al. Predictive factors for ealy unplanned rehospitalization of older adults after an ED visit: role of the caregiver burden. Aging Clin Exp Res. 2015;27(6):883–91.
Cole MG. Delirium in elderly patients. Am J Geriatr Psychiatry. 2004;12(1):7–21.
Emond M, Grenier D, Morin J, Eagles D, Boucher V, Le Sage N, et al. Emergency department stay associated delirium in older patients. Can Geriatr J. 2017;20(1):10–4.
Miu DKY, Chan CW, Kok C. Delirium amond elderly patients admitted to a post-acute care facility and 3-months outcome. Geriatr Gerontol Int. 2016;16(5):586–92.
Krogseth M, Wyller TB, Engedal K, Juliebo V. Delirium is an important predictor of incident dementia among elderly hip fracture patients. Dement Geriatr Cogn Disord. 2011;31(1):63–70.
McCusker J, Cole M, Abrahamowicz M, Primeau F, Belzile E. Delirium predicts 12-month mortality. Arch Intern Med. 2002;162(4):457–63.
National Institute for Health and Care Excellence. Delirium: prevention, diagnosis and management. 2019. Available from: https://www.nice.org.uk/guidance/cg103. Accessed 10 Aug 2020.
Boucher V, Lamontagne M-E, Nadeau A, Carmichael P-H, Yadav K, Voyer P, et al. Unrecognized incident delirium in older emergency department patients. J Emerg Med. 2019;57(4):535–42.
Sugalski G, Ullo M. Making sense of delirium in the emergency department. Emergency Medicine Reports. 2019. Available at https://www.reliasmedia.com/articles/143932-making-sense-of-delirium-in-the-emergency-department. Accessed 5 Apr 2020.
Bo M, Bonetto M, Bottignole G, Porrino P, Coppo E, Tibaldi M, et al. Length of stay in the emergency department and occurrence of delirium in older medical patients. J Am Geriatr Soc. 2016;64(5):1114–9.
Kennedy M, Enander RA, Tardiri SP, Wolfe RE, Shapiro NI, Marcantonio ER. Delirium risk prediction, healthcare use and mortality of elderly adults in the emergency department. JAGS. 2014;62:462–9.
Inouye SK, Charpentier PA. Precipating factors for delirium in hospitalized elderly persons. JAMA. 1996;275(11):852–7.
Laurila JV, Laakkonen ML, Timo SE, Reijo TS. Predisposing and precipating factors for delirium in a frail geriatric population. J Psychosom Res. 2008;65(3):249–54.
Ministère de la Santé et des Services Sociaux. Approche adaptée à la personne âgée en milieu hospitalier—Cadre de référence. 2011. Available at http://www.msss.gouv.qc.ca. Accessed 6 Feb 2020.
Émond M, Boucher V, Carmichael PH, Voyer P, Pelletier M, Gouin E, et al. Incidence of delirium in the Canadian emergency department and its consequences on hospital length of stay: a prospective observational multicentre cohort study. BMJ open. 2018;8(3):1–9.
Frenkel WJ, Jongerius EJ, Mandjes-van Uitert MJ, van Munster BC, de Rooij SE. Validation of the Charlson Comorbidity Index in acutely hospitalized elderly adults: a prospective cohort study. J Am Geriatr Soc. 2014;62(2):342–6.
Fillenbaum GG, Duke U. Multidimensional functional assessment of older adults: the Duke Older Americans Resources and Services procedures. Hillsdale, NJ: L Erlbaum Associates; 1988. p. 179.
Knaus WA, Draper EA, Wagner DP, Zimmerman JE. APACHE II: a severity of disease classification system. Crit Care Med. 1985;13(10):818–29.
Rockwood K, Song X, MacKnight C, Bergman H, Hogan DB, McDowell I, et al. A global clinical measure of fitness and frailty in elderly people. CMAJ. 2005;173(5):489–95.
de Jager C, Budge M, Clarke R. Utility of TICS-m for the assessment of cognitive function in older adults. Int J Geriatr psychiatry. 2003;18(4):318–24.
Knopman DS, Roberts RO, Geda YE, Pankratz VS, Christianson TJH, Petersen RC, et al. Validation of the telephone interview for cognitive status-modified in subjects with normal cognition, mild cognitive impairment, or dementia. Neuroepidemiology. 2010;34(1):34–42.
Inouye SK, van Dyck CH, Alessi CA, Balkin S, Siegal AP, Horwitz RI. Clarifying confusion: the confusion assessment method. A new method for detection of delirium. Ann Intern Med. 1990;113(12):941–8.
Monette J, Galbaud du Fort G, Fung SH, Massoud F, Moride Y, Arsenault L, et al. Evaluation of the Confusion Assessment Method (CAM) as a screening tool for delirium in the emergency room. Gen Hosp Psychiatry. 2001;23(1):20–5.
Inouye SK. The Confusion Assessment Method (CAM): training manual and coding guide Boston: Hospital Elder Life Program. 2003. Available from: www.hospitalelderlifeprogram.org. Accessed 3 Aug 2020.
McCusker J, Cole MG, Dendukuri N, Belzile E. The delirium index, a measure of the severity of delirium: new findings on reliability, validity, and responsiveness. J Am Geriatr Soc. 2004;52(10):1744–9.
Kelly AM. The minimum clinically significant difference in visual analogue scale pain score does not differ with severity of pain. Emerg Med J. 2001;18:205–7.
Hosmer DWJ, Lemeshow S, Sturdivant RX. Applied logistic regression. 3rd Edition ed. Statistics WSiPa; 2013. p. 528.
Lindroth H, Bratzke L, Purvis S, Brown RM, Coburn M, MrKobrada M, et al. Systematic review of prediction models for delirium in the older adult inpatient. BMJ open. 2018;8(4):1–22.
Institut Canadien d'Information sur la Santé. Nombre de visites au service d'urgence et durée du séjour, 2018–2019. 2018. Available from: https://www.cihi.ca/fr/search?query-all=temps+d%27attente+%C3%A0+l%27urgence&Search+Submit=. Accessed 21 Apr 2020.
Acknowledgements
The authors would like to thank Suzy Lavoie and research assistants who participated in the recruitment of patients for this study.
Funding
This study was funded by the Fonds Québécois de Recherche en Santé (FQRS 29307).
Author information
Authors and Affiliations
Contributions
MÉ had full access to all of the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis. He was responsible for design, funding and conduct of the study. VB managed the study. EB, AN and PHC led the statistical analyses and data interpretations. EB and AN wrote the manuscript. MP, RD, ÉG, SB and MÉ were responsible for recruitment at all five sites. PV, MM, SL, MÈL and LM are all collaborators of INDEED project. MÉ, VB, PHC, PV, MP, ÉG, RD, SB, MÈL, MM, and SL reviewed and approved the manuscript. Sponsor’s role. N/A.
Corresponding author
Ethics declarations
Conflict of interest
The authors have no conflicts.
Rights and permissions
About this article
Cite this article
Béland, E., Nadeau, A., Carmichael, PH. et al. Predictors of delirium in older patients at the emergency department: a prospective multicentre derivation study. Can J Emerg Med 23, 330–336 (2021). https://doi.org/10.1007/s43678-020-00004-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s43678-020-00004-8