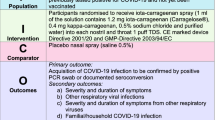
Abstract
Clinical management of COVID-19 has been a daunting task. Due to the lack of specific treatment, vaccines have been regarded as the first line of defence. Innate responses and cell-mediated systemic immunity, including serum antibodies, have been the primary focus of practically all studies of the immune response to COVID-19. However, owing to the difficulties encountered by the conventional route, alternative routes for prophylaxis and therapy became the need of the hour. The first site invaded by SARS-CoV-2 is the upper respiratory tract. Nasal vaccines are already in different stages of development. Apart from prophylactic purposes, mucosal immunity can be exploited for therapeutic purposes too. The nasal route for drug delivery offers many advantages over the conventional route. Besides offering a needle-free delivery, they can be self-administered. They present less logistical burden as there is no need for refrigeration. The present article focuses on various aspects of nasal spray for eliminating COVID-19.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
In December 2019, pneumonia incidences of unknown origin were reported in Wuhan, China, and was identified to be severe acute respiratory syndrome coronavirus-2 (SARS-CoV-2). Owing to the widespread transmission of SARS-CoV-2 along with thousands of fatalities, the World Health Organization (WHO) declared it a pandemic on March 12, 2020. The disease that SARS-CoV-2 virus caused was named coronavirus disease-2019 (COVID-19) [1, 2].
Until December 2019, a total of six coronavirus (CoV) strains had been identified to infect humans, leading to respiratory illnesses. The CoVs HCoV229E, HCoVOC43, HCoVNL63, and HKU1 generally caused minor upper respiratory illnesses with sporadic significant infections in infants, younger children, along with elder people [3]. However, SARS-CoV and Middle East respiratory syndrome coronavirus (MERS-CoV), infects the lower respiratory tract resulting in serious and life threatening respiratory illness in people. SARS-CoV and MERS-CoV are known to have been transmitted from bats to palm civets, dromedary camels, and subsequently to humans [4].
Due to the rapid mutation and transmission rate of CoVs, the available medications and vaccines require constant updating as the antibody neutralization efficacy decreases dramatically with each new variant. RNA viruses are known to mutate at higher rates as compared to DNA viruses. There are persistent reports of several mutations within the SARS-CoV-2 spike (S) protein gene [5]. The ease with which SARS-CoV-2 can spread from one host to another provides it with further opportunities to mutate. Knowledge regarding sequencing aids to find newly developed SARS-CoV-2 variations and mutations that could be connected to modifications in the viral characteristics. As of current scenario of COVID-19, the most promising approach to eradicate the virus is to prevent transmission of virus via acquired immunity in the community through administration of COVID-19 vaccines [6]. The initiative for vaccine development in the COVID-19 pandemic phase has been exceptional in terms of size, pace, and distribution network as compared to traditional vaccines [7]. The categories of COVID-19 vaccines belong to four categories—whole viruses, protein-based vaccines, viral vectors, and nucleic acid-based vaccines [8]. However, much uncertainty remains regarding the current, faster COVID-19 vaccine development. Scale-up production of the COVID-19 vaccine has been challenging. Short shelf life and particular temperature storage conditions are also a problem with vaccines. It is difficult to follow the restricted cold-chain system capacity for vaccine storage [9]. As such, further vaccination tools such as needles and syringes can be used to limit the vaccine supply. The number of doses that a vial can offer depends upon the syringe-needle combination, the skills of vaccinators, etc. Uncertainties in the number of doses can be posed a challenge in scheduling vaccination campaigns. Demand for COVID-19 vaccines has been outpacing supply, yet demand variation may culminate in the wastage of vaccine doses. Many instances can be cited wherein vaccines are discarded as fewer candidates than anticipated turned up to receive vaccines [8].
Vaccine reluctance is one of the factors influencing demand variability. As per the survey conducted by Yigit et al., vaccine hesitancy can be attributed to various social, political, economic, religious, and cultural factors. The study also revealed an inclination of the participants toward domestic vaccines compared to foreign [10]. As evident from the literature, some of the reasons for vaccine reluctance are skepticism of vaccine benefits, unanticipated future consequences, inclination toward natural immunity, etc. Apart from reluctance, vaccination fatigue is also one of the reasons as vaccines are administered in multiple doses. The cost of vaccinations is another barrier limiting the demand for vaccines. As per the survey by Tagoe and researchers, the COVID-19 vaccination campaign (due to higher costs) is limited in several ways to lower-middle-income countries [11]. Lack of coordination, poor telecommunication, and internet connectivity in the distribution and monitoring of vaccines can be posed a hurdle to poor monitoring of vaccination programs. As the vaccines have to be injected, trained staff are required and, as such, an inadequate number of trained health providers has been another obstacle to vaccine delivery [12]. Considering the problems with injectable vaccines and highest SARS-CoV-2 viral loads in the oral cavity, nasal or oral sprays provide a promising alternative to reduce infectious viral load transmission [13]. Herein, we review the use of nasal sprays currently in the market which may be useful in inactivating SARS-CoV-2.
Nasal route for COVID-19 management
The nasal epithelium is the primary site of SARS-CoV-2 infection, which further spreads to the respiratory tract where a high viral load is detected [14, 15]. The nasal cells of the olfactory neuroepithelium constitute an abundant amount of angiotensin converting enzyme 2 (ACE2) protein, which is 200 to 700 times greater than other nasal cells [16]. Nasal vaccination may provide immunity in distant mucosal organs. Nasal vaccination prevents pathogens from entering the body by producing a particular immune response in the mucosal tissue. Mucosal immunity of the nasal cavity is induced at nasal-associated lymphoid tissues [17], which is an organized mucosal immune system, consisting of B and T lymphocytes and, antigen-presenting cells [18]. An epithelial layer that contains memory (M) cells, which demonstrate a crucial role in antigen ingestion from the mucosa, protects this mucosal immune system. This assists in the rapid absorption of the vaccine into the circulatory system and enhances its effectiveness [19,20,21].
In human phase I and II clinical trials, intravenous administered IgG1 isotype-neutralizing monoclonal antibodies were shown to have inefficient penetration into mucosal tissues [22]. Antibody titers in the lungs were 200–500 times lower as compared to those in the serum [23]. High-dose intravenous administration of IgG1 isotype-neutralizing monoclonal antibodies also did not achieve an efficient antiviral effect on the respiratory tract. Intravenous administration of drugs results in drug concentration being diluted in the plasma [24]. For treating mucosal viral infections, mucosal administration is a possible alternative to intravenous infusion. Intranasal administered antibodies primarily target the respiratory system, with long-term circulation in the nasal cavity and lung [14, 25]. During the outbreak of highly infectious diseases, allied health professionals such as pharmacists or nurses can perform mass vaccinations if invasive mucosal routes like intranasal routes are selected as a needle-free vaccination approach. Vaccines in the form of liquids and dry powder formulations are feasible to be administered by the intranasal route. Such formulations have no transportation and wastage issues, and remain relatively stable without cold-chain requirement. Numerous microvilli are present in nasal mucosal membranes, increasing the surface area and blood supply for absorption, resulting in rapid onset immune response [26]. Good patient compliance can be achieved owing to ease of administration, affordable cost, and convenience of disposal.
With intranasal administration, the desired drug concentration can be achieved in the central nervous system via the porous cribriform plate, which is an anatomically porous bone present in the upper nasal cavity. In addition, when a drug is injected into the cerebrospinal fluid, arachnoid villi draining into the venous circulation lowers the concentration of the drug. Thus, intranasal administration of drugs is advantageous in the neurological presentations of COVID-19. Several other benefits offered are free from systemic side effects, targeted drug delivery to the central nervous system, no venous drainage or dilution in plasma thereby lowering the dose, delivery in the vaporized form to reach the porous cribriform plate, maintaining integrity of the blood–brain barrier [27].
Role of secretory IgA and IgG for sterilizing respiratory tract
The initial event in the pathogenesis of inflammatory respiratory illness is triggered by an increase in bacterial IgA1 protease, which disrupts the nasal mucosal immune barrier in a particular region. [28, 29]. Initially, local polymeric IgA antibodies are secreted, which block the pathogen’s binding to the nasal epithelial receptors [21]. Simultaneously, the antigen-loaded dendritic cells (DC) become mature and migrate toward the follicular B cell and interfollicular T cell areas. Here, they expose nearby naive T cells to antigens, triggering the onset of adaptive cellular immunity [22]. Activated T cells and B lymphoblasts move through the bloodstream and contribute toward systemic immunity after being activated by antigens. Additionally, the common mucosal immune system, which connects inductive mucosal sites with effector sites, disseminates primed immune cells [30].
In one study, IgG antibodies were twice as effective than plasma IgA against SARS-CoV-2 spike protein. However, as the predominant type of antibody in the nasopharynx, IgA dimers were 15 times more effective against the same target than IgA monomers. Therefore, dimeric IgA may be especially useful for vaccination effectiveness and prevention against SARS-CoV-2 [31].
The viral infection of epithelial cells in the nasal pharynx initiates as an interaction of the receptor-binding domain of S protein and ACE-2 [32,33,34,35]. SARS-CoV-2 transmits to other epithelial cells that express ACE-2, particularly in the gut and lungs. These tissues, which are categorized as nasopharynx, gut, and bronchial-associated lymphoid tissues, are densely packed with lymphoid cells. These lymphoid tissues are specifically targeted by inhaled vaccines, which have been demonstrated to be more efficient in killing SARS-CoV-2 [36].
Both the upper and lower respiratory tracts exhibit plasma-derived IgG. IgG causes inflammation by inducing the complement system, phagocytes such as neutrophils and macrophages, and natural killer (NK) cells.
An essential function of IgG in the lower respiratory tract is its specialized action against bacteria or antigens. IgG2 is particularly significant as a reservoir for antibodies against numerous prevalent bacteria that cause pneumonia. The specific activity or affinity of IgG antibody for microorganisms, causes opsonization or coating of the microorganism followed by interaction with its complement cascade. These lead to lysis, which could directly kill the microbe or cause an alveolar macrophage to phagocytize and destroy it inside the cell. The complement protein C3b may work as an additional opsonin that enhances phagocyte adhesion to a membrane receptor and, as a result, promotes antibody intake. This opsonic antibody, which is engulfed by the phagolysosome of a cell, can furthermore assist in killing microorganisms intracellularly. Opsonization of microorganisms may occur by antibodies called immune opsonin as well as by surfactant and fibronectin fragments called non-immune opsonins [37,38,39]. When compared to the absorption of non-opsonized or uncoated bacteria, the phagocytic uptake of viable bacteria having an IgG antibody coat is much higher in alveolar macrophages [40].
Nasal cycle and nasal disease
The nasal cavity is the first line of defence against respiratory infections and also a mediator for airflow passage. The nasal passages are symmetrical and are composed of both bony and cartilaginous parts. The nasal valve, the smallest part of nasal tube, maintains nasal airflow resistance. Sympathetic innervation and tone in the venous sinusoids actively regulate the breadth of the nasal cavity. The nasal cycle (NC) is the impulsive congested and non-congested nasal mucosa that occurs during the day, with congested nasal mucosa on each side followed by uncongested nasal mucosa on the opposite. NC can only be observed in patients with deviated septum and rhinitis [41]. The venous cavernous tissue in the submucosa of the turbinate and septum dilates or constricts during the nasal cycle. The airflow via the two nasal passages is typically uneven when the nose is infected with a viral infection and whenever the body is in a supine posture and the asymmetry is accentuated [42]. There are four distinct types of NC patterns, classic (reciprocal congestion/decongestion alterations, constant total volume); parallel (congestion/decongestion occurring inside nasal cavities simultaneously); irregular (mutual alteration in nasal volume without a specific pattern and a constant total nasal volume); and acyclic (total nasal volume in nostrils do not differ) [43].
Nasal disease
Nasal symptoms, including sneezing, pruritus, rhinorrhoea, and nasal congestion, are referred to as rhinitis. Different types are: allergic rhinitis, infectious rhinitis, and non-allergic, non-infectious rhinitis [44].
Infectious rhinitis
Acute viral rhinitis is an upper respiratory infection and is often caused by rhinoviruses, coronaviruses, adenoviruses, influenza, parainfluenza, respiratory syncytial viruses, and enteroviruses. These viruses have the ability to destroy tight junctions of epithelial cells, rupture their layers, enter epithelial cells, and regulate the metabolic activity of the host cell, utilizing it for their own growth and resulting in necrosis of the host cells [44]. When a person experiences an upper respiratory tract infection (URTI), congested nose and spontaneous and reciprocal changes in nasal airway resistance becomes much more obvious. The unilateral nasal resistance in URTI patients is significantly pronounced than the unilateral resistance in healthy individuals. Due to increased maximal unilateral nasal airway resistance, the nasal passages become severely congested and frequently totally unilaterally closed [41].
Allergic rhinitis
Allergens are proteins found in airborne particles such as pollen, mites, excreta of insects, animal dander, and molds that cause allergic rhinitis. A variety of environmental allergens can trigger allergic rhinitis that is characterized as an IgE-mediated, type I hypersensitivity response. The indications of allergic rhinitis include rhinorrhoea, nasal congestion, a scratchy nose, and sneezing that lasts longer than an hour on two or more consecutive days. Asthma and conjunctivitis are common diseases associated with allergic rhinitis. It has been shown that rhinitis interferes with NC expression. Nasal mucosa inflammation causes resistance to vascular vasodilatation, and hence increases pressure in sinusoids that results in nasal congestion. The frequency of the periodic reciprocal changes in the nasal airways results in increasing unilateral nasal congestion; resistance rises during allergic rhinitis [44].
Non-allergic rhinitis
Chronic non-allergic rhinitis is characterized by a loss of endonasal infection and systemic allergic inflammatory clinical symptoms. An inflamed nasal inner lining causes symptoms like nasal blockage, rhinorrhoea (posteriorly or anteriorly), sneezing, or nasal itching known as chronic rhinitis. Patients suffering from non-allergic rhinitis can be categorized as drug-induced, hormone-induced, senile or geriatric, gustatory, occupational, idiopathic and atrophic rhinitis [44].
Nasal spray for COVID-19 vaccination
Amidst the COVID-19 pandemic, several intramuscular vaccines were developed, approved, and rolled-out. However, conventional vaccines suffer from drawbacks including storage difficulties and reluctance of needle vaccination routes. Nose being the initial site of the virus for replication and transmission, nasally inhaled vaccines can be viewed as a promising alternative in stimulating immunity. Compared to conventional routes, nasal route of administration can induce both topical and systemic immune responses [45]. In addition, directly boosting immunity in the nose would reduce the spread of the virus to other individuals. Nasal spray vaccines might be thought of as a more affordable option in developing nations [46].
Barriers to nasal vaccine development
A nasal vaccine should contain antigens to elicit a specific adaptive immune response and immune stimulants, which can activate the innate immune system. Moreover, a device for the effective delivery of contents would be required. In order for the vaccine to be absorbed through the mucosal layer, the nasal vaccine needs to overcome the nasal barrier, i.e., sticky mucosa and cilia. Mucociliary clearance leads to decreased vaccine absorption. The vaccine is more likely to induce Th17 immune responses when given intranasally, which may hinder elimination of SARS-CoV-2 from the lungs [45]. Another barrier is the requirement of a unique delivery device, which can impose a financial obligation in the formulation of vaccines [47]. In addition, the vaccine contents should be compatible with various excipients used in the intranasal vaccine [48]. For a nasal vaccine to be successful, it should be able to address the above challenges.
Excipients and delivery systems
Vaccine formulations contain various agents like stabilizers, cryoprotectants, antibiotics etc., which complement the immunogenicity and effectiveness of vaccine. Recently, nanocarriers also are incorporated depending on the type of formulation. As far as stability of nasal vaccine is concerned, storage temperature and pH is of prime importance. Stabilizers aid in enhancing the vaccine’s thermostability. Widely used nasal vaccine stabilizers are arginine, hydrolyzed porcine gelatin, monosodium glutamate, gelatin, sucrose, sorbitol, L-alanine, and tricine [49]. Some of the most often employed mucosal adjuvants promoting mucosal immunization, especially via the intranasal route, include heat-labile enterotoxin, a-galactosyl ceramide (aGalCer) chitosan, and cholera toxin. Toll-like receptor agonists have been studied as mucosal adjuvants including mono-phosphoryl lipid A, macrophage-activating lipopeptide, and cytosine-phosphate-guanine [50].
Nasal vaccines
Lactobacillus, a probiotic commonly used in yogurt fermentation, has been used as an antigen delivery mode for nasal spray vaccines. This method induces local immune responses minimizing viral entrance and replication [51]. Several nasal spray vaccines are summarized in Table 1 [52].
Nasal spray for COVID-19 treatment
Despite the increasing vaccination rates around the world, the spread of the virus does not appear to have been slowed as anticipated. Even after parenteral vaccination, the nose is likely to continue to be a source of infectious viral transmission. Moreover, the high viral mutation rates makes prophylaxis challenging. Along with prophylaxis, treatment is equally significant which are limited [53]. Antivirals such as hydroxychloroquine, remdesivir, lopinavir, and supporting agents like corticosteroids, ascorbic acid are currently being used. These drugs are administered orally or via intravenous routes. Owing to the fact that nose is the first site of invasion by virus, exploration of the pulmonary route for drug delivery to manage COVID-19 infection is an attractive choice. The site of primary infection (upper respiratory tract and central pulmonary airways by surface contact or deposition of inhaled droplets), the development of COVID-19, and the biology of the pulmonary airways reflect a more plausible remedial strategy for the treatment of COVID-19 [54]. Owing to advantage of the directly delivering agent to the site of primary illness, nasal administration of medications has recently garnered a lot of attention (Figs. 1 and 2).
Antibody-induced disease enhancement in respiratory viruses—immune complexes are formed between non-neutralizing antibodies and viral antigens in the airway tissues, leading to events such as—secretion of pro-inflammatory cytokines, recruitment of immune cells, and activation of the complement cascade in lung tissue. The resulting inflammation can cause airway obstruction and acute respiratory distress syndrome in severe cases. (Figure created with biorender.com)
Nitric oxide nasal spray (NONS)
For decades, the pharmacology, toxicity, as well as data on safety for nitric oxide (NO) use in humans have been known. NO is implicated in innate immunity, wound healing, vasodilation, neurotransmission, and angiogenesis. NO is being viewed as a potential candidate against SARS-CoV-2 as shown in Fig. 3 [55], with several studies being conducted to determine its efficacy as a nasal spray option.
A nitric oxide nasal spray (NONS) manufactured by SaNOtize was found to reduce COVID-19 viral loads to significant levels in patients [56, 57]. Most intriguingly, it was noted that NO suppressed SARS-CoV replication through two different modes of action. NO or its derivatives decreased palmitoylation of nascently expressed spike (S) protein, which had an effect on the fusion of the S protein to its cognate receptor, ACE2. Second, it reduced viral RNA generation in the initial stages of viral replication, which could be due to an impact on one or both of the cysteine proteases encoded in Orf1a of SARS-CoV [58]. The effect of inhaled NO, pulmonary vasodilation is facilitated in part by elevated cellular cyclic guanidine monophosphate GMP (cGMP). The cGMP causes phosphorylation of the calcium channels thereby, increasing the uptake of Ca2+. This causes vasodilation and increased oxygen uptake by the lungs [59].
In the UK, SaNOtize, along with Ashford and St Peter's Hospitals NHS Foundation Trust and Berkshire and Surrey Pathology Services, showed that, in human phase II clinical trials, SaNOtize's nasal spray was an effective anti-viral therapy, which reduced COVID-19 spread, decreased its duration as well as severity of symptoms. In a randomized, double-blind, placebo-controlled phase II trial in 79 confirmed COVID-19 cases, SaNOtize's early therapy greatly reduced SARS-Cov-2 titers [60]. Patients who received treatment with the nasal spray experienced an overall viral log reduction of 1.362 in the initial 24 h, corresponding to a 95 percent reduction. The viral load declined by more than 99 percent within the first 72 h. There were no adverse effects reported in different studies that included 7000 participants investigating the self-administered medication. The spray can decrease infectivity—the transmission level from an infected individual to a non-infected person—in addition to delivering antiviral care in the initial phases of infection as well as for others, still to be vaccinated [61].
Hydroxypropyl methyl cellulose nasal spray
Another candidate explored for administration as the nasal spray is cellulose derivative—hydroxypropyl methylcellulose (HPMC), also known as hypromellose, which forms a mucoadhesive gel. As HPMC gets along nasal mucosa, it absorbs fluids and forms a micron-sized gel, coating the nasal cells, thereby barring viruses from interacting with receptors responsible for viral penetration into the cells.
In collaboration with the Israeli Ministry of Health and the Sheba Medical Center at Tel Hashomer Hospital, Nasus Pharma showed that their Taffix spray (containing HPMC) completely obstructed transmission of two SARS-CoV-2 alpha and beta variants [62]. Taffix also forms a local acidic (pH 3.5) microenvironment onto the mucosal surfaces which remains stable for up to 5 h, hence proving detrimental for virus survival, with little side effects to the host. Regulated clinical trials could be useful in the identification of more accurately target groups and methods to promote adherence. Given Taffix's excellent safety profile and considerable effectiveness to prevent infection following what is known as a high-risk infection event—it appears, this complementary layer of defence could play a role in lowering infection risks. According to the manufacturer, 83 worshipers made use of the spray before prayers and subsequently for the next 2 weeks. It was demonstrated that only two contracted the virus in a real-world evaluation of the medication. According to the study's surveys, those who contracted it, did not use the spray as directed or did not use the spray. Furthermore, in April 2022, a study sponsored by Chulalongkorn University tested HPMC-based nasal spray solution comprising human IgG1 anti-SARS-CoV-2 antibody cocktail in healthy volunteers. A phase 1 double-blind randomized clinical trial was carried out with great safety profile provided [63].
Polysaccharides-based nasal spray
It has been demonstrated that complex structural sulfated polysaccharides, which are present in large amounts in many species of marine algae, can prevent the replication of enveloped viruses. Compounds from red algae like phycocolloid carrageenan as well as sulfated polysaccharides derived from brown and green algae have been viewed as potential antivirals against SARS-COV-2 [64]. Iota-carrageenan-based nasal spray can suppress SARS-CoV-2 in vitro at levels as low as 6 μg/ml, according to Bansal et al. [65]. Grover et al. formulated a nasal spray containing gellan and λ-carrageenan. When tested for both prophylaxis and spreading prevention, spray systems showed extremely strong antiviral abilities that completely inhibited the virus [66]. Marino med Biotech engineered iota carrageenan a nasal spray formulation to suppress the coronavirus-2. It has been demonstrated to inactivate novel, rapidly spreading variants. In vitro testing showed that the compound was successful in combating the SARS-CoV-2 wild type and three variants identified as the British, South African, and Brazilian varieties. Carragelose, a sulfated polymer derived from the red seaweed, the company's recent discovery acts to create layer on the mucosa which coats invading viruses, making them inactive [67].
Nasal delivery of antibodies
Mucosal antibodies IgM and IgA serve as the first line of defence against infections that affect the mucous membranes. Additionally, IgM and IgA1 can be nebulized and inhaled to enter airway tissues. Ku et al. engineered six IgM antibodies based on the CR3022 monoclonal antibody and five IgG1 monoclonal antibodies to combat the resistance that immunoglobulin G (IgG)-based therapies experience. Thorough studies on IgM CoV2-14 (IgM-14) noted that IgM-14 outperformed IgG-14 in terms of binding, neutralization, and ACE2 blocking. In vivo biodistribution studies showed that IgM-14 was deposited primarily in the nasal cavity for more than 4 days following a single intranasal dose. The outcomes also demonstrated that nasally administered IgM-14 provided long residence duration and primarily targets the respiratory tract, thereby lowering viral load considerably [14]. IGM Biosciences developing engineered IgM antibodies, conducted a phase 1 human clinical trial in the US and South Africa with wither one or two dose regimens with safety profiles reported. [68].
Tiziana Life Sciences plc, a biotech company based in the UK, has accomplished a clinical trial (Phase 1) of Foralumab (nasal anti-CD3 human monoclonal antibody), in mild-to-moderately symptomatic COVID-19 patients in Brazil. Owing to its capability to confer systemic immunity through the respiratory or intestinal epithelium, Foralumab is the pioneer monoclonal antibody that can be administered through the nasal or oral route. The safety of nasal formulation was established in a study carried out in a joint venture with researchers from the Harvard Medical School and in trials [69].
Neurimmune, a Swiss antibody expert, and Ethris, a German RNA biotech, have developed inhaled messenger RNA (mRNA) antibodies which can combat the devastating respiratory consequences of COVID-19 [70]. Neurimmune AG is studying the immunoglobulin sequences of recovered COVID-19 patients, while Ethris focusses on employing a novel pulmonary therapeutic weapon to provide the same. The pulmonary SNIM®RNA technology produced by Ethris will assist in administering mRNA-encoded, neutralizing anti-SARS-CoV-2 antibodies straight into patients' lungs, thereby providing for the rapid achievement of desired pulmonary antibody titers. The collaboration will accelerate the advancement of this innovative drug to successfully combat the pandemic. The medicinal mRNA will be injected directly into the lungs of symptomatic patients using nanoparticle aerosols administered by nebulizers causing the lungs to release high levels of local antibodies that neutralize SARS-CoV-2 [71].
Nasal spray containing glucocorticoid
Glucocorticoid, ciclesonide is used in the maintenance of asthma in adults as well as juvenile patients aged 12 under brand name Alvesco (Covis Pharma, Luxembourg) in form of a pressurized metred dose inhaler (80 to 320 g ciclesonide/actuation). According to Matsuyama et al., ciclesonide may prevent SARS-CoV-2 genomic RNA replication by suppressing the viral endonuclease NSP15 [72]. According to Iwabuchi et al., ciclesonide inhalation was successful in treating three cases of COVID-19 pneumonia. USFDA recently accepted an Investigational New Drug proposal for a conducting phase 3 clinical trial to evaluate Alvesco (ciclesonide) for treating non-hospitalized, symptomatic COVID-19 patients (12 years and older) [73]. Similar trials involving ciclesonide are being conducted for the treatment of COVID-19 in various countries including Sweden, South Korea, Australia, the UK, the US, and Japan [74]. In a multicentre, randomized, double-blind, placebo-controlled trial including 400 patients, it was found that participants who received ciclesonide saw fewer subsequent emergency department visits or hospitalizations for COVID-19-related conditions [75].
Ivermectin nasal spray
Ivermectin (macrolide lactone) has been used for tropical diseases including helminthiases and scabies. Experimentally, the drug has also shown antimalarial, anti-viral and antibacterial activity. Caly et al. showed that employing high concentrations of Ivermectin in the range of 2.5–5 M, inhibits SARS-CoV-2 multiplication in vitro [76]. Ivermectin inhibits in vitro replication of SARS-CoV-2, and shows 5000-fold decrease in SARS-CoV-2 viral RNA within 2 days. It also docks in the region of Leucine 91 of the spike and Histidine 378 of SARS-Co2-ACE2 complex, hindering binding to human cell membrane [77]. In addition, data from a randomized clinical trial on its antiviral efficacy in SARS-CoV-2-infected individuals are currently available. As such, in a study by Erreclade et al., it was noted that Ivermectin in high concentrations could suppress SARS-CoV-2 replication. It was reported that when administered in the form of a nasal spray, Ivermectin could achieve high concentrations in nasopharyngeal tissues [78]. In a pig model, the spray was proven to be safe as well as well tolerated, without any significant adverse effects [79].
Astodrimer sodium 1% nasal spray
Astodrimer sodium, a highly branched dendrimer exhibits considerable antiviral as well as virucidal activity in vitro against different strains of SARS-CoV-2. Astodrimer sodium nasal spray was reported to inhibit or diminish SARS-CoV-2 replication and its consequences in K18-hACE2 mice by Paul et al. [56].
Mometasone Furoate nasal spray
One of COVID-19's most prevalent and early symptoms is olfactory impairment [80]. Mometasone Furoate nasal spray was studied on 80 patients having severe microsomia or anosmia by Kasiri et al. to determine how effectively it assisted patients recover from severe microsomia or anosmia spurred on by COVID-19 [81].
The outcomes showed that severe chronic anosmia as measured by COVID-19 improved more quickly when Mometasone Furoate nasal spray was combined with olfactory training. In yet another study, it was demonstrated that the frequency of anosmia was reduced by 22.9% when compared to the control group [82].
Chlorpheniramine maleate nasal spray
Chlorpheniramine is a powerful antiviral antihistamine that is both safe and efficient against different influenza A/B strains.According to the evidence, intranasal administration exhibits high efficacy and no side effects. Chlorpheniramine maleate was investigated for its virucidal properties in a nasal spray formulation by Xu et al. [83]. The virucidal activity of the same was examined by employing SARS-CoV-2 viral stocks (USA-WA1/2020 strain) in Vero 76 infected cells. The study exhibited that nasal spray exhibited powerful virucidal activity against SARS-CoV-2 [122]. In a case series provided by Torres et al. [84], it was shown that patients with low to moderate COVID-19 morbidity and mortality risk experienced a considerable improvement in their symptoms and a 50% step down in the clinical course when using Chlorpheniramine nasal spray.
PH94B nasal spray
The PH94B is a synthetic investigational neurosteroid produced from pherines. VistaGen Therapeutics, Inc. in the US tailored the neuroactive nasal spray. PH94B adheres to nasal chemosensory receptors, thereby triggering synaptic pathways in the central nervous system which curb anxiety related to daily social environments and other repetitive situations [85]. In phase 2 and phase 3 clinical trials, efficacy of the PH94B nasal spray (8 g) in the emergency management of social anxiety was established. Based on this, VistaGen Therapeutics, Inc. initiated a phase 2a review of PH94B nasal spray for the treatment of COVID-19 connected anxiety [86]. The spray was found effective without any side effects [87]. Nasal sprays for treatment of SARS-CoV-2 are summarized in Table 2.
Nasal platform for pediatric COVID-19 management
The epidemiology and clinical presentation of the effect of SARS-CoV-2 in the pediatric population indicate different effects as compared to adults. Although COVID-19 seems to affect children infrequently with mild effects but may cause serious complications, which can include pediatric inflammatory multisystem syndrome (PIMS-TS) [94]. One of the reasons for less frequency of cases in children could be stronger immunity owing to exposure to other corona virus infections or other respiratory viral pathogens in the past [95]. There are currently no proven disease-specific treatments available for children. However, two vaccines have been given emergency use authorization by the US Food and Drug Administration. Apart from that, a number of other vaccines are under evaluation or phase-III clinical trial testing [96]. Intravenous access could be challenging owing to hesitancy by children [97]. Needle-less delivery could be regarded as a better alternative for children. The nasal route can be employed for disease management in children. Intranasal administration of analgesics, anxiolytics, and anticonvulsants has been effectively achieved in children. Not many side effects of nasal medications have been reported [98].
As per the reports by the National Institute of Allergy and Infectious Disease, researchers have developed a candidate COVID-19 vaccine for infants and young children requiring only a single dose delivery through nasal spray.
Safety and ethical considerations
The nasal route can have an upper edge over traditional delivery methods, yet sufficient clinical data must be gathered for the practical use of nasal sprays. An adequate safety profile must be established for the realization of potential benefits of the nasal spray in the mass population. Appropriate strategies should be implemented for better coverage. It is crucial to determine how prophylactic or therapeutic agents and adjuvants interact to influence immune response [48]. As with conventional vaccines, the risk of vaccine-induced disease enhancement also exists for nasal vaccines. Long-term surveillance data are important to ensure that uncommon occurrences or side effects could be conquered following the use of nasal spray therapy [99]. For products that have received emergency use authorizations, rigorous follow-up becomes necessary to detect rare events, if any. A proper follow-up system should be established for evaluating the safety profile of the licensed products also. Ignorance and lack of adherence to safety protocols can increase the risk of infection in the workplace. Improper handling or contact between the nasal delivery device's tip and the patient's nasal cavity may cause contamination to spread into the nasal spray tip, thereby compromising safety [100]. While administering inhalation therapy, exposure of the healthcare workers to the patient's exhaled aerosols is a serious concern [46].
Various excipients like absorption enhancers, and preservatives are used in nasal formulations. However, some of the excipients have been known to be harmful to the nasal epithelium. They may affect the ciliary function and mucociliary clearance. Thus, adequate safety data should be collected for the excipients to be used in the formulation [101].
The ongoing clinical trials may not address a number of significant issues, including the adverse effects of the therapies and the impact on virus transmission to healthcare professionals [102]. Children and expectant mothers should receive additional consideration while establishing a safety profile. The regulations call for enhanced protection standards to be implemented to children participating in clinical trials [103].
Efficacy evaluation of nasal vaccines
The efficacy of vaccines is evaluated in phase 3 of clinical trials. For evaluation of vaccine efficacy, blood or nasal sample is collected from the infected person after 14–28 days of administration. Effective drug delivery into the nasal cavity depends on a sufficient dose being applied to the nasal mucosa and its ability to remain localized to the site of activity.
Frank et al. investigated the virucidal activity of a nasal spray using povidone-iodine as an active drug against the SARS-CoV-2 virus. With as much low as 1.25% concentration of povidone-iodine, he observed efficient viral inactivation within 15 s of contact. The spray forms a protective barrier for up to 4 h while also lowering viral titers and increasing viral clearance [104, 105]. Assessed the efficacy of an adenovirus type 5 vectored vaccine against SARS-CoV-2 in mice and reported that a single nasal spray dose had a significant systemic and site-specific immune response. A significant response was observed to the simultaneous release of serum neutralizing antibodies, mucosal antibodies (IgA), as well as CD4 + and CD8 + T cells. Sun et al. evaluated the immunogenicity, safety, and effectiveness of a Newcastle disease virus, viral vector-based vaccine against SARS-CoV-2 in mice and hamsters. It was shown that following intranasal administration, high levels of anti-SARS-CoV-2 specific IgA and IgG2a antibodies along with T cell-mediated immunity were induced [106].
In a small-scale clinical experiment, Lin and researchers investigated the effectiveness of a 35B5-based nasal spray in protecting against SARS-CoV-2 variants. It was demonstrated that the samples of nasal mucosa collected in a time of 24 h following the application of nasal spray successfully neutralized SARS-CoV-2 variants (including Delta and Omicron). At 48 and 72 h after nasal spray, the protective effectiveness was 60% and 20%, respectively. They concluded that a nasal spray of the 35B5 formulation provides excellent 24-h protection from SARS-CoV-2 variations, such as the alpha, beta, delta, or omicron forms [107].
Comparison of nasal and vascular vaccination
COVID-19 intranasal vaccines have demonstrated the ability to produce a significant antibody-mediated as cell-mediated immunity. In addition, they have the potential to induce mucosal immunity. By inducing the secretion of IgA antibody response especially in nasal cavity, the intranasal SARS-CoV-2 vaccine prevents viral infestation, reproduction, shedding as well as the spread of disease and virus transmission. Having significant vascularity in the muscles, the intramuscular vaccines get into systemic circulation quickly. Vascular vaccines induce systemic immunity. However, vaccine redistribution and transfection in tissues beyond the injection site, can lead to rare adverse effects including autoimmune reactions. It has been recently signified that administration of vaccine via intramuscular route and distribution through systemic circulation can lead to platelets–adenoviral vector interaction, platelets conglomeration and activation. Intranasal vaccines allow for a lower dose as compared to intramuscular administration. Intranasal vaccines would be preferred over vascular vaccines, especially by the younger population. Intranasal vaccinations can be self-administered, thereby reducing the burden for immunization programs. Unlike intravenous routes, they would not require sterilized settings. Intranasal vaccines can be designed to store at room temperature, which is not possible for vascular vaccines [108].
Drug product delivery and device development
Despite the apparent benefits of intranasal drug delivery, the nasal cavity can fall victim to limitations like low permeability for certain drugs including hydrophilic molecules, peptides, proteins, and nucleotides, accelerated mucociliary clearance, and biodegradation [109]. Drug delivery and device development are vital for the design of efficient and reliable intranasal medications. Three keys cooperate governing the delivery of drugs through nasal route that are: the drug, the delivery vehicle, and the administration tool, i.e., device. Low-molecular-weight drugs (below 300 Da) can easily pass through aqueous channels of the nasal membrane while for high-molecular-weight drugs, the rate of permeation is significant, which is attributed to the physiochemical nature of drugs. Nasal mucosa being lipophilic in nature, it allows for better permeation of lipophilic drugs. Hydrophilic drugs can be administered in the form of a prodrug [110]. Passive diffusion absorbs nasal secretions being watery in nature, hydrophilic drugs, while lipophilic drugs tend to get absorbed through active absorption. Chirality can affect the absorption of drug through the nasal mucosa; hence, consideration should be given while selecting the isomer [111]. Peptides and proteins can undergo enzymatic degradation while crossing the epithelial layer, thereby presenting low bioavailability. Enzymatic degradation can be avoided using protective shells like micelles, and liposomes or employing enzyme inhibitors [112]. Viscous delivery vehicle prolongs the contact time of the drug with nasal mucosa which increases permeation time. pH of the formulation should be adjusted between 4.5 and 6.5, to avoid nasal irritation. Also at acidic pH, lysozymes are activated, which destroy the bacteria [88]. A nasal absorption enhancer would be required for the nasal distribution of hydrophilic or high-molecular-weight medications in order for the drug to pass the nasal membrane in an amount adequate for therapeutic use. CPE-215®, Intravail®, ChiSysTM, PecSysTM, and CriticalSorbTM are examples of the absorption enhancer and modulator that are currently being developed commercially for a variety of drugs by CPEX Pharma, Aegis Therapeutics, Archimedes Pharma Ltd., and Critical Pharmaceuticals Ltd, respectively [113]. Innovative strategies to create efficient nasal delivery systems for specific active ingredients are currently in different phases of research and development. New nasal improved delivery technologies, vehicles made to prevent drug catabolism by mucosal enzymes, and modulation are a few of these.
Device for drug delivery
Numerous devices are available for nasal drug delivery. The device should be able to deliver different dosage forms since the formulation to be delivered can be powder, liquid or in aerosol form [114]. Nasal drug delivery systems operate best when spray properties, mucociliary clearance, deposition, dissolution, and absorption are taken into account. Devices for drug delivery can influence these parameters. Devices should be uncomplicated to limit failure modes, but for benefits like increased absorption, tailored deposition, etc., advanced technology becomes crucial [112]. Nasal delivery devices and their mechanisms should be arranged in such a way that protects the lungs and nasal route from various hazardous exposures [115]. Some of the devices and their characteristics have been depicted in Table 3.
The future of nasal delivery concepts
To date, powders, sprays, drops, gels, and other forms of administration into the nasal cavity have been developed. Novel formulations include mucoadhesive solutions, microparticles, liposomes, nasal inserts, thermosensitive and pH-sensitive nasal gels, micelles, etc. The major goals of nasal medication delivery systems are to enhance nasal epithelial permeability and contact period at the site of absorption. Several techniques are utilized to improve intranasal absorption, including changes to the mucus layer, tight junctions, reversed micelle production, extraction by co-micellization, and the utilization of surfactants and enzyme inhibitors. Recently, bio adhesives are being widely employed to prolong contact time at the site of absorption. The efficacy of multilamellar micelles and liposomal micelle formulations has also been studied. Nasal inserts are formulated through lyophilization or gasification. They can release the active ingredient in a controlled manner. Various delivery devices are there for intranasal administration. Metered dose inhalers, nebulizers, etc., are available. For systemic drugs and vaccines, a unique delivery concept was put forth by a Norwegian company. To prevent the deposition of small particles in lungs, they developed a bi-directional delivery device [121].
Concluding note
COVID-19 pandemic has affected people in almost all regions of the world. Different research organizations and health agencies have been working on the development of vaccinations and specific treatments against SARS-CoV-2. Despite the fact that several vaccines have now been approved for use against COVID-19, they suffer from drawbacks such as vaccine reluctance among individuals, wastage of doses due to their short shelf life as well as lack of a proper distribution system. The requirement for freeze drying of vaccines poses a logistical challenge. Again, the intramuscular route, being an invasive technique, hesitancy is noted among individuals. Moreover, not much sufficient data exist for establishing safety among pregnant women and small children. As far as treatment is concerned, still there is a lack of specific treatment. Immunization and treatment through parenteral route and oral routes can produce only systemic effect. In light of this, if nasal sprays are taken into consideration, they can combat the virus at the entry point itself, significantly decreasing the transmission to deeper areas. Needle-less administration may lead to less hesitancy among children. A number of nasal vaccines as well as nasal sprays for treatment are under clinical trials. Nasal sprays can be viewed as a promising alternative for curbing COVID-19. Prospects for the future include integrating in vivo data with clinical results. Steps in this direction have already been initiated as evident from the fact that number of nasal sprays are under clinical trial and a couple of them have received emergency use authorization. The multiple ongoing initiatives will definitely open the door for alternate approaches for the prevention and treatment of COVID-2. Parenteral vaccination along with nasal therapy could aid in achieving the ultimate goal of eliminating the virus.
Data availability
Not applicable.
Abbreviations
- ACE2:
-
Angiotensin converting enzyme 2
- CD4:
-
Clusters of differentiation 4
- cGMP:
-
Guanosine mono phosphate
- COVID-19:
-
Coronavirus disease-2019
- HCoV:
-
Human coronavirus
- HPMC:
-
Hydroxypropyl methyl cellulose
- IgG:
-
Immunoglobulin G
- IL-2:
-
Interleukin-2
- MERS-CoV:
-
Middle East respiratory syndrome coronavirus
- mRNA:
-
Messenger ribonucleic acid
- NC:
-
Nasal cycle
- NONS:
-
Nitric oxide nasal spray
- RNA:
-
Ribonucleic acid
- SARS-CoV-2:
-
Severe acute respiratory syndrome coronavirus disease 2
- URTI:
-
Upper respiratory tract infection
References
Ciotti M, Ciccozzi M, Terrinoni A, Jiang W-C, Wang C-B, Bernardini S. The COVID-19 pandemic. Crit Rev Clin Lab Sci. 2020;57:365–88. https://doi.org/10.1080/10408363.2020.1783198.
Hasöksüz M, Kilic S, Saraç F. Coronaviruses and sars-cov-2. Turkish Journal of Medical Sciences. 2020;50:549–56.
Peiris JSM. Coronaviruses. Medical Microbiology 2012:587–93. https://doi.org/10.1016/B978-0-7020-4089-4.00072-X.
Fehr AR, Perlman S, Maier HJ, Bickerton E, Britton P. An overview of their replication and pathogenesis; genomic organization. Methods Mol Biol. 2015;1282:1–23.
Li Q, Wu J, Nie J, Zhang L, Hao H, Liu S, et al. The impact of mutations in SARS-CoV-2 spike on viral infectivity and antigenicity. Cell. 2020;182:1284–94.
Fong SJ, Dey N, Chaki J. An Introduction to COVID-19. Artif Intell Cor Outbreak. 2020. https://doi.org/10.1007/978-981-15-5936-5_1.
Kashte S, Gulbake A, El-Amin Iii SF, Gupta A. COVID-19 vaccines: rapid development, implications, challenges and future prospects. Hum Cell. 2021;34:711–33. https://doi.org/10.1007/s13577-021-00512-4.
Dai T, Song J-S. Transforming COVID-19 vaccines into vaccination : challenges and opportunities for management scientists. Health Care Manag Sci. 2021;24:455–9. https://doi.org/10.1007/s10729-021-09563-3.
Ayenigbara IO, Adegboro JS, Ayenigbara GO, Adeleke OR, Olofintuyi OO. The challenges to a successful COVID-19 vaccination programme in Africa. Germs 2021:427–40.
Yigit M, Ozkaya-Parlakay A, Senel E. Evaluation of COVID-19 vaccine refusal in parents. Pediatr Infect Dis J. 2021;40:e134–6. https://doi.org/10.1097/INF.0000000000003042.
Tagoe ET, Sheikh N, Morton A, Nonvignon J, Sarker AR, Williams L, et al. COVID-19 vaccination in lower-middle income countries: national stakeholder views on challenges, barriers, and potential solutions. Front Public Health. 2021. https://doi.org/10.3389/fpubh.2021.709127.
Alam ST, Ahmed S, Ali SM, Sarker S, Kabir G, Ul-Islam A. Challenges to COVID-19 vaccine supply chain: implications for sustainable development goals. Int J Prod Econ. 2021. https://doi.org/10.1016/j.ijpe.2021.108193.
Meister TL, Todt D, Brüggemann Y, Steinmann J, Banava S, Brill FHH, et al. Virucidal activity of nasal sprays against severe acute respiratory syndrome coronavirus-2. J Hosp Infect. 2022;120:9–13. https://doi.org/10.1016/j.jhin.2021.10.019.
Ku Z, Xie X, Hinton PR, Liu X, Ye X, Muruato AE, et al. Nasal delivery of an IgM offers broad protection from SARS-CoV-2 variants. Nature. 2021;595:718–23.
Pujadas E, Chaudhry F, McBride R, Richter F, Zhao S, Wajnberg A, et al. SARS-CoV-2 viral load predicts COVID-19 mortality. Lancet Respir Med. 2020;8: e70.
Pilicheva B, Boyuklieva R. Can the nasal cavity help tackle COVID-19? Pharmaceutics. 2021;13:1612.
Zuercher AW, Coffin SE, Thurnheer MC, Fundova P, Cebra JJ. Nasal-associated lymphoid tissue is a mucosal inductive site for virus-specific humoral and cellular immune responses. J Immunol. 2002;168:1796–803.
Kiyono H, Fukuyama S. NALT-versus Peyer’s-patch-mediated mucosal immunity. Nat Rev Immunol. 2004;4:699–710.
Corr SC, Gahan CCGM, Hill C. M-cells: origin, morphology and role in mucosal immunity and microbial pathogenesis. FEMS Immunol Med Microbiol. 2008;52:2–12.
Fujimura Y. Evidence of M cells as portals of entry for antigens in the nasopharyngeal lymphoid tissue of humans. Virchows Arch. 2000;436:560–6.
Suman JD. Nasal drug delivery. Expert Opin Biol Ther. 2003;3:519–23.
Iwasaki A. Exploiting mucosal immunity for antiviral vaccines. Annu Rev Immunol. 2016;34:575–608.
DeFrancesco L. COVID-19 antibodies on trial. Nat Biotechnol. 2020;38:1242–52.
Weinreich DM, Sivapalasingam S, Norton T, Ali S, Gao H, Bhore R, et al. REGN-COV2, a neutralizing antibody cocktail, in outpatients with Covid-19. N Engl J Med. 2021;384:238–51.
Hou YJ, Okuda K, Edwards CE, Martinez DR, Asakura T, Dinnon KH III, et al. SARS-CoV-2 reverse genetics reveals a variable infection gradient in the respiratory tract. Cell. 2020;182:429–46.
Birkhoff M, Leitz M, Marx D. Advantages of intranasal vaccination and considerations on device selection. Indian J Pharm Sci. 2009;71:729.
Siddiqui R, Khan NA. Proposed intranasal route for drug administration in the management of central nervous system manifestations of COVID-19. ACS Chem Neurosci. 2020;11:1523–4.
Bellussi L, Cambi J, Passali D. Functional maturation of nasal mucosa: role of secretory immunoglobulin A (SIgA). Multidiscip Respir Med. 2013;8:46. https://doi.org/10.1186/2049-6958-8-46.
Kilian M, Reinholdt J, Mortensen SB, Sørensen CH. Perturbation of mucosal immune defence mechanisms by bacterial IgA proteases. Bull Eur Physiopathol Respir. 1983;19:99–104.
Kurono Y, Fujiyoshi T, Mogi G. Secretory IgA and bacterial adherence to nasal mucosal cells. Ann Otol Rhinol Laryngol. 1989;98:273–7. https://doi.org/10.1177/000348948909800407.
Wang Z, Lorenzi JCC, Muecksch F, Finkin S, Viant C, Gaebler C, et al. Enhanced SARS-CoV-2 neutralization by dimeric IgA. Sci Translat Med. 2021;13:1555.
Hoffmann M, Kleine-Weber H, Schroeder S, Krüger N, Herrler T, Erichsen S, et al. SARS-CoV-2 cell entry depends on ACE2 and TMPRSS2 and is blocked by a clinically proven protease inhibitor. Cell. 2020;181:271–80.
Lu R, Zhao X, Li J, Niu P, Yang B, Wu H, et al. Genomic characterisation and epidemiology of 2019 novel coronavirus: implications for virus origins and receptor binding. The Lancet. 2020;395:565–74.
Wrapp D, Wang N, Corbett KS, Goldsmith JA, Hsieh C-L, Abiona O, et al. Cryo-EM structure of the 2019-nCoV spike in the prefusion conformation. Science. 2020;367:1260–3.
Lan J, Ge J, Yu J, Shan S, Zhou H, Fan S, et al. Structure of the SARS-CoV-2 spike receptor-binding domain bound to the ACE2 receptor. Nature. 2020;581:215–20.
Hassan AO, Kafai NM, Dmitriev IP, Fox JM, Smith BK, Harvey IB, et al. A single-dose intranasal ChAd vaccine protects upper and lower respiratory tracts against SARS-CoV-2. Cell. 2020;183:169–84.
Czop JK, McGowan SE, Center DM. Opsonin-independent phagocytosis by human alveolar macrophages: augmentation by human plasma fibronectin. Am Rev Respir Dis. 1982;125:607–9.
Jonsson S, Musher DM, Goree A, Clinton LE. Human alveolar lining material and antibacterial defenses. Am Rev Respir Dis. 1986;133:136–40.
Coonrod JD. The role of extracellular bactericidal factors in pulmonary host defense. Semin Respir Infect. 1986;1:118–29.
Reynolds HY, Kazmierowski JA, Newball HH. Specificity of opsonic antibodies to enhance phagocytosis of Pseudomonas aeruginosa by human alveolar macrophages. J Clin Investig. 1975;56:376–85.
Hanif J, Jawad SSM, Eccles R. The nasal cycle in health and disease. Clin Otolaryngol Allied Sci. 2000;25:461–7.
Mygind N, Dahl R. Anatomy, physiology and function of the nasal cavities in health and disease. Adv Drug Deliv Rev. 1998;29:3–12.
Pendolino AL, Lund VJ, Nardello E, Ottaviano G. The nasal cycle: a comprehensive review. Rhinol Onl. 2018;1:67–76.
Papadopoulos NG, Guibas GV. Rhinitis subtypes, endotypes, and definitions. Immunol Aller Clinics. 2016;36:215–33.
Chavda VP, Vora LK, Pandya AK, Patravale VB. Intranasal vaccines for SARS-CoV-2: from challenges to potential in COVID-19 management. Drug Discovery Today. 2021;26:2619–36. https://doi.org/10.1016/j.drudis.2021.07.021.
Xi J, Lei LR, Zouzas W, April SX. Nasally inhaled therapeutics and vaccination for COVID-19: developments and challenges. MedComm. 2021;2:569–86. https://doi.org/10.1002/mco2.101.
Silen W, Machen TE, Forte JG. Acid-base balance in amphibian gastric mucosa. Am J Physiol. 1975;229:721–30. https://doi.org/10.1152/ajplegacy.1975.229.3.721.
Ehrhart IC, Parker PE, Weidner WJ, Dabney JM, Scott JB, Haddy FJ. Coronary vascular and myocardial responses to carotid body stimulation in the dog. Am J Physiol. 1975;229:754–60. https://doi.org/10.1152/ajplegacy.1975.229.3.754.
Smith A, Perelman M, Hinchcliffe M. Chitosan: a promising safe and immune-enhancing adjuvant for intranasal vaccines. Hum Vaccin Immunother. 2014;10:797–807. https://doi.org/10.4161/hv.27449.
de Apostólico JS, Lunardelli VAS, Coirada FC, Boscardin SB, Rosa DS. Adjuvants: classification, modus operandi, and licensing. J Immunol Res. 2016. https://doi.org/10.1155/2016/1459394.
Xiang S, Fu J, Ye K, Zheng Y, Zhu X, Chen J, et al. Effect of Lactobacillus gasseri PA3 on gut microbiota in an in vitro colonic simulation. Food Sci Nutr. 2019;7:3883–91. https://doi.org/10.1002/fsn3.1236.
Covid-19 Vaccine Tracker: Latest Updates - The New York Times n.d. https://www.nytimes.com/interactive/2020/science/coronavirus-vaccine-tracker.html (accessed October 29, 2022).
Castellarnau A, Heery GP, Seta A, Luscombe CA, Kinghorn GR, Button P, et al. Astodrimer sodium antiviral nasal spray for reducing respiratory infections is safe and well tolerated in a randomized controlled trial. Sci Rep. 2022;12:10210. https://doi.org/10.1038/s41598-022-14601-3.
Durbin RP. Letter: acid secretion by gastric mucous membrane. Am J Physiol. 1975;229:1726. https://doi.org/10.1152/ajplegacy.1975.229.6.1726.
Ricciardolo FLM, Bertolini F, Carriero V, Högman M. Nitric oxide’s physiologic effects and potential as a therapeutic agent against COVID-19. J Breath Res. 2020. https://doi.org/10.1088/1752-7163/abc302.
Paull JRA, Luscombe CA, Castellarnau A, Heery GP, Bobardt MD, Gallay PA. Protective effects of astodrimer sodium 1% nasal spray formulation against SARS-CoV-2 nasal challenge in K18-hACE2 mice. Viruses. 2021;13:1656. https://doi.org/10.3390/v13081656.
Mitchell JP, Berlinski A, Canisius S, Cipolla D, Dolovich MB, Gonda I, et al. Urgent appeal from international society for aerosols in medicine (ISAM) during COVID-19: clinical decision makers and governmental agencies should consider the inhaled route of administration: a statement from the ISAM regulatory and standardization issues networking group. J Aerosol Med Pulm Drug Deliv. 2020;33:235–8. https://doi.org/10.1089/jamp.2020.1622.
Åkerström S, Gunalan V, Keng CT, Tan Y-J, Mirazimi A. Dual effect of nitric oxide on SARS-CoV replication: viral RNA production and palmitoylation of the S protein are affected. Virology. 2009;395:1–9. https://doi.org/10.1016/j.virol.2009.09.007.
Mekler LB. On the problem of oncogene of tumour viruses. Acta Virol. 1975;19:501–8.
UK Clinical Trial Confirms SaNOtize’s Breakthrough Treatment for COVID-19 2021. https://www.businesswire.com/news/home/20210315005197/en/UK-Clinical-Trial-Confirms-SaNOtize%E2%80%99s-Breakthrough-Treatment-for-COVID-19 (accessed October 29, 2022).
Regev-Shoshani G, Vimalanathan S, McMullin B, Road J, Av-Gay Y, Miller C. Gaseous nitric oxide reduces influenza infectivity in vitro. Nitric Oxide. 2013;31:48–53. https://doi.org/10.1016/j.niox.2013.03.007.
Shmuel K, Dalia M, Tair L, Yaakov N. Low pH Hypromellose (Taffix) nasal powder spray could reduce SARS-CoV-2 infection rate post mass-gathering event at a highly endemic community: an observational prospective open label user survey. Expert Rev Anti Infect Ther. 2021;19:1325–30. https://doi.org/10.1080/14787210.2021.1908127.
Chulalongkorn University. A Phase I Double-blind, Randomized, Placebo-controlled Study to Evaluate Safety of Hypromellose-based Nasal Spray Solution Containing Human IgG1 Anti-SARS-CoV-2 Antibody Cocktail in Healthy Volunteers. clinicaltrials.gov; 2022.
Pereira L, Critchley AT. The COVID 19 novel coronavirus pandemic 2020: seaweeds to the rescue? Why does substantial, supporting research about the antiviral properties of seaweed polysaccharides seem to go unrecognized by the pharmaceutical community in these desperate times? J Appl Phycol. 2020;32:1875–7. https://doi.org/10.1007/s10811-020-02143-y.
Bansal S, Jonsson CB, Taylor SL, Figueroa JM, Dugour AV, Palacios C, et al. Iota-carrageenan and xylitol inhibit SARS-CoV-2 in Vero cell culture. PLoS ONE. 2021. https://doi.org/10.1371/journal.pone.0259943.
Moakes RJA, Davies SP, Stamataki Z, Grover LM. Formulation of a composite nasal spray enabling enhanced surface coverage and prophylaxis of SARS-COV-2. Adv Mater. 2021;33:2008304. https://doi.org/10.1002/adma.202008304.
Eva Prieschl-Grassauer. Nasal spray works against COVID-19 variants. 21–04–2021 2021. https://www.thepharmaletter.com/article/nasal-spray-works-against-covid-19-variants? (Accessed April 25, 2021).
Zhang H, Yang Z, Xiang J, Cui Z, Liu J, Liu C. Intranasal administration of SARS-CoV-2 neutralizing human antibody prevents infection in mice. Bioengineering. 2020. https://doi.org/10.1101/2020.12.08.416677.
Moreira TG, Matos KTF, De Paula GS, Santana TMM, Da Mata RG, Pansera FC, et al. Corrigendum: nasal administration of anti-CD3 monoclonal antibody (foralumab) reduces lung inflammation and blood inflammatory biomarkers in mild to moderate COVID-19 patients: a pilot study. Front Immunol. 2022. https://doi.org/10.3389/fimmu.2021.815812.
Dr. Fabian Buller. Neurimmune and Ethris Sign Collaboration Agreement to Rapidly Develop Inhaled mRNA-based Antibody Therapy for the Treatment of Covid-19. Neurimmune AG 2020. https://www.neurimmune.com/news/neurimmune-and-ethris-sign-collaboration-agreement-to-rapidly-develop-inhaled-mrna-based-antibody-therapy-for-the-treatment-of-covid-19 (accessed April 25, 2021).
Chakraverty A. Swiss and German Team to Develop Inhaled mRNA Coronavirus Treatment. LabiotechEu 2020. https://www.labiotech.eu/trends-news/ethris-neurimmune-mrna-coronavirus/ (accessed October 29, 2022).
Matsuyama S, Kawase M, Nao N, Shirato K, Ujike M, Kamitani W, et al. The inhaled steroid ciclesonide blocks SARS-CoV-2 RNA replication by targeting the viral replication-transcription complex in cultured cells. J Virol. 2020;95:e01648-e1720. https://doi.org/10.1128/JVI.01648-20.
Iwabuchi K, Yoshie K, Kurakami Y, Takahashi K, Kato Y, Morishima T. Therapeutic potential of ciclesonide inhalation for COVID-19 pneumonia: report of three cases. J Infect Chemother. 2020;26:625–32. https://doi.org/10.1016/j.jiac.2020.04.007.
Covis Pharma. Covis Pharma B.V. Initiates Phase 3 Clinical Trial of Alvesco (Ciclesonide) Inhaler for the Treatment of COVID-19. Prnewswire 2020. https://www.prnewswire.com/news-releases/covis-pharma-bv-initiates-phase-3-clinical-trial-of-alvesco-ciclesonide-inhaler-for-the-treatment-of-covid-19-301061105.html (accessed April 25, 2021).
Covis Pharma S.à.r.l. A Phase 3, Multicenter, Randomized, Double-Blind, Placebo-Controlled Study to Assess the Safety and Efficacy of Ciclesonide Metered-Dose Inhaler in Non-hospitalized Patients 12 Years of Age and Older With Symptomatic COVID-19 Infection. clinicaltrials.gov; 2022.
Caly L, Druce JD, Catton MG, Jans DA, Wagstaff KM. The FDA-approved drug ivermectin inhibits the replication of SARS-CoV-2 in vitro. Antiviral Res. 2020. https://doi.org/10.1016/j.antiviral.2020.104787.
Lehrer S, Rheinstein PH. Ivermectin Docks to the SARS-CoV-2 Spike Receptor-binding Domain Attached to ACE2. In Vivo 2020 https://doi.org/10.21873/invivo.12134.
Errecalde J, Lifschitz A, Vecchioli G, Ceballos L, Errecalde F, Ballent M, et al. Safety and pharmacokinetic assessments of a novel ivermectin nasal spray formulation in a pig model. J Pharm Sci. 2021;110:2501–7. https://doi.org/10.1016/j.xphs.2021.01.017.
Kashkooli L, Rozema D, Espejo-Ramirez L, Lasko P, Fagotto F. Ectoderm to mesoderm transition by down-regulation of actomyosin contractility. PLoS Biol. 2021. https://doi.org/10.1371/journal.pbio.3001060.
Huart C, Philpott C, Konstantinidis I, Altundag A, Whitcroft KL, Trecca EMC, et al. Comparison of COVID-19 and common cold chemosensory dysfunction. Rhin. 2020;58:623–5. https://doi.org/10.4193/Rhin20.251.
Kasiri H, Rouhani N, Salehifar E, Ghazaeian M, Fallah S. Mometasone furoate nasal spray in the treatment of patients with COVID-19 olfactory dysfunction: a randomized, double blind clinical trial. Int Immunopharmacol. 2021. https://doi.org/10.1016/j.intimp.2021.107871.
Hosseinpoor M, Kabiri M, Rajati Haghi M, Ghadam Soltani T, Rezaei A, Faghfouri A, et al. Intranasal corticosteroid treatment on recovery of long-term olfactory dysfunction due to COVID-19. Laryngoscope. 2022;132:2209–16. https://doi.org/10.1002/lary.30353.
Xu W, Xia S, Pu J, Wang Q, Li P, Lu L, et al. The antihistamine drugs carbinoxamine maleate and chlorpheniramine maleate exhibit potent antiviral activity against a broad spectrum of influenza viruses. Front Microbiol. 2018;9:2643. https://doi.org/10.3389/fmicb.2018.02643.
Torres J, Go CC, Chohan FA, L. GC, Sanchez-Gonzalez MA, Ferrer G. Chlorpheniramine maleate nasal spray in COVID-19 patients: Case Series. In Review 2021 https://doi.org/10.21203/rs.3.rs-138252/v1.
Michael R. Liebowitz,Ester Salman,Humberto Nicolini NR. Effect of an Acute Intranasal Aerosol Dose of PH94B on Social and Performance Anxiety in Women With Social Anxiety Disorder. Am J Psychiatry 2014;171.
VistaGen Therapeutics Inc. PH94B in the treatment of adjustment disorder with anxiety. May 27, 2020 2020. https://clinicaltrials.gov/ct2/show/NCT04404192 (accessed April 25, 2021).
Liebowitz MR, Salman E, Nicolini H, Rosenthal N, Hanover R, Monti L. Effect of an acute intranasal aerosol dose of PH94B on social and performance anxiety in women with social anxiety disorder. AJP. 2014;171:675–82. https://doi.org/10.1176/appi.ajp.2014.12101342.
Winchester S, John S, Jabbar K, John I. Clinical efficacy of nitric oxide nasal spray (NONS) for the treatment of mild COVID-19 infection. J Infect. 2021;83:237–79. https://doi.org/10.1016/j.jinf.2021.05.009.
Lo JB, Cruz ET. Efficacy of Carragelose® nasal spray impregnated versus mupirocin ointment impregnated nasal packs on mucosal healing after endoscopic sinus surgery: a double-blind, non-randomized, right-left side comparison. Philipp J Otolaryngol Head Neck Surg. 2020;35:11.
Ku Z, Xie X, Davidson E, Ye X, Su H, Menachery VD, et al. Molecular determinants and mechanism for antibody cocktail preventing SARS-CoV-2 escape. Nat Commun. 2021;12:469. https://doi.org/10.1038/s41467-020-20789-7.
Winkler ES, Bailey AL, Kafai NM, Nair S, McCune BT, Yu J, et al. SARS-CoV-2 infection of human ACE2-transgenic mice causes severe lung inflammation and impaired function. Nat Immunol. 2020;21:1327–35. https://doi.org/10.1038/s41590-020-0778-2.
Vaira LA, Hopkins C, Sandison A, Manca A, Machouchas N, Turilli D, et al. Olfactory epithelium histopathological findings in long-term coronavirus disease 2019 related anosmia. J Laryngol Otol. 2020;134:1123–7. https://doi.org/10.1017/S0022215120002455.
Aref ZF, Bazeed SEES, Hassan MH, Hassan AS, Rashad A, Hassan RG, et al. Clinical, biochemical and molecular evaluations of ivermectin mucoadhesive nanosuspension nasal spray in reducing upper respiratory symptoms of mild COVID-19. IJN. 2021;16:4063–72. https://doi.org/10.2147/IJN.S313093.
Fraile Navarro D, Tendal B, Tingay D, Vasilunas N, Anderson L, Best J, et al. Clinical care of children and adolescents with COVID-19: recommendations from the national COVID-19 clinical evidence taskforce. Med J Aust. 2022;216:255–63. https://doi.org/10.5694/mja2.51305.
Jansen AH, Russell BJ, Chernick V. Respiratory effects of H+ and dinitrophenol injections into the brain stem subarachnoid space of fetal lambs. Can J Physiol Pharmacol. 1975;53:726–33. https://doi.org/10.1139/y75-101.
Yonker LM, Shen K, Kinane TB. Lessons unfolding from pediatric cases of COVID-19 disease caused by SARS-CoV-2 infection. Pediatr Pulmonol. 2020;55:1085–6. https://doi.org/10.1002/ppul.24748.
Walker RWM, Darowski M, Morris P, Wraith JE. Anaesthesia and mucopolysaccharidoses: a review of airway problems in children. Anaesthesia. 1994. https://doi.org/10.1111/j.1365-2044.1994.tb04360.x.
Wolfe TR, Braude DA. Intranasal medication delivery for children: a brief review and update. Pediatrics. 2010;126:532–7. https://doi.org/10.1542/peds.2010-0616.
Yoshimura F, Suzuki T. Calcium-stimulated adenosine triphosphatase in the microsomal fraction of tooth germ from porcine fetus. Biochim Biophys Acta. 1975;410:167–77. https://doi.org/10.1016/0005-2744(75)90218-1.
Kolhe P, Shah M, Rathore N, (2013). American association of pharmaceutical scientists, editors. Sterile product development: formulation, process, quality and regulatory considerations. New York: Springer : AAPS Press.
Glenn JK, Goldman J. Task delegation to physician extenders–some comparisons. Am J Public Health. 1976;66:64–6. https://doi.org/10.2105/ajph.66.1.64.
Burton MJ, Clarkson JE, Goulao B, Glenny A-M, McBain AJ, Schilder AG, et al. Antimicrobial mouthwashes (gargling) and nasal sprays administered to patients with suspected or confirmed COVID-19 infection to improve patient outcomes and to protect healthcare workers treating them. Coch Database Syst Rev. 2020. https://doi.org/10.1002/14651858.CD013627.pub2.
Momper JD, Green DJ, Park K, Burckart GJ, Snyder DL. Ethical considerations for pediatric placebo-controlled trials: FDA outcomes and perspectives. Ther Innov Regul Sci. 2021;55:282–303. https://doi.org/10.1007/s43441-020-00214-3.
Frank S, Capriotti J, Brown SM, Tessema B. Povidone-iodine use in sinonasal and oral cavities: a review of safety in the COVID-19 era. Ear Nose Throat J. 2020;99:586–93. https://doi.org/10.1177/0145561320932318.
King RG, Silva-Sanchez A, Peel JN, Botta D, Dickson AM, Pinto AK, et al. Single-dose intranasal administration of AdCOVID elicits systemic and mucosal immunity against SARS-CoV-2 and fully protects mice from lethal challenge. Vaccines. 2021;9:881. https://doi.org/10.3390/vaccines9080881.
Sun W, McCroskery S, Liu W-C, Leist SR, Liu Y, Albrecht RA, et al. A newcastle disease virus (NDV) expressing a membrane-anchored spike as a cost-effective inactivated SARS-CoV-2 vaccine. Vaccines. 2020;8:771. https://doi.org/10.3390/vaccines8040771.
Lin Y, Yue S, Yang Y, Yang S, Pan Z, Yang X, et al. Nasal spray of neutralizing monoclonal antibody 35B5 confers potential prophylaxis against severe acute respiratory syndrome coronavirus 2 variants of concern: a small-scale clinical trial. Clin Infect Dis. 2022. https://doi.org/10.1093/cid/ciac448.
Dhama K, Dhawan M, Tiwari R, Emran TB, Mitra S, Rabaan AA, et al. COVID-19 intranasal vaccines: current progress, advantages, prospects, and challenges. Hum Vaccin Immunother. 2022;18:2045853. https://doi.org/10.1080/21645515.2022.2045853.
Touitou E, Natsheh H, Duchi S. Buspirone nanovesicular nasal system for non-hormonal hot flushes treatment. Pharmaceutics. 2018;10:82. https://doi.org/10.3390/pharmaceutics10030082.
Harris A. Review: clinical opportunities provided by the nasal administration of peptides. J Drug Target. 1993;1:101–16. https://doi.org/10.3109/10611869308996066.
Illum L. Nasal drug delivery—possibilities, problems and solutions. J Control Release. 2003;87:187–98. https://doi.org/10.1016/S0168-3659(02)00363-2.
Forbes B, Bommer R, Goole J, Hellfritzsch M, De Kruijf W, Lambert P, et al. A consensus research agenda for optimising nasal drug delivery. Expert Opin Drug Deliv. 2020;17:127–32. https://doi.org/10.1080/17425247.2020.1714589.
Keller L-A, Merkel O, Popp A. Intranasal drug delivery: opportunities and toxicologic challenges during drug development. Drug Deliv and Transl Res. 2022;12:735–57. https://doi.org/10.1007/s13346-020-00891-5.
Lobaina MY. Nasal route for vaccine and drug delivery: features and current opportunities. Int J Pharmaceut. 2019. https://doi.org/10.1016/j.ijpharm.2019.118813.
Kundoor V, Dalby RN. Effect of formulation- and administration-related variables on deposition pattern of nasal spray pumps evaluated using a nasal cast. Pharm Res. 2011;28:1895–904. https://doi.org/10.1007/s11095-011-0417-6.
Djupesland PG, Skretting A, Winderen M, Holand T. Bi-directional nasal delivery of aerosols can prevent lung deposition. J Aerosol Med. 2004;17:249–59. https://doi.org/10.1089/jam.2004.17.249.
Berkenfeld K, Lamprecht A, McConville JT. Devices for dry powder drug delivery to the lung. AAPS PharmSciTech. 2015;16:479–90. https://doi.org/10.1208/s12249-015-0317-x.
Kanowitz SJ, Batra PS, Citardi MJ. Topical budesonide via mucosal atomization device in refractory postoperative chronic rhinosinusitis. Otolaryngol Head Neck Surg. 2008;139:131–6. https://doi.org/10.1016/j.otohns.2008.03.009.
Marino D. Aptar Pharma’s Nasal Unidose Device Approved by US FDA. Drug Development and Delivery 2020. https://drug-dev.com/aptar-pharmas-nasal-unidose-device-approved-by-us-fda/ (accessed October 29, 2022).
SinusTM Pulsating Aerosol System - PARI n.d. https://www.pari.com/us/products/nebulizer-systems-for-the-sinuses-and-upper-airway-us/sinus-pulsating-aerosol-system-us/ (accessed October 29, 2022).
Illum L. Nasal drug delivery: recent developments and future prospects. J Control Release. 2012;161:254–63. https://doi.org/10.1016/j.jconrel.2012.01.024.
Westover JB, Ferrer G, Vazquez H, Bethencourt-Mirabal A, Go CC. In Vitro Virucidal Effect of Intranasally Delivered Chlorpheniramine Maleate Compound Against Severe Acute Respiratory Syndrome Coronavirus 2. Cureus 2020. https://doi.org/10.7759/cureus.10501
Acknowledgements
VPC wants to dedicate this work to L M College of pharmacy as a part of the 75th year celebration of the college.
Funding
Not applicable.
Author information
Authors and Affiliations
Contributions
VPC (VPC) prepared the manuscript's backbone and wrote the original draft of the manuscript along with other co-authors. All authors have read and approved the final version of the manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Chavda, V.P., Baviskar, K.P., Vaghela, D.A. et al. Nasal sprays for treating COVID-19: a scientific note. Pharmacol. Rep 75, 249–265 (2023). https://doi.org/10.1007/s43440-023-00463-7
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s43440-023-00463-7