Abstract
Background
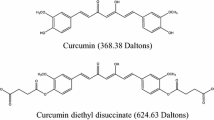
Curcumin, a natural polyphenol from Curcuma longa, is known to possess diversified pharmacological roles including anti-inflammatory, antioxidant, antiproliferative and antiangiogenic properties; however, its bioavailability is severely limited due to its poor solubility, poor absorption, rapid metabolism, and significant elimination. Hydrazinocurcumin (HZC), a novel analogue of curcumin has been reported to overcome the limitations of curcumin and also possesses multiple pharmacological activities. The present study aimed to evaluate the unexplored pharmacokinetic profile of this agent in experimental rats.
Methods
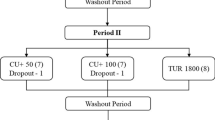
Drug formulations were administered to the experimental animals via oral, intravenous and intraperitoneal routes. Blood samples were collected at different pre-determined time intervals to determine the pharmacokinetic parameters. To understand the biodistribution profile of HCZ, tissue samples were isolated from different groups of Sprague–Dawley rats at different time points. The pharmacokinetic parameters of HZC were evaluated after administration through oral (100 mg/kg), intraperitoneal (100 mg/kg) and intravenous (10 mg/kg) routes.
Results
Significantly (p < 0.05) higher total AUC along with maximum concentration were evident with intraperitoneal administration when compared to the results of oral administration at a similar dose. In addition, shorter time to peak was observed with intraperitoneal administration. These results revealed a faster rate and longer duration of absorption with intraperitoneal administration, which further resulted in enhanced absolute bioavailability of HZC (29.17%) when compared to 5.1% upon oral dosing. The obtained data from the pharmacokinetic study indicated that HZC was instantaneously distributed and moderately eliminated from body fluids.
Conclusion
Based on the findings, it could be concluded that absorption of HZC is much higher via intraperitoneal route of administration compared to the oral administration.
Graphic abstract






Similar content being viewed by others
References
Amalraj A, Pius A, Gopi S, Gopi S. Biological activities of curcuminoids, other biomolecules from turmeric and their derivatives—a review. J Tradit Complement Med. 2017;7:205–33.
Sharifi-Rad J, Rayess YE, Rizk AA, Sadaka C, Zgheib R, Zam W, et al. Turmeric and its major compound curcumin on health: bioactive effects and safety profiles for food, pharmaceutical, biotechnological and medicinal applications. Front Pharmacol. 2020;11:01021.
Aggarwal BB, Sundaram C, Malani N, Ichikawa H. Curcumin: the Indian solid gold. Adv Exp Med Biol. 2007;595:1–75.
Dei Cas M, Ghidoni R. Dietary curcumin correlation between bioavailability and health potential. Nutrients. 2019. https://doi.org/10.3390/nu11092147.
Leung MH, Kee TW. Effective stabilization of curcumin by association to plasma proteins: human serum albumin and fibrinogen. Langmuir ACS J Surfaces Colloids. 2009;25:5773–7.
Zhao S, Pi C, Ye Y, Zhao L, Wei Y. Recent advances of analogues of curcumin for treatment of cancer. Eur J Med Chem. 2019;180:524–35.
Mbese Z, Khwaza V, Aderibigbe BA. Curcumin and Its Derivatives as Potential Therapeutic Agents in Prostate Colon and Breast Cancers. Molecules. 2019. https://doi.org/10.3390/molecules24234386.
Noureddin SA, El-Shishtawy RM, Al-Footy KO. Curcumin analogues and their hybrid molecules as multifunctional drugs. Euro J Med Chem. 2019. https://doi.org/10.1016/j.ejmech.2019.111631.
Chainoglou E, Hadjipavlou-Litina D. Curcumin analogues and derivatives with anti-proliferative and anti-inflammatory activity: structural characteristics and molecular targets. Expert Opin Drug Discov. 2019;14:821–42.
Chainoglou E, Hadjipavlou-Litina D. Curcumin in Health and diseases: Alzheimer’s disease and curcumin analogues, derivatives, and hybrids. Int J Mol Sci. 2020. https://doi.org/10.3390/ijms21061975.
Panahi Y, Fazlolahzadeh O, Atkin SL, Majeed M, Butler AE, Johnston TP, et al. Evidence of curcumin and curcumin analogue effects in skin diseases: a narrative review. J Cell Physiol. 2019;234:1165–78.
Moghadamtousi SZ, Kadir HA, Hassandarvish P, Tajik H, Abubakar S, Zandi K. A review on antibacterial, antiviral, and antifungal activity of curcumin. Biomed Res Int. 2014. https://doi.org/10.1155/2014/186864.
Sumeet G, Rachna K, Samrat C, Ipshita C, Vikas J, Manu S. Anti inflammatory and anti arthritic activity of different milk based formulation of curcumin in rat model. Curr Drug Deliv. 2018;15:205–14.
Arshad L, Haque MA, Abbas Bukhari SN, Jantan I. An overview of structure-activity relationship studies of curcumin analogs as antioxidant and anti-inflammatory agents. Future Med Chem. 2017;9:605–26.
Poma P, Notarbartolo M, Labbozzetta M, Maurici A, Carina V, Alaimo A, et al. The antitumor activities of curcumin and of its isoxazole analogue are not affected by multiple gene expression changes in an MDR model of the MCF-7 breast cancer cell line: analysis of the possible molecular basis. Int J Mol Med. 2007;20:329–35.
Wang X, Zhang Y, Zhang X, Tian W, Feng W, Chen T. The curcumin analogue hydrazinocurcumin exhibits potent suppressive activity on carcinogenicity of breast cancer cells via STAT3 inhibition. Int J Oncol. 2012;40:1189–95.
Fu M, Chen L, Zhang L, Yu X, Yang Q. Cyclocurcumin, a curcumin derivative, exhibits immune-modulating ability and is a potential compound for the treatment of rheumatoid arthritis as predicted by the MM-PBSA method. Int J Mol Med. 2017;39:1164–72.
Shim JS, Kim DH, Jung HJ, Kim JH, Lim D, Lee SK, et al. Hydrazinocurcumin, a novel synthetic curcumin derivative, is a potent inhibitor of endothelial cell proliferation. Bioorg Med Chem. 2002;10:2987–92.
Zhou Y, Zhang M, Zhang Z, Jia Y, Zhang C, Peng L. Hydrazinocurcumin and 5-fluorouracil enhance apoptosis and restrain tumorigenicity of HepG2 cells via disrupting the PTEN-mediated PI3K/Akt signaling pathway. Biomed pharmacother. 2020. https://doi.org/10.1016/j.biopha.2020.109851.
Zhang X, Tian W, Cai X, Wang X, Dang W, Tang H, et al. Hydrazinocurcumin Encapsuled nanoparticles “re-educate” tumor-associated macrophages and exhibit anti-tumor effects on breast cancer following STAT3 suppression. PLoS ONE. 2013. https://doi.org/10.1371/journal.pone.0065896.
Carvalho DdM, Takeuchi KP, Geraldine RM, Moura CJd, Torres MCL. Production, solubility and antioxidant activity of curcumin nanosuspension. Food Sci Technol. 2015;35:115–9.
Rathore R, Jain JP, Srivastava A, Jachak SM, Kumar N. Simultaneous determination of hydrazinocurcumin and phenol red in samples from rat intestinal permeability studies: HPLC method development and validation. J Pharm Biomed Anal. 2008;46:374–80.
Satyavert GS, Nair AB, Attimarad M. Development and validation of bioanalytical method for the determination of hydrazinocurcumin in rat plasma and organs by HPLC-UV. J Chromatogr B Analyt Technol Biomed Life Sci. 2020. https://doi.org/10.1016/j.jchromb.2020.122310.
Selvam C, Jachak SM, Thilagavathi R, Chakraborti AK. Design, synthesis, biological evaluation and molecular docking of curcumin analogues as antioxidant, cyclooxygenase inhibitory and anti-inflammatory agents. Bioorg Med Chem Lett. 2005;15:1793–7.
Thackaberry EA, Wang X, Schweiger M, Messick K, Valle N, Dean B, et al. Solvent-based formulations for intravenous mouse pharmacokinetic studies: tolerability and recommended solvent dose limits. Xenobiotica. 2014;44:235–41.
Shehata TM, Nair AB, Al-Dhubiab BE, Shah J, Jacob S, Alhaider IA, et al. Vesicular emulgel based system for transdermal delivery of insulin: factorial design and in vivo evaluation. Appl Sci. 2020;10:5341.
Roy B, Choudhury H, Das A, Das AK, Pal TK. Development and validation of a liquid chromatography-tandem mass spectrometry method to determine ulifloxacin, the active metabolite of prulifloxacin in rat and rabbit plasma: application to toxicokinetic study. Biomed Chromatogr BMC. 2011;25:890–901.
Nair A, Morsy MA, Jacob S. Dose translation between laboratory animals and human in preclinical and clinical phases of drug development. Drug Dev Res. 2018;79:373–82.
Nair AB, Shah J, Al-Dhubiab BE, Patel SS, Morsy MA, Patel V, et al. Development of Asialoglycoprotein Receptor Targeted Nanoparticles for Selective Delivery of Gemcitabine to Hepatocellular Carcinoma. Molecules. 2019. https://doi.org/10.3390/molecules24244566.
Jhaveri M, Nair AB, Shah J, Jacob S, Patel V, Mehta T. Improvement of oral bioavailability of carvedilol by liquisolid compact: optimization and pharmacokinetic study. Drug Deliv Transl Res. 2020;10:975–85.
Dansirikul C, Choi M, Duffull SB. Estimation of pharmacokinetic parameters from non-compartmental variables using Microsoft Excel. Comput Biol Med. 2005;35:389–403.
Jacob S, Nair AB. An updated overview with simple and practical approach for developing in vitro-in vivo correlation. Drug Dev Res. 2018;79:97–110.
Hilger RA, Jacek G, Oberhoff C, Kredtke S, Baumgart J, Seeber S, et al. Investigation of bioavailability and pharmacokinetics of treosulfan capsules in patients with relapsed ovarian cancer. Cancer Chemother Pharmacol. 2000;45:483–8.
Lukas G, Brindle SD, Greengard P. The route of absorption of intraperitoneally administered compounds. J Pharmacol Exp Ther. 1971;178:562–4.
Rehman S, Nabi B, Fazil M, Khan S, Bari NK, Singh R, et al. Role of P-Glycoprotein Inhibitors in the bioavailability enhancement of solid dispersion of darunavir. Biomed Res Int. 2017;2017:8274927.
Choudhury H, Gorain B, Karmakar S, Biswas E, Dey G, Barik R, et al. Improvement of cellular uptake, in vitro antitumor activity and sustained release profile with increased bioavailability from a nanoemulsion platform. Int J Pharm. 2014;460:131–43.
Sabet S, Rashidinejad A, Melton LD, McGillivray DJ. Recent advances to improve curcumin oral bioavailability. Trends in Food Sci Technol. 2021. https://doi.org/10.1016/j.tifs.2021.02.006.
Yang KY, Lin LC, Tseng TY, Wang SC, Tsai TH. Oral bioavailability of curcumin in rat and the herbal analysis from Curcuma longa by LC-MS/MS. J Chromatogr B Anal Technol Biomed Life Sci. 2007;853:183–9.
Al Shoyaib A, Archie SR, Karamyan VT. Intraperitoneal route of drug administration: should it be used in experimental animal studies? Pharm Res. 2019;37:12.
Pan MH, Huang TM, Lin JK. Biotransformation of curcumin through reduction and glucuronidation in mice. Drug Metab Dispos Biol Fate Chem. 1999;27:486–94.
Ning ZH, Long S, Zhou YY, Peng ZY, Sun YN, Chen SW, et al. Effect of exposure routes on the relationships of lethal toxicity to rats from oral, intravenous, intraperitoneal and intramuscular routes. Regul Toxicol Pharmacol RTP. 2015;73:613–9.
Yu RH, Cao YX. A method to determine pharmacokinetic parameters based on andante constant-rate intravenous infusion. Sci Rep. 2017;7:13279.
Beconi MG, Howland D, Park L, Lyons K, Giuliano J, Dominguez C, et al. Pharmacokinetics of memantine in rats and mice. PLoS Curr. 2011. https://doi.org/10.1371/currents.RRN1291.
Miners JO, Yang X, Knights KM, Zhang L. The role of the kidney in drug elimination: transport, metabolism, and the impact of kidney disease on drug clearance. Clin Pharmacol Ther. 2017;102:436–49.
Almazroo OA, Miah MK, Venkataramanan R. Drug metabolism in the liver. Clin Liver Dis. 2017;21:1–20.
Ravindranath V, Chandrasekhara N. Absorption and tissue distribution of curcumin in rats. Toxicology. 1980;16:259–65.
Garcea G, Berry DP, Jones DJ, Singh R, Dennison AR, Farmer PB, et al. Consumption of the putative chemopreventive agent curcumin by cancer patients: assessment of curcumin levels in the colorectum and their pharmacodynamic consequences. Cancer Epidemiol Biomark Prev. 2005;14:120–5.
Acknowledgements
The authors are grateful to management for offering the requisite technical help to accomplish this study.
Author information
Authors and Affiliations
Contributions
S: conceptualization, data curation, formal analysis, investigation, methodology and writing—original draft preparation. SG: conceptualization, data curation, formal analysis, investigation, methodology and writing—review and editing. HC: formal analysis, investigation, methodology and writing—review and editing. SJ: formal analysis, investigation, methodology and writing—review and editing. ABN: formal analysis, investigation, methodology and writing—review and editing. All authors have read and agreed to the published version of the manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors report no conflicts of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Satyavert, Gupta, S., Choudhury, H. et al. Pharmacokinetics and tissue distribution of hydrazinocurcumin in rats. Pharmacol. Rep 73, 1734–1743 (2021). https://doi.org/10.1007/s43440-021-00312-5
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s43440-021-00312-5