Abstract
Purpose
Magnetically controlled growing rod (MCGR) for the treatment of early-onset scoliosis (EOS) is a relatively innovative technique. MCGR benefits over traditional growing rods are known but limitations and complications are being revealed. The purpose of this study was to examine the importance of tissue depth on rod lengthening.
Methods
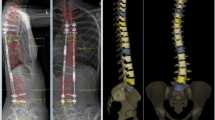
A single-institution retrospective review of 72 MCGR patients was performed. Ultrasound measured rod distraction. Differences in programmed and actual distraction, and complications were recorded. Tissue depths and achieved length were averaged and used to construct a regression to account for variability.
Results
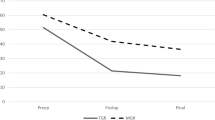
Percentage of std and offset orientation rod lengthening relative to the programmed distraction was inversely proportional to rod depth (std R = 0.50, p = 0.002) (offset R = 0.60, p < 0.001). Expected std rod lengthening achieved decreased by 1.46%/mm depth. Expected offset rod lengthening achieved decreased by 1.68%/mm depth. 28 pts (38.9%) sustained complications. Age, sex, BMI, standard tissue depth, and/or offset tissue depth had no predictive ability with respect to complications sustained (overall model R = 0.31, p = 0.36).
Conclusion
In a series of EOS surgical patients treated with MCGRs, the relationship between percentage of programmed lengthening achieved as well as total lengthening was inversely proportional to tissue depth of the rod. There was a trend towards increasing frequency of complications recorded with decreasing tissue depth though this was not significant. These data can help with surgical planning during MCGR placement.


Similar content being viewed by others
References
The 2nd international congress on early-onset scoliosis and growing spine, November 7–8, 2008, Montreal, Quebec, chairman: behrooz a. Akbarnia, MD. J Child Orthop 3(2):145–68
Fletcher ND, Bruce RW (2012) Early-onset scoliosis: current concepts and controversies. Curr Rev Musculoskelet Med 5(2):102–110
Thompson GH, Akbarnia BA, Campbell RM Jr (2007) Growing rod techniques in early-onset scoliosis. J Pediatr Orthop 27(3):354–361
Tis JE et al (2012) Early-onset scoliosis: modern treatment and results. J Pediatr Orthop 32(7):647–657
Odent T et al (2015) Fusionless surgery in early-onset scoliosis. Orthop Traumatol Surg Res 101(6 Suppl):S281–S288
Elsebai HB et al (2011) Safety and efficacy of growing rod technique for pediatric congenital spinal deformities. J Pediatr Orthop 31(1):1–5
Akbarnia BA et al (2014) Traditional growing rods versus magnetically controlled growing rods for the surgical treatment of early-onset scoliosis: a case-matched 2-year study. Spine Deform 2(6):493–497
Teoh KH et al (2016) Do magnetic growing rods have lower complication rates compared with conventional growing rods? Spine J 16(4 Suppl):S40–S44
Choi E et al (2017) Implant complications after magnetically controlled growing rods for early-onset scoliosis: a multicenter retrospective review. J Pediatr Orthop 37(8):e588–e592
Bess S et al (2010) Complications of growing-rod treatment for early-onset scoliosis: analysis of one hundred and forty patients. J Bone Jt Surg Am 92(15):2533–2543
Sankar WN, Acevedo DC, Skaggs DL (2010) Comparison of complications among growing spinal implants. Spine (Phila Pa 1976) 35(23):2091–2096
Yang JS et al (2011) Growing rod fractures: risk factors and opportunities for prevention. Spine (Phila Pa 1976) 36(20):1639–1644
Kabirian N et al (2014) Deep surgical site infection following 2344 growing-rod procedures for early-onset scoliosis: risk factors and clinical consequences. J Bone Jt Surg Am 96(15):e128
Hosseini P et al (2017) Rod fracture and lengthening intervals in traditional growing rods: is there a relationship? Eur Spine J 26(6):1690–1695
Gilday SE et al (2018) Observed length increases of magnetically controlled growing rods are lower than programmed. J Pediatr Orthop 38(3):e133–e137
Wang Q et al (2016) Validity study of vertebral rotation measurement using 3-D ultrasound in adolescent idiopathic scoliosis. Ultrasound Med Biol 42(7):1473–1481
Moratalla J et al (2010) Semi-automated system for measurement of nuchal translucency thickness. Ultrasound Obstet Gynecol 36(4):412–416
Zheng R et al (2018) Factors influencing spinal curvature measurements on ultrasound images for children with adolescent idiopathic scoliosis (AIS). PLoS ONE 13(6):e0198792
Hwang M, Piskunowicz M, Darge K (2019) Advanced ultrasound techniques for pediatric imaging. Pediatrics 143(3)
Kayaalp L et al (2006) Psychological effects of repeated general anesthesia in children. Paediatr Anaesth 16(8):822–827
Flynn JM et al (2012) Psychological dysfunction in children who require repetitive surgery for early-onset scoliosis. J Pediatr Orthop 32(6):594–599
Aslan C et al (2017) Psychological profile of children who require repetitive surgical procedures for early-onset scoliosis: is a poorer quality of life the cost of a straighter spine? Spine Deform 5(5):334–341
Hu D et al (2017) Association between exposure of young children to procedures requiring general anesthesia and learning and behavioral outcomes in a population-based birth cohort. Anesthesiology 127(2):227–240
Cheung KM et al (2012) Magnetically controlled growing rods for severe spinal curvature in young children: a prospective case series. Lancet 379(9830):1967–1974
Charroin C et al (2014) Direct costs associated with the management of progressive early-onset scoliosis: estimations based on gold standard technique or with magnetically controlled growing rods. Orthop Traumatol Surg Res 100(5):469–474
Doany ME et al (2018) Health-related quality of life in early-onset scoliosis patients treated surgically: EOSQ scores in traditional growing rod versus magnetically controlled growing rods. Spine (Phila Pa 1976) 43(2):148–153
Bekmez S et al (2019) Is magnetically controlled growing rod the game changer in early-onset scoliosis? A preliminary report. J Pediatr Orthop 39(3):e195–e200
Oetgen ME, McNulty EM, Matthews AL (2019) Cost-effectiveness of magnetically controlled growing rods: who really benefits? Spine Deform 7(3):501–504
Dannawi Z et al (2013) Early results of a remotely-operated magnetic growth rod in early-onset scoliosis. Bone Jt J 95(1):75–80
Heydar AM, Sirazi S, Bezer M (2016) Magnetic controlled growing rods as a treatment of early-onset scoliosis: early results with two patients. Spine (Phila Pa 1976) 41(22):1336–1342
Yilmaz B et al (2016) Magnetically controlled growing rod in early-onset scoliosis: a minimum of 2-year follow-up. Pediatr Neurosurg 51(6):292–296
La Rosa G, Oggiano L, Ruzzini L (2017) Magnetically controlled growing rods for the management of early-onset scoliosis: a preliminary report. J Pediatr Orthop 37(2):79–85
Beaven A et al (2018) Magnetically controlled growing rods: the experience of mechanical failure from a single center consecutive series of 28 children with a minimum follow-up of 2 years. Asian Spine J 12(5):794–802
Thakar C et al (2018) Systematic review of the complications associated with magnetically controlled growing rods for the treatment of early-onset scoliosis. Eur Spine J 27(9):2062–2071
Funding
No funding was required. This was part of routine care.
Author information
Authors and Affiliations
Contributions
CS: study conception and design, data analysis, manuscript draft, commented on previous versions of the manuscript, read and approved the final manuscript. SG: study conception and design, Material preparation, data collection, commented on previous versions of the manuscript, read and approved the final manuscript. VJ: study conception and design, commented on previous versions of the manuscript, read and approved the final manuscript. PS: study conception and design, commented on previous versions of the manuscript, read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethical approval
This research study was conducted retrospectively from data obtained for clinical purposes. We consulted extensively with the IRB of Cincinnati Children’s Hospital Medical Center who determined that our study did not need ethical approval. An IRB official waiver of ethical approval was granted from the IRB of Cincinnati Children’s Hospital Medical Center.
Conflict of interest
The authors have no conflict of interest. Dr. Sturm reports other support from DePuy, a Johnson and Johnson Company, Nuvasive, and Green Sun Medical, outside the submitted work.
Informed consent
As this was a retrospective chart review of routine care, no informed consent was required.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Seidel, C.P., Gilday, S.E., Jain, V.V. et al. How much does depth matter? Magnetically controlled growing rod distraction directly influenced by rod tissue depth. Spine Deform 10, 177–182 (2022). https://doi.org/10.1007/s43390-021-00399-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s43390-021-00399-z