Abstract
Study design
Retrospective study.
Objective
To report the incidence of revision surgery due to mechanical failure following pedicle subtraction osteotomy (PSO) in adult spinal deformity (ASD) patients.
Summary of background data
PSO allow major surgical correction of ASD, although; the risk of mechanical complications remains considerable. Previous reports have been based on smaller cohorts or multicenter databases and none have utilized competing risk (CR) survival analysis.
Methods
All ASD patients undergoing PSO surgery from 2010 to 2015 at a single, tertiary institution were included. Demographics, long standing radiographs as well as intra- and postoperative complications were registered for all. A CR-model was used to estimate the incidence of revision surgery due to mechanical failure and two predefined multivariable models were used to assess radiographic prediction of failure and reported as odds ratios (OR) with 95% confidence intervals (95% CI).
Results
A total of 171 patients were included with 2-year follow-up available for 91% (mean [IQR]: 35 [24–50] months). Mechanical failure occurred in 111 cases (65%) at any time in follow-up, the most frequent being rod breakage affecting 81 patients (47%). Cumulative incidence of revision surgery due to mechanical failure was estimated to 34% at 2 years and 58% at 5 years. A multivariable proportional odds model with death as competing risk showed significantly increased odds of revision with fusion to the sacrum (OR: 5.42; 95% CI 1.89–15.49) and preoperative pelvic tilt (PT) > 20° (OR: 2.41; 95% CI 1.13–5.16). History of previous surgery, number of instrumented vertebra, as well as postoperative SRS-Schwab modifiers and Global Alignment and Proportion score were not associated with significant effects on odds of revision.
Conclusions
In a consecutive single-center cohort of patients undergoing PSO for ASD, we found an estimated incidence of revision surgery due to mechanical failure of 34% 2 years postoperatively. Fusion to the sacrum and preoperative PT > 20° were associated with elevated risks of revision.
Level of evidence
Prognostic III.




Similar content being viewed by others
References
Ames CP, Scheer JK, Lafage V, Smith JS, Bess S, Berven SH et al (2016) Adult spinal deformity: epidemiology, health impact, evaluation, and management. Spine Deform 4:310–322. https://doi.org/10.1016/j.jspd.2015.12.009
Imagama S, Hasegawa Y, Matsuyama Y, Sakai Y, Ito Z, Hamajima N et al (2011) Influence of sagittal balance and physical ability associated with exercise on quality of life in middle-aged and elderly people. Arch Osteoporos 6:13–20. https://doi.org/10.1007/s11657-011-0052-1
Schwab F, Farcy J-P, Bridwell K, Berven S, Glassman S, Harrast J et al (2006) A clinical impact classification of scoliosis in the adult. Spine (Phila Pa 1976) 31:2109–2114. https://doi.org/10.1097/01.brs.0000231725.38943.ab
Lafage V, Schwab F, Patel A, Hawkinson N, Farcy J-P (2009) Pelvic tilt and truncal inclination. Spine (Phila Pa 1976) 34:E599–606. https://doi.org/10.1097/BRS.0b013e3181aad219
Glassman SD, Berven S, Bridwell K, Horton W, Dimar JR (2005) Correlation of radiographic parameters and clinical symptoms in adult scoliosis. Spine (Phila Pa 1976) 30:682–688. https://doi.org/10.1097/01.brs.0000155425.04536.f7
Hassanzadeh H, Jain A, El Dafrawy MH, Ain MC, Mesfin A, Skolasky RL et al (2012) Three-column osteotomies in the treatment of spinal deformity in adult patients 60 years old and older: outcome and complications. Spine (Phila Pa 1976) 38:726–731. https://doi.org/10.1097/BRS.0b013e31827c2415
Schwab FJ, Hamill CL, Horton WC, Ondra SL, Sansur CA, Bridwell KH et al (2011) Risk-benefit assessment of surgery for adult scoliosis. Spine (Phila Pa 1976) 36:817–824. https://doi.org/10.1097/BRS.0b013e3181e21783
Kiaer T, Gehrchen M (2010) Transpedicular closed wedge osteotomy in ankylosing spondylitis: results of surgical treatment and prospective outcome analysis. Eur Spine J 19:57–64. https://doi.org/10.1007/s00586-009-1104-8
Cho K-J, Kim K-T, Kim W-J, Lee S-H, Jung J-H, Kim Y-T et al (2013) Pedicle subtraction osteotomy in elderly patients with degenerative sagittal imbalance. Spine (Phila Pa 1976) 38:E1561–E1566. https://doi.org/10.1097/BRS.0b013e3182a63c29
Lenke LG, Sides BA, Koester LA, Hensley M, Blanke KM (2010) Vertebral column resection for the treatment of severe spinal deformity. Clin Orthop Relat Res 468:687–699. https://doi.org/10.1007/s11999-009-1037-x
Hallager DW, Karstensen S, Bukhari N, Gehrchen M, Dahl B (2017) Radiographic predictors for mechanical failure after adult spinal deformity surgery. Spine (Phila Pa 1976) 42:E855–E863. https://doi.org/10.1097/BRS.0000000000001996
Sciubba DM, Yurter A, Smith JS, Kelly MP, Scheer JK, Goodwin CR et al (2015) A comprehensive review of complication rates after surgery for adult deformity: a reference for informed consent. Spine Deform 3:575–594. https://doi.org/10.1016/j.jspd.2015.04.005
Charosky S, Guigui P, Blamoutier A, Roussouly P, Chopin D (2012) Complications and risk factors of primary adult scoliosis surgery. Spine (Phila Pa 1976) 37:693–700. https://doi.org/10.1097/BRS.0b013e31822ff5c1
Varadhan R, Weiss CO, Segal JB, Wu AW, Scharfstein D, Boyd C (2010) Evaluating health outcomes in the presence of competing risks: a review of statistical methods and clinical applications. Med Care S96–S105
Southern DA, Faris PD, Brant R, Galbraith PD, Norris CM, Knudtson ML et al (2006) Kaplan–Meier methods yielded misleading results in competing risk scenarios. J Clin Epidemiol 59:1110–1114. https://doi.org/10.1016/j.jclinepi.2006.07.002
Maillot C, Ferrero E, Fort D, Heyberger C, Le Huec J-C (2015) Reproducibility and repeatability of a new computerized software for sagittal spinopelvic and scoliosis curvature radiologic measurements: Keops®. Eur Spine J 24:1574–1581. https://doi.org/10.1007/s00586-015-3817-1
Hart RA, McCarthy I, Ames CP, Shaffrey CI, Hamilton DK, Hostin R (2013) Proximal junctional kyphosis and proximal junctional failure. Neurosurg Clin N Am 24:213–218. https://doi.org/10.1016/j.nec.2013.01.001
Roussouly P, Gollogly S, Berthonnaud E, Dimnet J (2005) Classification of the normal variation in the sagittal alignment of the human lumbar spine and pelvis in the standing position. Spine (Phila Pa 1976) 30:346–353
R Core Team (2017) R: a language and environment for statistical computing. R Foundation Statistical Computing, Vienna. https://www.r-project.org/
Therneau TM, Grambsch PM (2015) A package for survival analysis in R. version 2.38., https://CRAN.R-project.org/package=survival
Therneau TM, Grambsch PM (2013) Modeling survival data: extending the Cox model. Springer Science & Business Media
Gerds TA (2017) Prodlim: product-limit estimation for censored event history analysis. R package version 1.6.1. https://CRAN.R-project.org/package=prodlim
Scheike TH, Martinussen T (2006) Timereg: dynamic regression models for survival data. Springer, New-York
Scheike TH, Zhang M-J (2011) Analyzing competing risk data using the R timereg Package. J Stat Softw. https://doi.org/10.18637/jss.v038.i02
Aalen OO, Johansen S (1978) An empirical transition matrix for non-homogeneous Markov chains based on censored observations. Scand J Stat 5:141–150
Fine JP (2001) Regression modeling of competing crude failure probabilities. Biostatistics 2:85–97. https://doi.org/10.1093/biostatistics/2.1.85
Eriksson F, Li J, Scheike T, Zhang M-J (2015) The proportional odds cumulative incidence model for competing risks. Biometrics 71:687–695. https://doi.org/10.1111/biom.12330
Harrell FE Jr, Lee KL, Mark DB (1996) Multivariable prognostic models: issues in developing models, evaluating assumptions and adequacy, and measuring and reducing errors. Stat Med 15:361–387
Kim HJ, Bridwell KH, Lenke LG, Park MS, Song KS, Piyaskulkaew C et al (2014) Patients with proximal junctional kyphosis requiring revision surgery have higher postoperative lumbar lordosis and larger sagittal balance corrections. Spine (Phila Pa 1976) 39:576–580. https://doi.org/10.1097/BRS.0000000000000246
Maruo K, Ha Y, Inoue S, Samuel S, Okada E, Hu SS et al (2013) Predictive factors for proximal junctional kyphosis in long fusions to the sacrum in adult spinal deformity. Spine (Phila Pa 1976) 38:14–20. https://doi.org/10.1097/BRS.0b013e3182a51d43
Bridwell KH, Lenke LG, Cho SK, Pahys JM, Zebala LP, Dorward IG et al (2013) Proximal junctional kyphosis in primary adult deformity surgery: evaluation of 20 degrees as a critical angle. Neurosurgery 72:899–906. https://doi.org/10.1227/NEU.0b013e31828bacd8
Yagi M, King AB, Boachie-Adjei O (2012) Incidence, risk factors, and natural course of proximal junctional kyphosis: surgical outcomes review of adult idiopathic scoliosis. Minimum 5 years of follow-up. Spine (Phila Pa 1976) 37:1479–1489. https://doi.org/10.1097/BRS.0b013e31824e4888
Kim HJ, Yagi M, Nyugen J, Cunningham ME, Boachie-Adjei O (2012) Combined anterior-posterior surgery is the most important risk factor for developing proximal junctional kyphosis in idiopathic scoliosis. Clin Orthop Relat Res 470:1633–1639. https://doi.org/10.1007/s11999-011-2179-1
Lonner BS, Newton P, Betz R, Scharf C, O’Brien M, Sponseller P et al (2007) Operative management of Scheuermannʼs kyphosis in 78 patients. Spine (Phila Pa 1976) 32:2644–2652. https://doi.org/10.1097/BRS.0b013e31815a5238
Kim YJ, Lenke LG, Bridwell KH, Kim J, Cho SK, Cheh G et al (2007) Proximal junctional kyphosis in adolescent idiopathic scoliosis after 3 different types of posterior segmental spinal instrumentation and fusions: incidence and risk factor analysis of 410 cases. Spine (Phila Pa 1976) 32:2731–2738. https://doi.org/10.1097/BRS.0b013e31815a7ead
Nicholls FH, Bae J, Theologis AA, Eksi MS, Ames CP, Berven SH et al (2017) Factors associated with the development of and revision for proximal junctional kyphosis in 440 consecutive adult spinal deformity patients. Spine (Phila Pa 1976) 42:1693–1698. https://doi.org/10.1097/BRS.0000000000002209
Passias PG, Soroceanu A, Yang S, Schwab F, Ames C, Boniello A et al (2016) Predictors of revision surgical procedure excluding wound complications in adult spinal deformity and impact on patient-reported outcomes and satisfaction: a two-year follow-up. J Bone Jt Surg Am 98:536–543. https://doi.org/10.2106/JBJS.14.01126
Kim YJ, Bridwell KH, Lenke LG, Glattes CR, Rhim S, Cheh G (2008) Proximal junctional kyphosis in adult spinal deformity after segmental posterior spinal instrumentation and fusion. Spine (Phila Pa 1976) 33:2179–2184. https://doi.org/10.1097/BRS.0b013e31817c0428
Kim YJ, Bridwell KH, Lenke LG, Cho K-J, Edwards CC, Rinella AS (2006) Pseudarthrosis in adult spinal deformity following multisegmental instrumentation and arthrodesis. J Bone Jt Surg 88:721–728. https://doi.org/10.2106/JBJS.E.00550
Inoue S, Khashan M, Fujimori T, Berven SH (2015) Analysis of mechanical failure associated with reoperation in spinal fusion to the sacrum in adult spinal deformity. J Orthop Sci. https://doi.org/10.1007/s00776-015-0729-1
Maier S, Smith JS, Schwab FJ, Obeid I, Mundis G, Klineberg E et al (2014) Revision surgery after three-column osteotomy in 335 adult spinal deformity patients: inter-center variability and risk factors. Spine (Phila Pa 1976) 39:881–885. https://doi.org/10.1097/BRS.0000000000000304
Lertudomphonwanit T, Kelly MP, Bridwell KH, Lenke LG, McAnany SJ, Punyarat P et al (2018) Rod fracture in adult spinal deformity surgery fused to the sacrum: prevalence, risk factors, and impact on health-related quality of life in 526 patients. Spine J 18:1612–1624. https://doi.org/10.1016/j.spinee.2018.02.008
Park SJ, Lee CS, Chung SS, Lee JY, Kang SS, Park SH (2016) Different risk factors of proximal junctional kyphosis and proximal junctional failure following long instrumented fusion to the sacrum for adult spinal deformity: survivorship analysis of 160 patients. Neurosurgery 80:279–286. https://doi.org/10.1227/NEU.0000000000001240
Smith JS, Shaffrey E, Klineberg E, Shaffrey CI, Lafage V, Schwab FJ et al (2014) Prospective multicenter assessment of risk factors for rod fracture following surgery for adult spinal deformity. J Neurosurg Spine 21:994–1003. https://doi.org/10.3171/2014.9.SPINE131176
Ames CP, Smith JS, Scheer JK, Bess S, Bederman SS, Deviren V et al (2012) Impact of spinopelvic alignment on decision making in deformity surgery in adults: a review. J Neurosurg Spine 16:547–564. https://doi.org/10.3171/2012.2.SPINE11320
Rothenfluh DA, Mueller DA, Rothenfluh E, Min K (2015) Pelvic incidence-lumbar lordosis mismatch predisposes to adjacent segment disease after lumbar spinal fusion. Eur Spine J 24:1251–1258. https://doi.org/10.1007/s00586-014-3454-0
Schwab F, Ungar B, Blondel B, Buchowski J, Coe J, Deinlein D et al (2012) Scoliosis research society—Schwab adult spinal deformity classification. Spine (Phila Pa 1976) 37:1077–1082. https://doi.org/10.1097/BRS.0b013e31823e15e2
Yilgor C, Sogunmez N, Boissiere L, Yavuz Y, Obeid I, Kleinstück F et al (2017) Global alignment and proportion (GAP) score. J Bone Jt Surg Am 99A:1661–1672. https://doi.org/10.2106/JBJS.16.01594
Smith JS, Shaffrey CI, Klineberg E, Lafage V, Schwab F, Lafage R et al (2017) Complication rates associated with 3-column osteotomy in 82 adult spinal deformity patients: retrospective review of a prospectively collected multicenter consecutive series with 2-year follow-up. J Neurosurg Spine 27:444–457. https://doi.org/10.3171/2016.10.SPINE16849
Kim YJ, Bridwell KH, Lenke LG, Rinella AS, Edwards C, Edward C (2005) Pseudarthrosis in primary fusions for adult idiopathic scoliosis: incidence, risk factors, and outcome analysis. Spine (Phila Pa 1976) 30:468–474. https://doi.org/10.1097/01.brs.0000153392.74639.ea
Legaye J, Duval-Beaupère G, Hecquet J, Marty C (1998) Pelvic incidence: a fundamental pelvic parameter for three-dimensional regulation of spinal sagittal curves. Eur Spine J 7:99–103. https://doi.org/10.1007/s005860050038
Lafage R, Schwab F, Challier V, Henry JK, Gum J, Smith J et al (2016) Defining spino-pelvic alignment thresholds should operative goals in adult spinal deformity surgery account for age? Spine (Phila Pa 1976) 41:62–68. https://doi.org/10.1097/BRS.0000000000001171
Lewis SJ, Abbas H, Chua S, Bacon S, Bronstein Y, Goldstein S et al (2012) Upper instrumented vertebral fractures in long lumbar fusions: what are the associated risk factors? Spine (Phila Pa 1976) 37:1407–1414. https://doi.org/10.1097/BRS.0b013e31824fffb9
Laouissat F, Sebaaly A, Gehrchen M, Roussouly P (2018) Classification of normal sagittal spine alignment: refounding the Roussouly classification. Eur Spine J 27:2002–2011. https://doi.org/10.1007/s00586-017-5111-x
Sebaaly A, Grobost P, Mallam L, Roussouly P (2018) Description of the sagittal alignment of the degenerative human spine. Eur Spine J 27:489–496. https://doi.org/10.1007/s00586-017-5404-0
Lewis SJ, Mohanty C, Gazendam AM, Kato S, Keshen SG, Lewis ND et al (2018) Posterior column reconstruction improves fusion rates at the level of osteotomy in three-column posterior-based osteotomies. Eur Spine J 27:636–643. https://doi.org/10.1007/s00586-017-5299-9
Luca A, Ottardi C, Sasso M, Prosdocimo L, La Barbera L, Brayda-Bruno M et al (2017) Instrumentation failure following pedicle subtraction osteotomy: the role of rod material, diameter, and multi-rod constructs. Eur Spine J 26:764–770. https://doi.org/10.1007/s00586-016-4859-8
Hyun SJ, Rhim SC (2010) Clinical outcomes and complications after pedicle subtraction osteotomy for fixed sagittal imbalance patients: a long-term follow-up data. J Korean Neurosurg Soc 47:95–101. https://doi.org/10.3340/jkns.2010.47.2.95
Ikenaga M, Shikata J, Takemoto M, Tanaka C (2007) Clinical outcomes and complications after pedicle subtraction osteotomy for correction of thoracolumbar kyphosis. J Neurosurg Spine 6:330–336. https://doi.org/10.3171/spi.2007.6.4.8
Tang JA, Leasure JM, Smith JS, Buckley JM, Kondrashov D, Ames CP (2013) Effect of severity of rod contour on posterior rod failure in the setting of lumbar pedicle subtraction osteotomy (PSO). Neurosurgery 72:276–283. https://doi.org/10.1227/NEU.0b013e31827ba066
Yang BP, Ondra SL, Chen LA, Jung HS, Koski TR, Salehi SA (2006) Clinical and radiographic outcomes of thoracic and lumbar pedicle subtraction osteotomy for fixed sagittal imbalance. J Neurosurg Spine 5:9–17. https://doi.org/10.3171/spi.2006.5.1.9
Barton C, Noshchenko A, Patel V, Cain C, Kleck C, Burger E (2015) Risk factors for rod fracture after posterior correction of adult spinal deformity with osteotomy: a retrospective case-series. Scoliosis 10:30. https://doi.org/10.1186/s13013-015-0056-5
Liu F-Y, Wang T, Yang S-D, Wang H, Yang D-L, Ding W-Y (2016) Incidence and risk factors for proximal junctional kyphosis: a meta-analysis. Eur Spine J 25:2376–2383. https://doi.org/10.1007/s00586-016-4534-0
Kim D, Kim J, Kim D, Rhim S, Yoon S (2017) Risk factors of proximal junctional kyphosis after multilevel fusion surgery: more than 2 years follow-up data. J Korean Neurosurg Soc 60:174–180. https://doi.org/10.3340/jkns.2016.0707.014
Kim HJ, Iyer S (2016) Proximal junctional kyphosis. J Am Acad Orthop Surg 24:318–326. https://doi.org/10.5435/JAAOS-D-14-00393
Edwards CC, Bridwell KH, Patel A, Rinella AS, Berra A, Lenke LG (2004) Long adult deformity fusions to L5 and the sacrum: a matched cohort analysis. Spine (Phila Pa 1976) 29:1996–2005. https://doi.org/10.1097/01.brs.0000138272.54896.33
Shen FH, Mason JR, Shimer AL, Arlet VM (2013) Pelvic fixation for adult scoliosis. Eur Spine J 22:265–275. https://doi.org/10.1007/s00586-012-2525-3
Tsuchiya K, Bridwell KH, Kuklo TR, Lenke LG, Baldus C (2006) Minimum 5-year analysis of L5–S1 fusion using sacropelvic fixation (bilateral S1 and iliac screws) for spinal deformity. Spine (Phila Pa 1976) 31:303–308. https://doi.org/10.1097/01.brs.0000197193.81296.f1
Jain A, Brooks JT, Kebaish KM, Sponseller PD (2016) Sacral alar iliac fixation for spine deformity. JBJS Essent Surg Tech 6:1–8. https://doi.org/10.2106/JBJS.ST.15.00074
Schwab F, Patel A, Ungar B, Farcy J, Lafage V (2010) Adult spinal deformity—postoperative standing imbalance. Spine (Phila Pa 1976) 35:2224–2231. https://doi.org/10.1097/BRS.0b013e3181ee6bd4
Bari TJ, Ohrt-Nissen S, Hansen LV, Dahl B, Gehrchen M (2019) Ability of the global alignment and proportion score to predict mechanical failure following adult spinal deformity surgery—validation in 149 patients with two-year follow-up. Spine Deform 7:331–337. https://doi.org/10.1016/j.jspd.2018.08.002
Ohba T, Ebata S, Oba H, Koyama K, Yokomichi H, Haro H (2019) Predictors of poor global alignment and proportion score after surgery for adult spinal deformity. Spine (Phila Pa 1976) 44:E1136–E1143. https://doi.org/10.1097/BRS.0000000000003086
Massier JRA, Ogink PT, Schlösser TPC, Ferrone ML, Hershman SH, Cha TD et al (2019) Sagittal spinal parameters after en bloc resection of mobile spine tumors. Spine J 19:1606–1612. https://doi.org/10.1016/j.spinee.2019.05.012
Jacobs E, van Royen BJ, van Kuijk SMJ, Merk JMR, Stadhouder A, van Rhijn LW et al (2019) Prediction of mechanical complications in adult spinal deformity surgery—the GAP score versus the Schwab classification. Spine J 19:781–788. https://doi.org/10.1016/j.spinee.2018.11.013
Noh SH, Ha Y, Obeid I, Park JY, Kuh SU, Chin DK et al (2020) Modified global alignment and proportion scoring with body mass index and bone mineral density (GAPB) for improving predictions of mechanical complications after adult spinal deformity surgery. Spine J 20:776–784. https://doi.org/10.1016/j.spinee.2019.11.006
Boulay C, Tardieu C, Hecquet J, Benaim C, Mouilleseaux B, Marty C et al (2006) Sagittal alignment of spine and pelvis regulated by pelvic incidence: standard values and prediction of lordosis. Eur Spine J 15:415–422. https://doi.org/10.1007/s00586-005-0984-5
Bari TJ, Hallager DW, Tøndevold N, Karbo T, Hansen LV, Dahl B et al (2019) Moderate interrater and substantial intrarater reproducibility of the Roussouly classification system in patients with adult spinal deformity. Spine Deform 7:312–318. https://doi.org/10.1016/j.jspd.2018.08.009
Laouissat F, Scemama C, Delécrin J (2016) Does the type of sagittal spinal shape influence the clinical results of lumbar disc arthroplasty? Orthop Traumatol Surg Res 102:765–768. https://doi.org/10.1016/j.otsr.2016.05.012
Ohrt-Nissen S, Bari T, Dahl B, Gehrchen M (2018) Sagittal alignment after surgical treatment of adolescent idiopathic scoliosis—application of the Roussouly classification. Spine Deform 6:537–544. https://doi.org/10.1016/j.jspd.2018.02.001
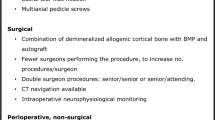
Sethi RK, Burton DC, Wright AK, Lenke LG, Cerpa M, Kelly MP et al (2019) The role of potentially modifiable factors in a standard work protocol to decrease complications in adult spinal deformity surgery: a systematic review, part 2. Spine Deform 7:684–695. https://doi.org/10.1016/j.jspd.2019.03.001
Burton DC, Sethi RK, Wright AK, Daniels AH, Ames CP, Reid DB et al (2019) The role of potentially modifiable factors in a standard work protocol to decrease complications in adult spinal deformity surgery: a systematic review, part 1. Spine Deform 7:684–695. https://doi.org/10.1016/j.jspd.2019.04.003
Hallager DW, Gehrchen M, Dahl B, Harris JA, Gudipally M, Jenkins S et al (2016) Use of supplemental short pre-contoured accessory rods and cobalt chrome alloy posterior rods reduces primary rod strain and range of motion across the pedicle subtraction osteotomy level: an in vitro biomechanical study. Spine (Phila Pa 1976) 41:E388–E395. https://doi.org/10.1097/BRS.0000000000001282
Karstensen S, Bari T, Gehrchen M, Street J, Dahl B (2016) Morbidity and mortality of complex spine surgery: a prospective cohort study in 679 patients validating the Spine AdVerse Event Severity (SAVES) system in a European population. Spine J 16:146–153. https://doi.org/10.1016/j.spinee.2015.09.051
Bari TJ, Hallager DW, Tøndevold N, Karbo T, Hansen LV, Dahl B et al (2019) Spinopelvic parameters depending on the angulation of the sacral end plate are less reproducible than other spinopelvic parameters in adult spinal deformity patients. Spine Deform 7:771–778. https://doi.org/10.1016/j.jspd.2018.12.002
Funding
No external funding was received.
Author information
Authors and Affiliations
Contributions
TJB, DWH, LVH, BD, MG: substantial contributions to the conception or design of the work. TJB: substantial contributions to the acquisition, analysis and interpretation of data. DWH: substantial contributions to the analysis and interpretation of data. TJB, DWH, LVH, BD, MG: revising the work critically for important intellectual content. TJB, DWH, LVH, BD, MG: final approval of the version to be published.
Corresponding author
Ethics declarations
Conflict of interest
MG (institutional grants from K2M and Medtronic outside of the submitted work), the remaining authors report no conflicts of interest.
Ethical approval
This study was approved by the National Health and Medical authority and The National Data Protection Agency.
Informed consent
This study includes no experimental investigation.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Bari, T.J., Hallager, D.W., Hansen, L.V. et al. Mechanical revision following pedicle subtraction osteotomy: a competing risk survival analysis in 171 consecutive adult spinal deformity patients. Spine Deform 9, 191–205 (2021). https://doi.org/10.1007/s43390-020-00195-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s43390-020-00195-1