Abstract
Study design
Observational.
Objectives
To report on the rate of major complications following spinal fusion and instrumentation to treat spinal deformity in patients with cerebral palsy (CP).
Summary of background data
Understanding the risk of major complications following the surgical treatment of spine deformities in patients with CP is critical.
Methods
A prospectively collected, multicenter database of patients with CP who had surgical correction of their spinal deformity (scoliosis or kyphosis) was reviewed for all major complications. Patients with ≥ 2 year follow-up or who died ≤ 2 years of surgery were included. A complication was defined as major if it resulted in reoperation, re-admission to the hospital, prolongation of the hospital stay, was considered life-threatening, or resulted in residual disability. Overall complication and revision rates were calculated for the perioperative (Peri-op; occurring ≤ 90 days postoperative) and delayed postoperative (Delayed; > 90 days) time periods.
Results
Two hundred and fifty-seven patients met inclusion. Seventy-eight (30%) patients had a major complication, 18 (7%) had > 1. There were 92 (36%) major complications; 64 (24.9%) occurred Peri-op. The most common Peri-op complications were wound (n = 16, 6.2%) and pulmonary issues (n = 28, 10.9%), specifically deep infections (n = 12, 4.7%) and prolonged ventilator support (n = 21, 8.2%). Delayed complications (n = 28, 10.9%) were primarily deep infections (n = 8, 3.1%) and instrumentation-related (n = 6, 2.3%). There were 42 additional surgeries for an overall unplanned return to the operating room rate of 16% (Peri-op: 8.6%, Delayed: 7.8%). Thirty-six (14.0%) reoperations were spine related surgeries (wound or instrumentation-related). Eleven (4.3%) patients died between 3 months to 5.6 years postoperatively; 4 occurred ≤ 1 year of surgery. Two deaths were directly related to the spinal deformity surgery.
Conclusion
Spinal deformity surgery in CP patients with greater than 2 years of follow-up have a postoperative major complication rate of 36% with a spine-related reoperation rate of 14.0%.
Level of evidence
Therapeutic-IV.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Cerebral Palsy (CP) is a disorder characterized by an impairment of movement that results from a non-progressive abnormality in the developing brain. Lack of control and/or spasticity of truncal muscles frequently lead to scoliosis especially when the extent of involvement is more severe. In some cases this scoliosis and pelvic obliquity may create progressive symptoms and functional impairment that may benefit from surgical correction, typically with a spinal instrumentation and fusion from T2 to the pelvis. When compared to idiopathic scoliosis, surgical intervention in the CP population is associated with higher rates of perioperative and postoperative complications [1,2,3]. This is likely due to differences in co-morbidities and surgical complexity between the two populations.
Depending on the study, complication rates in patients undergoing spinal deformity surgery ranging from 18 to 65% have been reported in the literature [3,4,5]. The wide discrepancy in rates of complications is likely based on historical data, inclusion of other neuromuscular conditions, and differences in complication criteria. Recently, Samdani et al. reported a 39% complication rate in 127 patients with CP [2]. The presence of a complication was associated with an increased length of ICU stay (7.8 days vs. 3.2).
The decision to pursue surgery in the CP patient should balance the intended outcome with the potential risk of complications. Providing accurate and up-to-date information for known complications with modern day treatment will allow for improved informed consent and better standards for reimbursement in the era of pay for performance. The purpose of this study is to report on the rate of major perioperative and delayed complications in a prospectively enrolled cohort of surgically treated spinal deformity patients with an underlying diagnosis of cerebral palsy and a minimum of 2 years follow-up after the spinal fusion procedure.
Methods
A prospectively collected (2008–2014), multicenter database of patients with CP who underwent spinal fusion and instrumentation to correct their spine deformity (scoliosis or kyphosis) was reviewed for all major complications. Patients with minimum 2 year follow-up or who died within 2 years of surgery were included. For inclusion into the database, patients had to be age 8–21 years at the time of surgery, have a diagnosis of CP with spinal deformity, and undergo a spinal fusion for a coronal curve > 50° or a kyphotic deformity from T5–T12 > 70°.
A complication was defined as major if it resulted in reoperation, re-admission to the hospital, a prolongation of the initial hospital stay, was considered life-threatening, or resulted in residual disability. A standardization manual that defined each complication was provided to all participating site research investigators and coordinators. Complications were classified into 1 of 11 categories: Death, Gastrointestinal, Instrumentation, Medical, Neurologic, Pain, Pulmonary, Pseudarthrosis, Reoperation (not otherwise categorized), Surgical Site/Incision (“wound”), and Transfusion. For the full list of complications included within these categories, see Bartley et al. [1]. If more than one related complications occurred, the most severe was the category that was counted in the overall rate. A review of all reported complications was performed first by a research team independent of the surgeon, as then by a subcommittee of study group members to provide consistency and quality assurance. In addition, a secondary review of the complications was performed to confirm if a complication met the defined “major complication” criteria. Demographic and operative data for each patient was analyzed. The deaths, major complications and reoperations were analyzed for the perioperative (occurring ≤ 90 days postoperatively) and delayed (> 90 days postoperatively) time periods. Patient caregiver reported outcomes, as assessed using the CPChild questionnaire and Health Utilities Index (HUI3), were evaluated preoperatively and 2 years postoperatively for the entire cohort as well as between those who experienced a complication and those who did not.
Results
Demographics
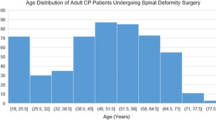
Two hundred and fifty-seven patients met the greater than 2 year follow-up inclusion criteria. The average length of follow-up was 3.3 ± 1.6 years (range 0.1–7.3 including the follow-up for those who died prior to 2 years postoperatively). There was a 67% follow-up rate with minimum 2 years. The average age at time of surgery was 14 ± 3 years. There were 135 males and 122 females. The gross motor function classification system (GMFCS) levels for the cohort were as follows: Level V: 184, Level IV: 45, Level III: 10, Level II: 5, Level I: 1, Level Unavailable: 12. One hundred and ninety (74%) patients had profound to severe mental retardation, 176 (68%) had a history of seizures, 96 (37%) had a history of pneumonia, and 137 (53%) patients required a G-tube for feeding. Scoliosis was the primary deformity in 234 patients (major curve: 86 ± 22°) and kyphosis (T2–T12 kyphosis: 79 ± 20°) was the primary deformity in 23. The average coronal deformity for the entire cohort was 82 ± 25°. The average kyphosis was 44 ± 24° from T2 to T12, and 37 ± 23° from T5 to T12. Radiographic measurements for each primary deformity, as well as for the entire cohort can be found in Table 1.
The surgical correction procedures included the following: 227 posterior spinal fusion and instrumentation (PSF) cases, 26 PSF with an anterior release, 3 combined PSF with anterior spinal fusion/instrumentation, and 1 anterior only spinal fusion with instrumentation. The majority of patients were fused proximally between T1 and T3 (94%; range C5–T9) and distally to the pelvis (91%; range L2-Ilium). For all procedures combined, the average operative time was 425 ± 174 min (range 180–1266) and the average EBL was 1763 ± 1287 cc (range 150–8500), with an average of 972 ± 904 cc (range 0–7500) of blood transfused. The average length of hospital stay was 13 ± 12 days (range 3–137) and the average length of days in the ICU was 5 ± 6 (range 0–46). All but 12 patients (95%) were admitted to the ICU postoperatively. On average, patients received ventilator support for 2.7 ± 4.2 days (range 0–39).
Major complications
Seventy-six (30%) patients had a major complication, 18 (7%) of which had 2–3 major complications. There were a total of 92 (36%) major complications, 64 (24.9%) occurred perioperatively (Table 2). The most common perioperative complications were wound healing related (n = 16, 6.2%) and pulmonary issues (n = 28, 10.9%), specifically deep infections (n = 12, 4.7%) and prolonged ventilator support (n = 21, 8.2%). Delayed complications (n = 28, 10.9%) were primarily deep infections (n = 8, 3.1%) and instrumentation related (n = 6, 2.3%). On average, major complications occurred 5.5 months postoperatively (range immediate to 5.5 years). There was no difference in the distribution of complication based on GMFCS level: Level V: Y-31% vs N-69%, Level IV: Y-24% vs N-76%, Level III: Y-40% vs N-60%, Level II: Y-20% vs N-80%, Level I: Y-0% vs N-100%, Level Unavailable: Y-25% vs N-75%; p = 0.8.
There were 42 additional surgeries for an overall unplanned return to the operating room rate of 16% (Peri-op: 8.6%, Delayed: 7.8%). Thirty-six (14.0%) surgeries were spine related, with the majority being wound (8.7%) or instrumentation related (2.7%). Table 3 summarizes the indications for the spine-related revision procedures. The single most frequent indication for reoperation was a deep infection (6.6%). Eleven (4.2%) patients died between 3 months to 5.6 years postoperatively, with 4 occurring within 1 year of surgery. Two deaths were directly related to the spinal deformity surgery and included in the major complication rate. The first death related to the spinal deformity surgery occurred 3 months postoperatively and involved a cerebral infarction due to acute hydrocephalus and E. coli meningitis. The second related death followed a viral infection 2 months after being treated for a wound infection. The causes of the non-spine surgery related deaths were varied: gastrointestinal related (3), respiratory related (2), seizure (1), and unknown (3).
Caregiver reported outcomes
Significant improvements were seen from preoperative to 2 years postoperative for the entire cohort in all CPChild domains and total score: Activities of daily living (39 ± 16 to 45 ± 17, p < 0.001), Transferring and Mobility (34 ± 17 to 45 ± 17, p < 0.001), Comfort and Emotions (75 ± 21 to 82 ± 18, p < 0.001), Communications and Social Interactions (54 ± 30 to 57 ± 28, p = 0.048), Health (56 ± 20 to 62 ± 20, p < 0.001), Overall Quality of Life (62 ± 24 to 71 ± 23, p < 0.001), and Total Score (51 ± 15 to 58 ± 15, p < 0.001). No significant difference was observed in HUI Overall Utility Score for the entire cohort from preoperative (− 0.08 ± 0.2) to 2 years (− 0.06 ± 0.2) (p = 0.2).
The change from preoperative to 2 years postoperative in all CPChild domains was not significantly different based on whether a major complication occurred or not (Table 4). However, the complication group had a HUI score that worsened slightly (− 0.08 to − 0.10), whereas the no complication group showed a modest improvement (− 0.08 to − 0.03) p = 0.035.
Discussion
Surgery for scoliosis in patients with CP can come with high risks due to the comorbidities associated with this condition. Having current and accurate information regarding major complications following spinal fusion and instrumentation for significant scoliosis and/or kyphosis in the CP patient is important in weighing the costs against the benefits when educating a family on whether to pursue surgery for patients in this population. Therefore, the current study reports on the major complications, both perioperative and delayed, in a large prospectively collected series of surgically treated patients with CP and spinal deformity.
This study is not without limitations. As these patients have frequent comorbidities, it is challenging to identify the relative contribution of the surgery versus the patient’s overall health to any given postoperative complication. Whereas some major complications are clearly associated with the surgery (e.g., broken rod), others may be partially attributable to a pre-existing condition (e.g., failed extubation in a patient with limited respiratory function). Additionally, this study was a multicenter study with each site responsible for self-reporting postoperative complications. However, to help reduce the variability in reporting, a standardization manual was provided to all sites and a quality assurance review was conducted by a research team independent of the surgeon, as well as by a subcommittee of study group members to provide consistency and quality assurance. Finally, all complications were again reviewed by the authors to confirm the “major” complication categorization.
Of the 257 patients, 76 patients (30%) experienced 92 major complications giving an overall rate of 36% (25% perioperative), with a reoperation rate of 16%. There was a 14% reoperation rate for spine-related revisions. The majority of all complications were pulmonary (12.1%), wound (9.7%), or medical (5.8%) related.
The risk of pulmonary problems in neuromuscular patients following spinal surgery is well known and includes respiratory failure, aspiration, pneumonia, pneumothorax, or pleural effusion [2, 6, 7]. Rates between 17 and 50% have been reported in the literature [6,7,8,9]. Scoliosis surgery has been shown to produce a transient decrease in vital capacity in all patients [10]. Therefore, neuromuscular patients with pre-existing pulmonary compromise should be identified before surgery to optimize lung function. These patients will be at particular risk for requiring prolonged mechanical ventilation. Aggressive management by the intensive care unit with protocols for early extubation and the use of non-invasive ventilation (BIPAP and NCPAP) have demonstrated benefits in the prevention of respiratory failure [11, 12]. Pre-operative assessment by pulmonology to optimize pulmonary function before proceeding with surgery may also help minimize some of this risk.
The second most common complication reported in our study was wound related (9.7%). This is significantly higher than the published 1–2% rate seen in the AIS population [1, 13,14,15,16]. They were primarily deep wound infections but also included superficial infections, dehiscence, seroma, hematoma, and prolonged drainage; all required a reoperation. While the majority occurred in the perioperative period (6.2%), a significant portion was delayed (3.5%). Our rate of wound complications was similar to those already reported in the literature for CP scoliosis [6, 17, 18]. Sponseller et al. reported a 10% infection rate in a retrospective review of 157 CP patients treated for scoliosis [19]. They found higher preoperative white blood cell count and the use of unit rods to be risk factors for the development of a postoperative infection.
Medical complications occurred in 5.8% of patients and represent a diverse group of problems. They include: hypotension or shock, myocardial infarction, urinary tract infection, deep vein thrombosis and others. While difficult to analyze individually, grouped together they demonstrate the complexity of the postoperative care of the CP patient. Not routinely reported in the literature, major medical complications in the AIS population are exceedingly rare with a reported incidence of 0.06% in a recent publication1. Appropriate medical management by the ICU or medical specialists may be needed and in some cases outweigh the postoperative surgical management.
The most concerning complication reported in this study is the mortality following surgery. There were 11 deaths that occurred after the time of spine surgery, 4 of which occurred within 1 year. Only 2 of the deaths were known to be directly related to the spine surgery. One occurred 3 months postoperatively and included cerebral infarction due to acute hydrocephalus and E. coli meningitis. The other death was related to an infection 2 months after being treated for a wound infection. Very few reports exist on the mortality following spinal deformity surgery. Barsdorf et al. reported a 1.6% in-hospital mortality rate for pediatric patients undergoing correction of neuromuscular spinal deformity [20]. This rate, however, was not specific to the CP population. Tsirikos et al. reported a 1% perioperative mortality rate following spinal surgery in patients with CP [21]. This is similar to our rate of 0.8% that we found directly related to surgical treatment. The other important issue our findings open to consideration is the general survivorship of the CP patient that undergoes scoliosis. Approximately 4% of the 257 patients analyzed died following their surgery timing of which ranged from the perioperative period to 5 years postoperative. This was significantly lower than the 28% mortality rate Sitoula et al. found [22]. Their patients were younger at the time of surgery with a mean age of 8.3 years suggesting a more severe patient population.
Conclusion
Spinal surgery for CP can have significant major complications. When preparing patients and their families, having an accurate understanding of complication rates following spinal fusion and instrumentation for CP is of great importance. In addition, many of these risks may be reduced by optimizing patients’ overall health [23]. While a formal process has not been employed by this multicenter group, many centers will refer patients for pulmonary, nutritional and anesthetic assessment before any procedure is undertaken. In some cases, the risks of complications may be too extreme to consider pursuing a surgical intervention. With a major complication rate of 36% and a spine-related reoperation rate of 14%, future studies will be needed to better understand the risk and methods to mitigate these risks.
Key Points
-
In patients with CP undergoing spinal fusion and instrumentation for a spinal deformity, there was a major perioperative complication rate of 36% with a spine-related reoperation rate of 14%.
-
Within the perioperative period, the major complication rate was 25% and the reoperation rate was 8.6%. The majority of these complications were pulmonary (11%), wound (6%), or medical (4%) related.
-
The rate of delayed major complications was 11%, which were primarily deep infections (3%) and instrumentation-related (2%).
-
Spinal surgery for CP can have significant major complications and it is of great importance to have an accurate understanding of the complication rates when preparing patients and their families for the procedure.
References
Bartley CE, Yaszay B, Bastrom TP et al (2017) Perioperative and delayed major complications following surgical treatment of adolescent idiopathic scoliosis. J Bone Joint Surg Am 99:1206–1212
Samdani AF, Belin EJ, Bennett JT et al (2016) Major perioperative complications after spine surgery in patients with cerebral palsy: assessment of risk factors. Eur Spine J 25:795–800
Sharma S, Wu C, Andersen T et al (2013) Prevalence of complications in neuromuscular scoliosis surgery: a literature meta-analysis from the past 15 years. Eur Spine J 22:1230–1249
Master DL, Son-Hing JP, Poe-Kochert C et al (2011) Risk factors for major complications after surgery for neuromuscular scoliosis. Spine (Phila Pa 1976) 36:564–571
Rumalla K, Yarbrough CK, Pugely AJ et al (2016) Spinal fusion for pediatric neuromuscular scoliosis: national trends, complications, and in-hospital outcomes. J Neurosurg Spine 25:500–508
Modi HN, Suh SW, Yang JH et al (2009) Surgical complications in neuromuscular scoliosis operated with posterior- only approach using pedicle screw fixation. Scoliosis 4:11
Mohamad F, Parent S, Pawelek J et al (2007) Perioperative complications after surgical correction in neuromuscular scoliosis. J Pediatr Orthop 27:392–397
Miyanji F, Nasto LA, Sponseller PD et al (2018) Assessing the risk-benefit ratio of scoliosis surgery in cerebral palsy: surgery is worth it. J Bone Joint Surg Am 100:556–563
Toovey R, Harvey A, Johnson M et al (2017) Outcomes after scoliosis surgery for children with cerebral palsy: a systematic review. Dev Med Child Neurol 59:690–698
Yuan N, Fraire JA, Margetis MM et al (2005) The effect of scoliosis surgery on lung function in the immediate postoperative period. Spine (Phila Pa 1976) 30:2182–2185
Ornico SR, Lobo SM, Sanches HS et al (2013) Noninvasive ventilation immediately after extubation improves weaning outcome after acute respiratory failure: a randomized controlled trial. Crit Care 17:R39
Burns KE, Adhikari NK, Keenan SP et al (2009) Use of non-invasive ventilation to wean critically ill adults off invasive ventilation: meta-analysis and systematic review. BMJ 338:b1574
Marks MC, Newton PO, Bastrom TP et al (2013) Surgical site infection in adolescent idiopathic scoliosis surgery. Spine Deform 1:352–358
Lamberet A, Violas P, Buffet-Bataillon S et al (2018) Postoperative spinal implant infections in children: risk factors, characteristics and outcome. Pediatr Infect Dis J 37:511–513
Kamath VH, Cheung JP, Mak KC et al (2016) Antimicrobial prophylaxis to prevent surgical site infection in adolescent idiopathic scoliosis patients undergoing posterior spinal fusion: 2 doses versus antibiotics till drain removal. Eur Spine J 25:3242–3248
Webb ML, Lukasiewicz AM, Samuel AM et al (2015) Overall Similar Infection Rates Reported in the Physician-reported Scoliosis Research Society Database and the Chart-abstracted American College of Surgeons National Surgical Quality Improvement Program Database. Spine (Phila Pa 1976) 40:1431–1435
Aleissa S, Parsons D, Grant J et al (2011) Deep wound infection following pediatric scoliosis surgery: incidence and analysis of risk factors. Can J Surg 54:263–269
Szoke G, Lipton G, Miller F et al (1998) Wound infection after spinal fusion in children with cerebral palsy. J Pediatr Orthop 18:727–733
Sponseller PD, Shah SA, Abel MF et al (2010) Infection rate after spine surgery in cerebral palsy is high and impairs results: multicenter analysis of risk factors and treatment. Clin Orthop Relat Res 468:711–716
Barsdorf AI, Sproule DM, Kaufmann P (2010) Scoliosis surgery in children with neuromuscular disease: findings from the US National Inpatient Sample, 1997 to 2003. Arch Neurol 67:231–235
Tsirikos AI, Lipton G, Chang WN et al (2008) Surgical correction of scoliosis in pediatric patients with cerebral palsy using the unit rod instrumentation. Spine (Phila Pa 1976) 33:1133–1140
Sitoula P, Holmes L Jr, Sees J et al (2016) The long-term outcome of early spine fusion for scoliosis in children with cerebral palsy. Clin Spine Surg 29:E406–E412
Halawi MJ, Lark RK, Fitch RD (2015) Neuromuscular scoliosis: current concepts. Orthopedics 38:e452–e456
Acknowledgements
Harms Study Group Investigators: Aaron Buckland, MD; New York University. Amer Samdani, MD; Shriners Hospitals for Children—Philadelphia. Amit Jain, MD; Johns Hopkins Hospital. Baron Lonner, MD; Mount Sinai Hospital. Benjamin Roye, MD; Columbia University. Burt Yaszay, MD; Rady Children’s Hospital. Chris Reilly, MD; BC Children’s Hospital. Daniel Hedequist, MD; Boston Children’s Hospital. Daniel Sucato, MD; Texas Scottish Rite Hospital. David Clements, MD; Cooper Bone & Joint Institute New Jersey. Firoz Miyanji, MD; BC Children’s Hospital. Harry Shufflebarger, MD; Nicklaus Children’s Hospital. Jack Flynn, MD; Children’s Hospital of Philadelphia. Jahangir Asghar, MD; Cantor Spine Institute. Jean Marc Mac Thiong, MD; CHU Sainte-Justine. Joshua Pahys, MD; Shriners Hospitals for Children—Philadelphia. Juergen Harms, MD; Klinikum Karlsbad-Langensteinbach, Karlsbad. Keith Bachmann, MD; University of Virginia. Larry Lenke, MD; Columbia University. Mark Abel, MD; University of Virginia. Michael Glotzbecker, MD; Boston Children’s Hospital. Michael Kelly, MD; Washington University. Michael Vitale, MD; Columbia University. Michelle Marks, PT, MA; Setting Scoliosis Straight Foundation. Munish Gupta, MD; Washington University. Nicholas Fletcher, MD; Emory University. Patrick Cahill, MD; Children’s Hospital of Philadelphia. Paul Sponseller, MD; Johns Hopkins Hospital. Peter Gabos, MD: Nemours/Alfred I. duPont Hospital for Children. Peter Newton, MD; Rady Children’s Hospital. Peter Sturm, MD; Cincinnati Children’s Hospital. Randal Betz, MD; Institute for Spine & Scoliosiscba. Ron Lehman, MD; Columbia University. Stefan Parent, MD: CHU Sainte-Justine. Stephen George, MD; Nicklaus Children’s Hospital. Steven Hwang, MD; Shriners Hospitals for Children—Philadelphia. Suken Shah, MD; Nemours/Alfred I. duPont Hospital for Children. Tom Errico, MD; Nicklaus Children’s Hospital. Vidyadhar Upasani, MD; Rady Children’s Hospital
Funding
This study was supported in part by grants to the Setting Scoliosis Straight Foundation from DePuy Synthes Spine, EOS imaging, K2M, Medtronic, NuVasive and Zimmer Biomet in support of Harms Study Group research.
Author information
Authors and Affiliations
Contributions
Conception or design of the work; or Acquisition, analysis, or interpretation of data for the work: BY, CEB, PDS, MA, PJC, SAS, FM, AFS, CD, PON; Drafting or critically revising the work: BY, CEB, PDS, MA, PJC, SAS, FM, AFS, CD, PON; Final approval of the version to be published: BY, CEB, PDS, MA, PJC, SAS, FM, AFS, CD, PON.
Corresponding author
Ethics declarations
Ethics approval
This study has been approved by the IRB.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations
Rights and permissions
About this article
Cite this article
Yaszay, B., Bartley, C.E., Sponseller, P.D. et al. Major complications following surgical correction of spine deformity in 257 patients with cerebral palsy. Spine Deform 8, 1305–1312 (2020). https://doi.org/10.1007/s43390-020-00165-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s43390-020-00165-7