Abstract
Study design
Basic science.
Objective
Investigate the ability of local applicaiton of vancomycin, either in powder form or suspended within poly(lactic-co-glycolic acid) microspheres (MS), to treat infection using a rat spinal model.
Summary of background data
Surgical site infections (SSIs) are a serious complication after spine surgery and are associated with high morbidity and mortality and often caused my coagulase negative staphylococci. A comprehensive approach to reduce SSIs has been recommended including the use of topical vancomycin. Animal and human studies have shown improved control of infection with local compared to systemic antibiotics.
Methods
K-wires seeded with methicillin-resistant Staphylococcus epidermidis RP62A (MRSE) were treated with vancomycin powder, carboxymethylcellulose sodium salt (CMC) (microsphere carrier), vancomycin powder, blank MS or vancomycin-loaded MS for 24 or 48 h in vitro after which bacteria were enumerated. In addition, a spinal instrumentation model was developed in rats with a bacterial seeded K-wire implanted into the right side of L4 and L5. Rats underwent no treatment or were treated locally with either vancomycin powder, blank MS or vancomycin-loaded MS. After 8 weeks, the K-wire, bone, soft tissue and wire fastener were cultured and results analyzed.
Results
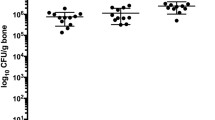
Vancomycin powder and vancomycin-loaded MS resulted in significantly fewer bacteria remaining in vitro than did CMC. Vancomycin powder- treated animals’ cultures were significantly lower than all other groups (P < 0.0001) with negative culture results, except for one animal. The vancomycin-loaded MS-treated animals had lower bone bacterial counts than the controls (P < 0.0279); blank MS-treated animals had no differences in bacterial densities when compared to non-treated animals.
Conclusion
Vancomycin powder and vancomycin-loaded MS were active against MRSE in vitro, in a rat MRSE implant model; however, vancomycin MS were inferior to the topical vancomycin powder. Vancomycin powder prevented MRSE infection in a rat spinal implant infection model.





Similar content being viewed by others
References
Hey HWD, Thiam DW, Koh ZSD et al (2017) Is intraoperative local vancomycin powder the answer to surgical site infections in spine surgery? Spine 42:267–274
Lee GI, Bak KH, Chun HJ et al (2016) Effect of using local intrawound vancomycin powder in addition to intravenous antibiotics in posterior lumbar surgery: midterm result in a single-center study. Korean J Spine 13:47
Agarwal N, Agarwal P, Querry A et al (2018) Implementation of an infection prevention bundle and increased physician awareness improves surgical outcomes and reduces costs associated with spine surgery. J Neurosurg 29:108–114
Vitale MG, Riedel MD, Glotzbecker MP et al (2013) Building consensus: development of a best practice guideline (BPG) for surgical site infection (SSI) prevention in high-risk pediatric spine surgery. J Pediatr Orthop 33:471–478
Gerometta A, Olaverri JCR, Bitan F (2012) Infections in spinal instrumentation. Int Orthop 36:457–464
Kang DG, Holekamp TF, Wagner SC et al (2015) Intrasite vancomycin powder for the prevention of surgical site infection in spine surgery: a systematic literature review. Spine J 15:762–770
Park HY, Sheppard W, Smith R et al (2018) The combined administration of vancomycin IV, standard prophylactic antibiotics, and vancomycin powder in spinal instrumentation surgery: does the routine use affect infection rates and bacterial resistance? J Spine Surg 4:173
Takeuchi M, Wakao N, Kamiya M et al (2018) A double-blind randomized controlled trial of the local application of vancomycin versus ampicillin powder into the operative field for thoracic and/or lumbar fusions. J Neurosurg Spine 1:1–7
Texakalidis P, Lu VM, Yolcu Y et al (2018) Impact of powdered vancomycin on preventing durgical dite infections in neurosurgery: a systematic review and meta-analysis. Neurosurg 84:569–580
Xie LL, Zhu J, Yang MS et al (2017) Effect of intra-wound vancomycin for spinal surgery: a systematic review and meta-analysis. Orthop Surg 9:350–358
Clark A, Milbrandt TA, Hilt JZ et al (2014) Retention of insulin-like growth factor I bioactivity during the fabrication of sintered polymeric scaffolds. Biomed Mater 9:025015
Raiche A, Puleo D (2006) Modulated release of bioactive protein from multilayered blended PLGA coatings. Int J Pharm 311:40–49
Hu Y, Hegde V, Johansen D et al (2017) Combinatory antibiotic therapy increases rate of bacterial kill but not final outcome in a novel mouse model of Staphylococcus aureus spinal implant infection. PLoS ONE 12:e0173019
Brown ME, Zou Y, Peyyala R et al (2018) Testing of a bioactive, moldable bone graft substitute in an infected, critically sized segmental defect model. J Biomed Mater Res B 106:1878–1886
Liu G, Chen S, Fang J et al (2016) Vancomycin microspheres reduce postoperative spine infection in an in vivo rabbit model. BMC Pharmacol Toxicol 17:61
Andersen NJ (2014) Microsphere spray system for wound coverage. Thesis, Biomedical Engineering, University of Kentucky
Armaghani SJ, Menge TJ, Lovejoy SA et al (2014) Safety of topical vancomycin for pediatric spinal deformity: nontoxic serum levels with supratherapeutic drain levels. Spine 39:1683–1687
Miksić NG (2013) Spinal infections with and without hardware: the viewpoint of an infectious disease specialist. Eur J Orthop Surg Traumatol 23:21–28
Acknowledgements
Mayo Clinic Endowment for Pediatric Infectious Diseases. We would like to acknowledge Scott Gamb (Mayo Clinic) for performing biofilm imaging. IRB approval was not necessary for this study. Level 2 FDA approved.
Funding
There was no outside funding for this study. No funding was received from the National Institutes of Health (NIH); Wellcome Trust; Howard Hughes Medical Institute (HHMI).
Author information
Authors and Affiliations
Contributions
MJK: experimental design, execution, data analysis, drafting manuscript and review and approval of manuscript. CZ: experimental design, execution, drafting portions of the manuscript and review of manuscript and approval of manuscript. JNM: experimental design and statistical analysis of data, manuscript review and approval of manuscript. NJK: manufacturing and analyzing the release of vancomycin-loaded PLGA microspheres, drafting portions of the manuscript and manuscript review and approval of manuscript. DAP: oversight of the manufacturing and analyzing the release of vancomycin-loaded PLGA microspheres, drafting portions of the manuscript and manuscript review and approval of manuscript. AJvW, TGB, and ANL: experimental design and manuscript review and approval of manuscript. RP: co-investigator, experimental design, oversight of execution and manuscript review and approval of manuscript. TAM: principal investigator, experimental design, oversight of execution and manuscript review and approval of manuscript.
Corresponding author
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations
Rights and permissions
About this article
Cite this article
Karau, M.J., Zhang, C., Mandrekar, J.N. et al. Topical vancomycin for treatment of methicillin-resistant Staphylococcus epidermidis infection in a rat spinal implant model. Spine Deform 8, 553–559 (2020). https://doi.org/10.1007/s43390-020-00087-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s43390-020-00087-4