Abstract
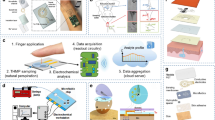
Sweat, as a biofluid with the potential for noninvasive collection, provides profound insights into human health conditions, because it contains various chemicals and information to be utilized for the monitoring of well-being, stress levels, exercise, and nutrition. Recently, wearable sweat sensors have been developed as a promising substitute to conventional laboratory sweat detection methods. Such sensors are promising to realize low-cost, real-time, in situ sweat measurements, and provide great opportunities for health status evaluation analysis based on personalized big data. This review first presents an overview of wearable sweat sensors from the perspective of basic components, including materials and structures for specific sensing applications and modalities. Current strategies and specific methods of the fabrication of wearable power management are also summarized. Finally, current challenges and future directions of wearable sweat sensors are discussed.







Similar content being viewed by others
References
Yu Y, Suh MJ, Sikorski P et al (2014) Urine sample preparation in 96-well filter plates for quantitative clinical proteomics. Anal Chem 86(11):5470–5477. https://doi.org/10.1021/ac5008317
Torrente-Rodríguez RM, Lukas H, Tu J et al (2020) SARS-CoV-2 RapidPlex: a graphene-based multiplexed telemedicine platform for rapid and low-cost COVID-19 diagnosis and monitoring. Matter 3(6):1981–1998. https://doi.org/10.1016/j.matt.2020.09.027
Farandos NM, Yetisen AK, Monteiro MJ et al (2015) Contact lens sensors in ocular diagnostics. Adv Healthcare Mater 4(6):792–810. https://doi.org/10.1002/adhm.201400504
Kim J, Sempionatto JR, Imani S et al (2018) Simultaneous monitoring of sweat and interstitial fluid using a single wearable biosensor platform. Adv Sci 5(10):1800880. https://doi.org/10.1002/advs.201800880
Kim J, Campbell AS, de Ávila BEF et al (2019) Wearable biosensors for healthcare monitoring. Nat Biotechnol 37(4):389–406. https://doi.org/10.1038/s41587-019-0045-y
Jessen C (2001) Temperature regulation in humans and other mammals. Springer, Berlin
Xu K, Lu Y, Takei K (2021) Flexible hybrid sensor systems with feedback functions. Adv Funct Mater 31(39):2007436. https://doi.org/10.1002/adfm.202007436
Lu Y, Fujita Y, Honda S et al (2021) Wireless and flexible skin moisture and temperature sensor sheets toward the study of thermoregulator center. Adv Healthcare Mater 10(17):2100103. https://doi.org/10.1002/adhm.202100103
Yang G, Deng J, Pang G et al (2018) An IoT-enabled stroke rehabilitation system based on smart wearable armband and machine learning. IEEE J Transl Eng Health Med 6:1–10. https://doi.org/10.1109/JTEHM.2018.2822681
Xu K, Lu Y, Takei K (2019) Multifunctional skin-inspired flexible sensor systems for wearable electronics. Adv Mater Technol 4(3):1800628. https://doi.org/10.1002/admt.201800628
Heng W, Pang G, Xu F et al (2019) Flexible insole sensors with stably connected electrodes for gait phase detection. Sensors 19(23):5197. https://doi.org/10.3390/s19235197
Yang G, Pang G, Pang Z et al (2019) Non-invasive flexible and stretchable wearable sensors with nano-based enhancement for chronic disease care. IEEE Rev Biomed Eng 12:34–71. https://doi.org/10.1109/RBME.2018.2887301
Yang Y, Song Y, Bo X et al (2020) A laser-engraved wearable sensor for sensitive detection of uric acid and tyrosine in sweat. Nat Biotechnol 38(2):217–224. https://doi.org/10.1038/s41587-019-0321-x
Rogers JA, Someya T, Huang Y (2010) Materials and mechanics for stretchable electronics. Science 327(5973):1603–1607. https://doi.org/10.1126/science.1182383
Wang G, Zhang S, Dong S et al (2019) Stretchable optical sensing patch system integrated heart rate, pulse oxygen saturation, and sweat pH detection. IEEE Trans Biomed Eng 66(4):1000–1005. https://doi.org/10.1109/TBME.2018.2866151
Wang C, Wang C, Huang Z et al (2018) Materials and structures toward soft electronics. Adv Mater 30(50):1801368. https://doi.org/10.1002/adma.201801368
Li BM, Kim I, Zhou Y et al (2019) Kirigami-inspired textile electronics: K.I.T.E. Adv Mater Technol 4(11):1900511. https://doi.org/10.1002/admt.201900511
Ning X, Wang X, Zhang Y et al (2018) Assembly of advanced materials into 3D functional structures by methods inspired by origami and kirigami: a review. Adv Mater Interf 5(13):1800284. https://doi.org/10.1002/admi.201800284
He W, Wang C, Wang H et al (2019) Integrated textile sensor patch for real-time and multiplex sweat analysis. Sci Adv 5(11):eaax0649. https://doi.org/10.1126/sciadv.aax0649
Xu F, Zhu Y (2012) Highly conductive and stretchable silver nanowire conductors. Adv Mater 24(37):5117–5122. https://doi.org/10.1002/adma.201201886
Kaltenbrunner M, Sekitani T, Reeder J et al (2013) An ultra-lightweight design for imperceptible plastic electronics. Nature 499(7459):458–463. https://doi.org/10.1038/nature12314
Zhang H, Xiang L, Yang Y et al (2018) High-performance carbon nanotube complementary electronics and integrated sensor systems on ultrathin plastic foil. ACS Nano 12(3):2773–2779. https://doi.org/10.1021/acsnano.7b09145
Wang L, Wang L, Zhang Y et al (2018) Weaving sensing fibers into electrochemical fabric for real-time health monitoring. Adv Funct Mater 28(42):1804456. https://doi.org/10.1002/adfm.201804456
Chan EP, Smith EJ, Hayward RC et al (2008) Surface wrinkles for smart adhesion. Adv Mater 20(4):711–716. https://doi.org/10.1002/adma.200701530
Kim K, Kim SU, Choi S et al (2020) High-definition optophysical image construction using mosaics of pixelated wrinkles. Adv Sci 7(24):2002134. https://doi.org/10.1002/advs.202002134
Toi PT, Trung TQ, Dang TML et al (2019) Highly electrocatalytic, durable, and stretchable nanohybrid fiber for on-body sweat glucose detection. ACS Appl Mater Interf 11(11):10707–10717. https://doi.org/10.1021/acsami.8b20583
Mohan AMV, Kim N, Gu Y et al (2017) Merging of thin- and thick-film fabrication technologies: toward soft stretchable “island–bridge” devices. Adv Mater Technol 2(4):1600284. https://doi.org/10.1002/admt.201600284
Song Z, Ma T, Tang R et al (2014) Origami lithium-ion batteries Nat Commun 5(1):1–6. https://doi.org/10.1038/ncomms4140
Hojaiji H, Zhao Y, Gong MC et al (2020) An autonomous wearable system for diurnal sweat biomarker data acquisition. Lab Chip 20(24):4582–4591. https://doi.org/10.1039/D0LC00820F
Heng W, Yang G, Pang G et al (2021) Fluid-driven soft CoboSkin for safer human–robot collaboration: fabrication and adaptation. Adv Intell Syst 3(3):2000038. https://doi.org/10.1002/aisy.202000038
Pang G, Yang G, Heng W et al (2021) CoboSkin: soft robot skin with variable stiffness for safer human–robot collaboration. IEEE Trans Ind Electron 68(4):3303–3314. https://doi.org/10.1109/TIE.2020.2978728
Huang X, Liu Y, Chen K et al (2014) Stretchable, wireless sensors and functional substrates for epidermal characterization of sweat. Small 10(15):3083–3090. https://doi.org/10.1002/smll.201400483
Ding R, Lisak G (2019) Sponge-based microfluidic sampling for potentiometric ion sensing. Anal Chim Acta 1091:103–111. https://doi.org/10.1016/j.aca.2019.09.024
Xu K, Lu Y, Yamaguchi T et al (2019) Highly precise multifunctional thermal management-based flexible sensing sheets. ACS Nano 13(12):14348–14356. https://doi.org/10.1021/acsnano.9b07805
Lu Y, Xu K, Yang MQ et al (2021) Highly stable Pd/HNb3O8-based flexible humidity sensor for perdurable wireless wearable applications. Nanoscale Horiz 6(3):260–270. https://doi.org/10.1039/D0NH00594K
Imani S, Bandodkar AJ, Mohan AMV et al (2016) A wearable chemical–electrophysiological hybrid biosensing system for real-time health and fitness monitoring. Nat Commun 7(1):1–7. https://doi.org/10.1038/ncomms11650
Nakata S, Shiomi M, Fujita Y et al (2018) A wearable pH sensor with high sensitivity based on a flexible charge-coupled device. Nat Electron 1(11):596–603. https://doi.org/10.1038/s41928-018-0162-5
Xu K, Fujita Y, Lu Y et al (2021) A wearable body condition sensor system with wireless feedback alarm functions. Adv Mater 33(18):2008701. https://doi.org/10.1002/adma.202008701
Yang H, Xu K, Xu C et al (2019) Femtosecond laser fabricated elastomeric superhydrophobic surface with stretching-enhanced water repellency. Nanoscale Res Lett 14(1):1–10. https://doi.org/10.1186/s11671-019-3140-6
Reeder JT, Choi J, Xue Y et al (2019) Waterproof, electronics-enabled, epidermal microfluidic devices for sweat collection, biomarker analysis, and thermography in aquatic settings. Sci Adv 5(1):eaau6356. https://doi.org/10.1126/sciadv.aau6356
Zhao Y, Wang B, Hojaiji H et al (2020) A wearable freestanding electrochemical sensing system. Sci Adv 6(12):eaaz0007. https://doi.org/10.1126/sciadv.aaz0007
Zhao Z, Li Q, Chen L et al (2021) A thread/fabric-based band as a flexible and wearable microfluidic device for sweat sensing and monitoring. Lab Chip 21(5):916–932. https://doi.org/10.1039/D0LC01075H
Xu K, Zhou R, Takei K et al (2019) Toward flexible surface-enhanced Raman scattering (SERS) sensors for point-of-care diagnostics. Adv Sci 6(16):1900925. https://doi.org/10.1002/advs.201900925
Li H, Cheng F, Robledo-Lara JA et al (2020) Fabrication of paper-based devices for in vitro tissue modeling. Bio-Des Manuf 3:252–265. https://doi.org/10.1007/s42242-020-00077-5
Liang B, Cao Q, Mao X et al (2021) An integrated paper-based microfluidic device for real-time sweat potassium monitoring. IEEE Sens J 21(8):9642–9648. https://doi.org/10.1109/JSEN.2020.3009327
Li M, Wang L, Liu R et al (2021) A highly integrated sensing paper for wearable electrochemical sweat analysis. Biosens Bioelectron 174:112828. https://doi.org/10.1016/j.bios.2020.112828
Sato K, Kang WH, Saga K et al (1989) Biology of sweat glands and their disorders. I. Normal sweat gland function. J Am Acad Dermatol 20:537–563. https://doi.org/10.1016/S0190-9622(89)70063-3
Yang Y, Gao W (2019) Wearable and flexible electronics for continuous molecular monitoring. Chem Soc Rev 48(6):1465–1491. https://doi.org/10.1039/C7CS00730B
Lee H, Choi TK, Lee YB et al (2016) A graphene-based electrochemical device with thermoresponsive microneedles for diabetes monitoring and therapy. Nat Nanotechnol 11(6):566–572. https://doi.org/10.1038/nnano.2016.38
Zhang J, Xu J, Lim J et al (2021) Wearable glucose monitoring and implantable drug delivery systems for diabetes management. Adv Healthcare Mater 10(17):2100194. https://doi.org/10.1002/adhm.202100194
Kim SB, Lee K, Raj MS et al (2018) Soft, skin-interfaced microfluidic systems with wireless, battery-free electronics for digital, real-time tracking of sweat loss and electrolyte composition. Small 14(45):1802876. https://doi.org/10.1002/smll.201802876
Sempionatto JR, Lin M, Yin L et al (2021) An epidermal patch for the simultaneous monitoring of haemodynamic and metabolic biomarkers. Nat Biomed Eng 5:737–748. https://doi.org/10.1038/s41551-021-00685-1
Kidwell DA, Holland JC, Athanaselis S (1998) Testing for drugs of abuse in saliva and sweat. J Chromatogr B Biomed Sci Appl 713(1):111–135. https://doi.org/10.1016/S0378-4347(97)00572-0
Torrente-Rodríguez RM, Tu J, Yang Y et al (2020) Investigation of cortisol dynamics in human sweat using a graphene-based wireless mHealth system. Matter 2(4):921–937. https://doi.org/10.1016/j.matt.2020.01.021
Madhu S, Anthuuvan AJ, Ramasamy S et al (2020) ZnO nanorod integrated flexible carbon fibers for sweat cortisol detection. ACS Appl Electron Mater 2(2):499–509. https://doi.org/10.1021/acsaelm.9b00730
Amjadi M, Kyung KU, Park I et al (2016) Stretchable, skin-mountable, and wearable strain sensors and their potential applications: a review. Adv Funct Mater 26(11):1678–1698. https://doi.org/10.1002/adfm.201504755
Zhou W, Yao S, Wang H et al (2020) Gas-permeable, ultrathin, stretchable epidermal electronics with porous electrodes. ACS Nano 14(5):5798–5805. https://doi.org/10.1021/acsnano.0c00906
Yu Y, Nyein HYY, Gao W et al (2020) Flexible electrochemical bioelectronics: the rise of in situ bioanalysis. Adv Mater 32(15):1902083. https://doi.org/10.1002/adma.201902083
Bariya M, Nyein HYY, Javey A (2018) Wearable sweat sensors Nat Electron 1(3):160–171. https://doi.org/10.1038/s41928-018-0043-y
Parrilla M, Cuartero M, Crespo GA (2019) Wearable potentiometric ion sensors. TrAC Trends Anal Chem 110:303–320. https://doi.org/10.1016/j.trac.2018.11.024
Zhai Q, Yap LW, Wang R et al (2020) Vertically aligned gold nanowires as stretchable and wearable epidermal ion-selective electrode for noninvasive multiplexed sweat analysis. Anal Chem 92(6):4647–4655. https://doi.org/10.1021/acs.analchem.0c00274
Oh SY, Hong SY, Jeong YR et al (2018) Skin-attachable, stretchable electrochemical sweat sensor for glucose and pH detection. ACS Appl Mater Interf 10(16):13729–13740. https://doi.org/10.1021/acsami.8b03342
Bai YF, Xu TB, Luong JHT et al (2014) Direct electron transfer of glucose oxidase-boron doped diamond interface: a new solution for a classical problem. Anal Chem 86(10):4910–4918. https://doi.org/10.1021/ac501143e
Hui X, Sharifuzzaman M, Sharma S et al (2020) High-performance flexible electrochemical heavy metal sensor based on layer-by-layer assembly of Ti3C2Tx /MWNTs nanocomposites for noninvasive detection of copper and zinc ions in human biofluids. ACS Appl Mater Interf 12(43):48928–48937. https://doi.org/10.1021/acsami.0c12239
Kinnamon D, Ghanta R, Lin KC et al (2017) Portable biosensor for monitoring cortisol in low-volume perspired human sweat. Sci Rep 7(1):13312. https://doi.org/10.1038/s41598-017-13684-7
Ganguly A, Lin KC, Muthukumar S et al (2021) Autonomous, real-time monitoring electrochemical aptasensor for circadian tracking of cortisol hormone in sub-microliter volumes of passively eluted human sweat. ACS Sens 6(1):63–72. https://doi.org/10.1021/acssensors.0c01754
Gao W, Emaminejad S, Nyein HYY et al (2016) Fully integrated wearable sensor arrays for multiplexed in situ perspiration analysis. Nature 529(7587):509–514. https://doi.org/10.1038/nature16521
Emaminejad S, Gao W, Wu E et al (2017) Autonomous sweat extraction and analysis applied to cystic fibrosis and glucose monitoring using a fully integrated wearable platform. Proc Natl Acad Sci 114(18):4625–4630. https://doi.org/10.1073/pnas.1701740114
Anastasova S, Crewther B, Bembnowicz P et al (2017) A wearable multisensing patch for continuous sweat monitoring. Biosens Bioelectron 93:139–145. https://doi.org/10.1016/j.bios.2016.09.038
Guinovart T, Bandodkar AJ, Windmiller JR et al (2013) A potentiometric tattoo sensor for monitoring ammonium in sweat. Analyst 138(22):7031–7038. https://doi.org/10.1039/C3AN01672B
Nyein HYY, Gao W, Shahpar Z et al (2016) A wearable electrochemical platform for noninvasive simultaneous monitoring of Ca2+ and pH. ACS Nano 10(7):7216–7224. https://doi.org/10.1021/acsnano.6b04005
Amatore C, Szunerits S, Thouin L (2000) Mapping concentration profiles within the diffusion layer of an electrode Part II. Potentiometric measurements with an ultramicroelectrode. Electrochem Commun 2(4):248–253. https://doi.org/10.1016/S1388-2481(00)00016-3
Alizadeh A, Burns A, Lenigk R et al (2018) A wearable patch for continuous monitoring of sweat electrolytes during exertion. Lab Chip 18(17):2632–2641. https://doi.org/10.1039/C8LC00510A
Yu Y, Nassar J, Xu C et al (2020) Biofuel-powered soft electronic skin with multiplexed and wireless sensing for human-machine interfaces. Sci Robot 5(41):eaaz7946. https://doi.org/10.1126/scirobotics.aaz7946
Bariya M, Li L, Ghattamaneni R et al (2020) Glove-based sensors for multimodal monitoring of natural sweat. Sci Adv 6(35):eabb8308. https://doi.org/10.1126/sciadv.abb8308
Xu Y, Zhao G, Zhu L et al (2020) Pencil–paper on-skin electronics. Proc Natl Acad Sci 117(31):18292–18301. https://doi.org/10.1073/pnas.2008422117
Kim J, Jeerapan I, Imani S et al (2016) Noninvasive alcohol monitoring using a wearable tattoo-based iontophoretic-biosensing system. ACS Sens 1(8):1011–1019. https://doi.org/10.1021/acssensors.6b00356
Windmiller JR, Bandodkar AJ, Valdés-Ramírez G et al (2012) Electrochemical sensing based on printable temporary transfer tattoos. Chem Commun 48(54):6794–6796. https://doi.org/10.1039/c2cc32839a
Jia W, Bandodkar AJ, Valdés-Ramírez G et al (2013) Electrochemical tattoo biosensors for real-time noninvasive lactate monitoring in human perspiration. Anal Chem 85(14):6553–6560. https://doi.org/10.1021/ac401573r
Gao W, Nyein HYY, Shahpar Z et al (2016) Wearable microsensor array for multiplexed heavy metal monitoring of body fluids. ACS Sens 1(17):866–874. https://doi.org/10.1021/acssensors.6b00287
Lin S, Wang B, Yu W et al (2020) Design framework and sensing system for noninvasive wearable electroactive drug monitoring. ACS Sens 5(1):265–273. https://doi.org/10.1021/acssensors.9b02233
Wang J (2008) Electrochemical glucose biosensors. Chem Rev 108(2):814–825. https://doi.org/10.1021/cr068123a
Cheng X, Wang B, Zhao Y et al (2020) A mediator-free electroenzymatic sensing methodology to mitigate ionic and electroactive interferents’ effects for reliable wearable metabolite and nutrient monitoring. Adv Funct Mater 30(10):1908507. https://doi.org/10.1002/adfm.201908507
Martín A, Kim J, Kurniawan JF et al (2017) Epidermal microfluidic electrochemical detection system: enhanced sweat sampling and metabolite detection. ACS Sens 2(12):1860–1868. https://doi.org/10.1021/acssensors.7b00729
Teymourian H, Barfidokht A, Wang J (2020) Electrochemical glucose sensors in diabetes management: an updated review (2010–2020). Chem Soc Rev 49:7671–7709. https://doi.org/10.1039/D0CS00304B
Tai LC, Ahn CH, Nyein HYY et al (2020) Nicotine monitoring with a wearable sweat band. ACS Sens 5(6):1831–1837. https://doi.org/10.1021/acssensors.0c00791
Xu G, Cheng C, Liu Z et al (2019) Battery-free and wireless epidermal electrochemical system with all-printed stretchable electrode array for multiplexed in situ sweat analysis. Adv Mater Technol 4(7):1800658. https://doi.org/10.1002/admt.201800658
Bandodkar AJ, Hung VWS, Jia W et al (2013) Tattoo-based potentiometric ion-selective sensors for epidermal pH monitoring. Analyst 138(1):123–128. https://doi.org/10.1039/C2AN36422K
Zhao Y, Zhai Q, Dong D et al (2019) Highly stretchable and strain-insensitive fiber-based wearable electrochemical biosensor to monitor glucose in the sweat. Anal Chem 91(10):6569–6576. https://doi.org/10.1021/acs.analchem.9b00152
Kim S, Lee B, Reeder JT et al (2020) Soft, skin-interfaced microfluidic systems with integrated immunoassays, fluorometric sensors, and impedance measurement capabilities. Proc Natl Acad Sci 117(45):27906–27915. https://doi.org/10.1073/pnas.2012700117
Nyein HYY, Tai LC, Ngo QP et al (2018) A wearable microfluidic sensing patch for dynamic sweat secretion analysis. ACS Sens 3(5):944–952. https://doi.org/10.1021/acssensors.7b00961
Rose DP, Ratterman ME, Griffin DK et al (2015) Adhesive RFID sensor patch for monitoring of sweat electrolytes. IEEE Trans Biomed Eng 62(6):1457–1465. https://doi.org/10.1109/TBME.2014.2369991
Xiao G, He J, Chen X et al (2019) A wearable, cotton thread/paper-based microfluidic device coupled with smartphone for sweat glucose sensing. Cellulose 26(7):4553–4562. https://doi.org/10.1007/s10570-019-02396-y
Kwon K, Kim JU, Deng Y et al (2021) An on-skin platform for wireless monitoring of flow rate, cumulative loss and temperature of sweat in real time. Nat Electron 4(4):302–312. https://doi.org/10.1038/s41928-021-00556-2
Lin S, Yu W, Wang B et al (2020) Noninvasive wearable electroactive pharmaceutical monitoring for personalized therapeutics. Proc Natl Acad Sci 117(32):19017–19025. https://doi.org/10.1073/pnas.2009979117
Ghaffari R, Choi J, Raj MS et al (2020) Soft wearable systems for colorimetric and electrochemical analysis of biofluids. Adv Funct Mater 30(37):1907269. https://doi.org/10.1002/adfm.201907269
Kim SB, Zhang Y, Won SM et al (2018) Super-absorbent polymer valves and colorimetric chemistries for time-sequenced discrete sampling and chloride analysis of sweat via skin-mounted soft microfluidics. Small 14(12):1703334. https://doi.org/10.1002/smll.201703334
Promphet N, Rattanawaleedirojn P, Siralertmukul K et al (2019) Non-invasive textile based colorimetric sensor for the simultaneous detection of sweat pH and lactate. Talanta 192:424–430. https://doi.org/10.1016/j.talanta.2018.09.086
Vaquer A, Barón E, de la Rica R (2021) Wearable analytical platform with enzyme-modulated dynamic range for the simultaneous colorimetric detection of sweat volume and sweat biomarkers. ACS Sens 6(1):130–136. https://doi.org/10.1021/acssensors.0c01980
He J, Xiao G, Chen X et al (2019) A thermoresponsive microfluidic system integrating a shape memory polymer-modified textile and a paper-based colorimetric sensor for the detection of glucose in human sweat. RSC Adv 9(41):23957–23963. https://doi.org/10.1039/C9RA02831E
Koh A, Kang D, Xue Y et al (2016) A soft, wearable microfluidic device for the capture, storage, and colorimetric sensing of sweat. Sci Transl Med 8(366):366ra165. https://doi.org/10.1126/scitranslmed.aaf2593
Bandodkar AJ, Gutruf P, Choi J et al (2019) Battery-free, skin-interfaced microfluidic/electronic systems for simultaneous electrochemical, colorimetric, and volumetric analysis of sweat. Sci Adv 5(1):eaav3294. https://doi.org/10.1126/sciadv.aav3294
Choi J, Bandodkar AJ, Reeder JT et al (2019) Soft, skin-integrated multifunctional microfluidic systems for accurate colorimetric analysis of sweat biomarkers and temperature. ACS Sens 4(2):379–388. https://doi.org/10.1021/acssensors.8b01218
Sekine Y, Kim SB, Zhang Y et al (2018) A fluorometric skin-interfaced microfluidic device and smartphone imaging module for in situ quantitative analysis of sweat chemistry. Lab Chip 18(15):2178–2186. https://doi.org/10.1039/C8LC00530C
Morris NB, Cramer MN, Hodder SG et al (2013) A comparison between the technical absorbent and ventilated capsule methods for measuring local sweat rate. J Appl Physiol 114(6):816–823. https://doi.org/10.1152/japplphysiol.01088.2012
Parrilla M, Guinovart T, Ferré J et al (2019) A wearable paper-based sweat sensor for human perspiration monitoring. Adv Healthcare Mater 8(16):1900342. https://doi.org/10.1002/adhm.201900342
Reeder JT, Xue Y, Franklin D et al (2019) Resettable skin interfaced microfluidic sweat collection devices with chemesthetic hydration feedback. Nat Commun 10(1):1–12. https://doi.org/10.1038/s41467-019-13431-8
Nyein HYY, Bariya M, Tran B et al (2021) A wearable patch for continuous analysis of thermoregulatory sweat at rest. Nat Commun 12(1):1–13. https://doi.org/10.1038/s41467-021-22109-z
Choi DH, Gonzales M, Kitchen GB et al (2020) A capacitive sweat rate sensor for continuous and real-time monitoring of sweat loss. ACS Sens 5(12):3821–3826. https://doi.org/10.1021/acssensors.0c01219
Choi J, Xue Y, Xia W et al (2017) Soft, skin-mounted microfluidic systems for measuring secretory fluidic pressures generated at the surface of the skin by eccrine sweat glands. Lab Chip 17(15):2572–2580. https://doi.org/10.1039/C7LC00525C
He Q, Das SR, Garland NT et al (2017) Enabling inkjet printed graphene for ion selective electrodes with postprint thermal annealing. ACS Appl Mater Interf 9(14):12719–12727. https://doi.org/10.1021/acsami.7b00092
Zoerner A, Oertel S, Jank MPM et al (2018) Human sweat analysis using a portable device based on a screen-printed electrolyte sensor. Electroanalysis 30(4):665–671. https://doi.org/10.1002/elan.201700672
Abrar M, Dong Y, Lee P et al (2016) Bendable electro-chemical lactate sensor with printed silver nano ink. Sci Rep 6(1):1–9. https://doi.org/10.1038/srep30565
Dong Y, Min X, Kim WS (2018) A 3D printed integrated electro-chemical sensor system. IEEE Sens J 18(7):2959–2966. https://doi.org/10.1109/JSEN.2018.2801459
Nyein HYY, Bariya M, Kivimäki L et al (2019) Regional and correlative sweat analysis using high-throughput microfluidic sensing patches toward decoding sweat. Sci Adv 5(8):eaaw9906. https://doi.org/10.1126/sciadv.aaw9906
Xu J, Zhang Z, Gan S et al (2020) Highly stretchable fiber-based potentiometric ion sensors for multichannel real-time analysis of human sweat. ACS Sens 5(9):2834–2842. https://doi.org/10.1021/acssensors.0c00960
Su R, Wen J, Su Q et al (2020) 3D printed self-supporting elastomeric structures for multifunctional microfluidics. Sci Adv 6(41):eabc9846. https://doi.org/10.1126/sciadv.abc9846
Mehta V, Rath SN (2021) 3D printed microfluidic devices: a review focused on four fundamental manufacturing approaches and implications on the field of healthcare. Bio-Des Manuf 4:311–343. https://doi.org/10.1007/s42242-020-00112-5
Francis J, Stamper I, Heikenfeld J et al (2018) Digital nanoliter to milliliter flow rate sensor with in vivo demonstration for continuous sweat rate measurement. Lab Chip 19(1):178–185. https://doi.org/10.1039/C8LC00968F
Ouyang H, Jiang D, Fan Y et al (2021) Self-powered technology for next-generation biosensor. Sci Bull 66(17):1709–1712. https://doi.org/10.1016/j.scib.2021.04.035
Zou Y, Bo L, Li Z (2021) Recent progress in human body energy harvesting for smart bioelectronic system. Fundam Res 1(3):364–382. https://doi.org/10.1016/j.fmre.2021.05.002
Tan P, Zou Y, Fan Y et al (2020) Self-powered wearable electronics. Wearable Technol 1:e5. https://doi.org/10.1017/wtc.2020.3
Gu X, Zhou Y, Gu K et al (2017) Roll-to-roll printed large-area all-polymer solar cells with 5% efficiency based on a low crystallinity conjugated polymer blend. Adv Energy Mater 7(14):1602742. https://doi.org/10.1002/aenm.201602742
Zhao J, Lin Y, Wu J et al (2019) A fully integrated and self-powered smartwatch for continuous sweat glucose monitoring. ACS Sens 4(7):1925–1933. https://doi.org/10.1021/acssensors.9b00891
Luo J, Gao W, Wang ZL (2021) The triboelectric nanogenerator as an innovative technology toward intelligent sports. Adv Mater 33(17):2004178. https://doi.org/10.1002/adma.202004178
Song Y, Min J, Yu Y et al (2020) Wireless battery-free wearable sweat sensor powered by human motion. Sci Adv 6(40):eaay9842. https://doi.org/10.1126/sciadv.aay9842
Yin L, Moon JM, Sempionatto JR et al (2021) A passive perspiration biofuel cell: high energy return on investment. Joule 5(7):1888–1904. https://doi.org/10.1016/j.joule.2021.06.004
Yeknami AF, Wang X, Jeerapan I et al (2018) A 0.3-V CMOS biofuel-cell-powered wireless glucose/lactate biosensing system. IEEE J Solid-State Circ 53(11):3126–3139. https://doi.org/10.1109/JSSC.2018.2869569
Yin L, Kim KN, Lv J et al (2021) A self-sustainable wearable multi-modular E-textile bioenergy microgrid system. Nat Commun 12(1):1–12. https://doi.org/10.1038/s41467-021-21701-7
Jing Y, Wang A, Li J et al (2021) Preparation of conductive and transparent dipeptide hydrogels for wearable biosensor. Bio-Des Manuf. https://doi.org/10.1007/s42242-021-00143-6
Chen H, Zhang Y, Zhang L et al (2021) Applications of bioinspired approaches and challenges in medical devices. Bio-Des Manuf 4:146–148. https://doi.org/10.1007/s42242-020-00103-6
Heikenfeld J, Jajack A, Feldman B et al (2019) Accessing analytes in biofluids for peripheral biochemical monitoring. Nat Biotechnol 37(4):407–419. https://doi.org/10.1038/s41587-019-0040-3
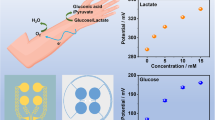
Huang X, Li J, Liu Y et al (2021) Epidermal self-powered sweat sensors for glucose and lactate monitoring. Bio-Des Manuf. https://doi.org/10.1007/s42242-021-00156-1
Bandodkar AJ, Jeang WJ, Ghaffari R et al (2019) Wearable sensors for biochemical sweat analysis. Annu Rev Anal Chem 12:1–22. https://doi.org/10.1146/annurev-anchem-061318-114910
Dunn MR, Jimenez RM, Chaput JC (2017) Analysis of aptamer discovery and technology. Nat Rev Chem 1(10):0076. https://doi.org/10.1038/s41570-017-0076
Parrilla M, Ferré J, Guinovart T et al (2016) Wearable potentiometric sensors based on commercial carbon fibres for monitoring sodium in sweat. Electroanalysis 28(6):1267–1275. https://doi.org/10.1002/elan.201600070
Acknowledgements
This work was supported in part by the National Natural Science Foundation of China (Nos. 51975513 and 52105593), the Natural Science Foundation of Zhejiang Province, China (No. LR20E050003), and the Major Research Plan of Ningbo Innovation 2025 (No. 2020Z022).
Author information
Authors and Affiliations
Contributions
WZH was involved in writing the original draft; GY, WSK, and KCX had contributed to writing, reviewing, and editing.
Corresponding authors
Ethics declarations
Conflict of interest
The authors declare that there is no conflict of interest.
Ethical approval
This article does not contain any studies with human or animal subjects performed by any of the authors.
Rights and permissions
About this article
Cite this article
Heng, W., Yang, G., Kim, W.S. et al. Emerging wearable flexible sensors for sweat analysis. Bio-des. Manuf. 5, 64–84 (2022). https://doi.org/10.1007/s42242-021-00171-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s42242-021-00171-2