Key summary points
The systematic review aimed to assess the under-triage rate for older trauma patients in prehospital care and its impact on their outcomes.
AbstractSection FindingsOlder trauma patients were significantly under-triaged in prehospital care and the benefits of triaging these patients to Tauma Centres (TCs) are still uncertain. Current triage criteria and developed geriatric-specific criteria lacked acceptable accuracy and when patients met the criteria, they had a low chance of being transported to TCs.
AbstractSection MessageFuture worldwide research is needed to assess the following aspects: (1) the accuracy of current trauma triage criteria, (2) developing more accurate triage criteria, (3) destination compliance rates for patients meeting the triage criteria, (4) factors leading to destination non-compliance and their impact on outcomes, and (5) the benefits of TC access for older trauma patients.
Abstract
Background
It is argued that many older trauma patients are under-triaged in prehospital care which may adversely affect their outcomes. This systematic review aimed to assess prehospital under-triage rates for older trauma patients, the accuracy of the triage criteria, and the impact of prehospital triage decisions on outcomes.
Methods
A computerised literature search using MEDLINE, Scopus, and CINHAL databases was conducted for studies published between 1966 and 2021 using a list of predetermined index terms and their associated alternatives. Studies which met the inclusion criteria were included and critiqued using the Critical Appraisal Skills Programme tool. Due to the heterogeneity of the included studies, narrative synthesis was used in this systematic review.
Results
Of the 280 identified studies, 23 met the inclusion criteria. Current trauma triage guidelines have poor sensitivity to identify major trauma and the need for TC care for older adults. Although modified triage tools for this population have improved sensitivity, they showed significantly decreased specificity or were not applied to all older people. The issue of low rates of TC transport for positively triaged older patients is not well understood. Furthermore, the benefits of TC treatment for older patients remain uncertain.
Conclusions
This systematic review showed that under-triage is an ongoing issue for older trauma patients in prehospital care and its impact on their outcomes is still uncertain. Further high-quality prospective research is needed to assess the accuracy of prehospital triage criteria, the factors other than the triage criteria that affect transport decisions, and the impact of under-triage on outcomes.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The population of older adults is continuing to grow in numerous countries across the world. In the United Kingdom (UK), 18% of the population are now aged ≥ 65 years [1] and the number of people aged ≥ 85 years is predicted to double in the next 25 years [2]. The trend of increasing rates of population ageing is generalised to most European countries [3]. There were 90.5 million people aged ≥ 65 years living in Europe in 2019 which represented 20.3% of the total population [3]. This trend is expected to continue in Europe; peaking at 129.8 million older adults and representing 29.4% of the total population by 2050 [3]. As this population grows, more older patients will require high-quality trauma care including prehospital assessment, management, and triage decisions [4].
Current data indicates there is an increasing number of patients aged ≥ 60 years who have sustained major injuries despite apparently low impact trauma, and these now comprise half the number of patients classified as having major trauma in the UK (Injury Severity Score [ISS] > 15) [5]. Although recent studies have shown that older trauma patients with one or more comorbid health problems are at greater risk of death [6], clinical protocols and guidelines are not clear on how to optimise the treatment and management of this population [4].
Prehospital trauma triage tools are predominantly used to identify injury severity in trauma patients to determine transportation decisions [7, 8]. Any trauma triage tool should be sensitive enough to identify major trauma patients so they can benefit from access to level I/II Trauma Centres (TCs) (equivalent to Major Trauma Centres in the UK, or Major Trauma Service in Australia), whilst being specific enough to predict patients whose injuries are not classified as major trauma so they can be treated at lower or non-TCs [9]. Recent research has found that older people suffer increased under-triage in prehospital trauma care [10].
Under-triage refers to the transportation of severely injured patients to lower-level TCs or other acute care facilitates [11]. There are several factors that may affect the accuracy of prehospital trauma triage criteria and triage decisions for older adults, including altered physiological responses to trauma [12, 13], perceived insignificant injury mechanisms such as low-level falls (i.e. < 2 m) [14, 15], high comorbidity [16] and frailty rates [17, 18], and the use of multiple medications [19]. The effective triage of injured patients is the first step towards providing high-quality care and reducing mortality rates [20]. A recent piece of evidence from Sweden showed that treatment at TCs was associated with a 41% lower adjusted 30-day mortality (Odds Ratio [OR] 0.59, 95% Confidence Interval [CI] 0.50–0.70, P < 0.0001) compared to non-TCs for all trauma patients (i.e., ISS ≥ 1) [21]. Evidence from the United States of America (USA) also showed that TC treatment, compared to non-TC treatment, was associated with a significantly lower in-hospital mortality rate (7.6% vs. 9.5%, Relative Risk [RR] 0.80, 95% CI 0.66–0.98) and one-year mortality rate (10.4% vs. 13.8%, RR 0.75, 95% CI 0.60–0.95) [22]. Therefore, increased under-triage for older trauma patients is considered to increase their mortality rates [10]. This systematic review, therefore, aimed to assess recent evidence for prehospital under-triage rates of older trauma patients, the accuracy of current and developed prehospital trauma triage criteria for this population, and the impact of prehospital trauma triage on their outcomes.
Methods
To effectively answer the problem of the review, an appropriate question was established using the Population, Intervention, Comparison, and Outcome (PICO) model [23]: are older trauma patients under-triaged in prehospital care? (P: older adults, I: trauma triage, C: younger adults, and O: rate of under-triage).
A literature search was undertaken using the following databases: MEDLINE, Scopus, and CINHAL. A list of index terms and associated alternatives were generated prior to performing this electronic search to identify the most relevant literature. The index terms were: ‘older adult*’, ‘trauma’, ‘under-triage’, and ‘prehospital’. The alternatives that were applied in this search included the following: ‘advanced age’, ‘elderly’, ‘geriatric*’, ‘injur*’, ‘triag*’, ‘paramedic*’, ‘emergency medical service*’, ‘EMS’, and ‘ambulance’. In addition to searching the selected databases, the reference lists of the included studies were reviewed to identify further possible studies for inclusion in this review. This systematic review was performed according to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines [24].
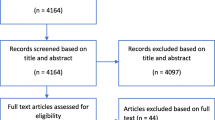
Clear inclusion/exclusion criteria were discussed and determined by the authors prior to search the literature (Fig. 1). No specific time limits were employed in this search as any study met the criteria and published prior to January 7, 2021, which is the date of the last database search, was included in the review.
The eligibility assessment, data extraction, and critical appraisal were performed independently by two reviewers (first and second authors). The process of critical appraisal was performed using the Critical Appraisal Skills Programme (CASP) for quantitative cohort studies [25]. The rates of under-triage among older trauma patients and their impact on the outcomes were the primary outcome measures. Under-triage, in general, is defined as transporting patients with major trauma (ISS > 15) whether they met the prehospital trauma triage or not to lower-level or non-TCs. We made sure to define under-triage in the included studies as it is sometimes defined by triage criteria, initial destination, or final destination. The sensitivity and specificity of any triage criteria could differ from one to another based on what they are sensitive or specific for, which may include, for example, higher injury severity, need for TC care, or adverse outcomes. This was considered and made clear in the results section where needed. Each study was read, reread, critically appraised, and assessed for the risk of bias including the assessment of selective reporting bias independently by two reviewers. The main findings of each study were collated, assessed for further analysis, and are interpreted in the discussion. A third reviewer was assigned in case of disagreement about inclusion/exclusion criteria or quality assessment of the included studies in the systematic review. Due to the heterogeneity of the included studies, a thematic interpretation was applied [26]. Sub-themes were generated from each included study first which then were merged into more representative themes.
Results
Of the 280 screened articles, 33 abstracts were found relevant to the initial inclusion in this review (Fig. 2). After obtaining and reviewing full-text articles, 10 studies were excluded as they were not original research (literature review, articles, and editorial) [27,28,29,30], not focused in evaluating prehospital triage [10, 31,32,33], assessed a specific injury mechanism [34], or used the same data of another included study [35]. The quality assessment of the remaining 23 articles was performed independently by two reviewers. There were no disagreements between the two reviewers.
Six of the 23 included studies did not mention any information about ethical approval [36,37,38,39,40,41]. Two studies may have a risk of selection bias; one study included all patients coming to the emergency department whether by ambulance or private vehicle which could adversely affect the assessment of the accuracy of prehospital triage decisions [42], and one study restricted its sample to those who had pre-injury information [43]. Overall, all the included articles were of moderate quality.
Most of the included studies were conducted in the USA (n = 21) [36, 38,39,40,41,42,43,44,45,46,47,48,49,50,51,52,53,54,55,56,57]. Eleven studies were published in the last five years [41, 43,44,45, 47, 50, 52, 55,56,57,58], four of which were published in 2020 [41, 55,56,57]. All studies were retrospective cohort studies and only one study additionally included a survey (Table 1). Furthermore, data were collected retrospectively for different periods of time ranging from six months to up to 13 years (Table 1). The included studies had different definitions of the population of older adults by age (Table 1). Moreover, some studies included younger adults and children, comparing their prehospital trauma triage decisions with those of older adults (Table 1).
A thematic approach was applied when analysing the literature as this was appropriate given the methods employed in the articles that were reviewed [26]. Upon completion of full-text reading and critical analysis, seventeen initial sub-themes were identified and developed based on their prominence and relevance to the review. Interlinked subthemes were then combined into five overarching and representative themes (Table 2). The themes within each included study are presented in Supplement 1.
Under-triage rates
In the USA, nationwide research has found that older trauma patients are significantly under-triaged in prehospital care [42] (Table 3). This finding is similar to the results of other studies conducted at both regional and state-wide level in the USA [38,39,40, 43, 46,47,48, 50,51,52,53, 55,56,57], and Australia [37, 58] (Table 3). Under-triage is still an ongoing issue for older trauma patients for over 25 years now, however, most research work looking into this issue was done in the last decade (Table 3).
Under-triage rates were shown to be relatively constant in trauma patients up to 60 years, then increased with age up to a rate of 58% to 62% in patients aged > 90 years [51]. Further evidence from the USA and Australia showed increased under-triage with increasing age among older trauma patients [40, 58] (Table 3).
Evidence from Australia also showed that, even though current adult prehospital trauma triage criteria are more sensitive in identifying major trauma (ISS > 15) for older adults than those described in other research studies [38,39,40, 42, 43, 46,47,48,49,50,51,52,53, 55,56,57], older trauma patients were significantly under-triaged in comparison with younger adults [37]. Even during inter-hospital transfers, older trauma patients were less likely to be transferred to higher TCs. For example, 53% of older patients presenting at non-TCs were transferred to other non-TCs compared to only 34% of younger patients [47]. In addition, 15% were transported by Helicopter Emergency Medical Services (HEMS) compared to 20% of younger trauma patients [47]. Indeed, Meyers et al. [50] showed that almost 3% of the entire study population of older trauma patients were transported through HEMS although 31% of them met the trauma triage criterion (≥ 60 min from the nearest TC).
Some older trauma patients were not triaged in prehospital care, which may explain the issue of increased under-triage rates in this population. The transport of patients aged ≥ 65 years by private vehicles, meaning they were not triaged in prehospital care, was associated with increased odds of non-TC treatment by 19% compared to those transported by ambulance (OR 1.19; 95% CI 1.17–1.20) [57]. Furthermore, for patients with an ISS > 15 and living > 30 miles from TCs, the private vehicle transport was associated with increased odds of under-triage by 69% (OR 1.69; 95% CI 1.62–1.76) compared to those transported by ambulance [57]. Treatment at TCs was predominantly associated with ambulance transport for older trauma patients [55].
Clinical effectiveness of trauma triage criteria
Current trauma triage tools lack acceptable accuracy in identifying major trauma for older adults [48, 52]. Most common examples of prehospital triage tools are Field Triage Decision Scheme in the USA [59] and the Major Trauma Triage Tool in the UK [60]. Different triage tools are applied in different countries even some states, cities, or trusts within the same country have different trauma triage tools, which makes it difficult to cover all of them in this review.
A study from the USA showed that the sensitivity of current trauma triage criteria to identify major trauma (ISS > 15) and need for TC care was 61% for patients aged ≥ 70 years compared to 87% for younger patients [48]. Another study highlighted a sensitivity of almost 76% in identifying major trauma for patients aged ≥ 65 years [52]. However, research in Australia has shown that the Victorian trauma triage tool can identify major trauma among older patients as effectively as it can for younger patients with sensitivity rates of 96% [37].
There are factors that could adversely affect meeting some criteria of the triage tool for older trauma patients such as physiological criteria [47, 49, 54, 55], comorbidities [55], injury pattern and mechanism [39, 41, 53, 58] (Table 4). Distance could also affect the time to get the patient to a TC, which is used as a criterion for TC transport in some triage tools [47, 55, 57] (Table 4).
Developing specific trauma triage criteria
Some scholars have argued that all trauma systems and centres should have specific and effective guidelines for triaging and managing older trauma patients [49]. This has led to further research focusing on the development of specific trauma triage guidelines for older people. Some studies modified the current trauma triage guidelines while others developed separate and specific triage criteria for older trauma patients.
Applying age (age boundary of > 55 years) as a mandatory triage criterion in the trauma triage tool was shown to significantly increase the rates of over-triage as one additional patient with severe injury (ISS > 15) was identified for every 60–65 patients with less severe injuries to be transported to TCs [51]. However, applying the Systolic Blood Pressure (SBP) < 110 mm Hg instead of the SBP < 90 mm Hg for triaging older trauma patients in prehospital care decreased the under-triage rate by 4% and increased the over-triage rate by 4% [36]. As the risk of death for older trauma patients who had a SBP < 110 mm Hg is similar to those who had a SBP < 90 mm Hg, this finding may require the application of this criterion for the direct transportation of these patients to TCs [36]. Furthermore, for trauma patients aged ≥ 70 years, applying the criterion of Glasgow Coma Scale (GCS) ≤ 14 instead GCS ≤ 13 increased the sensitivity rate of the triage tool in this population from 50.7 (95% CI 47.5–53.9) to 59.2% (95% CI 56.1–62.3) with a similar specificity rate to the criterion GCS ≤ 13 in younger adults (85.1% [95% CI 84.6–85.7] vs. 85% [95% CI 84.6–85.4], respectively) [54].
Some other studies developed separate and specific trauma triage criteria for older adults. For example, Newgard et al. [52] developed an alternative trauma triage tool for trauma patients aged ≥ 65 years that, compared to current adult trauma triage guidelines, showed better sensitivity in identifying major trauma (ISS > 15) (92% vs. 76%) but significantly less specificity (42% vs. 78%). Furthermore, Newgard and colleagues [43] developed a clinical decision rule for triaging older trauma patients which aligned the current triage criteria with geriatric-specific physiology and comorbidity criteria. The overall sensitivity of this decision rule was 90%, however, it had significantly low specificity (17%) to identify injured older adults who had an ISS > 15 or those who require major non-orthopaedic surgery. Adding the use of anticoagulants in the decision rule was not shown to be a good predictor of high-risk patients when compared to current triage criteria, geriatric-specific physiologic measures, and comorbidities [43]. However, the geriatric-specific trauma triage guidelines developed by the Trauma Committee of the Ohio Emergency Medical Services Board showed increased sensitivity for patients aged ≥ 70 years compared to current adult trauma triage criteria (93% vs. 61%) and decreased specificity (49% vs. 61%) [48]. Furthermore, the performance of this developed triage tool in geriatric trauma patients was similar to the performance of the current triage tool in younger trauma patients (sensitivity: 93% vs. 87%, and specificity: 49% vs. 44%, respectively) [48]. Nevertheless, using the cut-off point of ≥ 70 years represents a major limitation in this triage tool as a previous study has shown that under-triage issues can begin as early as the age of 50 years [46].
Trauma triage destination compliance
‘Destination compliance’ is defined as access to the highest level of trauma services for patients who meet the prehospital trauma triage criteria. An example of this is that if a trauma patient with a GCS 8 was assessed by a paramedic to have severe injury and met the triage criteria for TC transport, he/she was actually transported to a TC. In this section, we are going to discuss the rates of destination compliance and the possible contributing factors leading to destination non-compliance for older trauma patients meeting the prehospital triage criteria.
Destination compliance and current triage criteria
For injured patients meeting current triage criteria, there was a constant decrease in the rate of destination compliance with increasing age [37, 50, 51]. Trauma patients aged > 60 years had a greater under-triage rate when defined by hospital destination; indicating that older trauma patients meeting the triage criteria were not as likely to be transported to TCs [51]. In Australia, 67% of older confirmed major trauma patients who met the triage criteria were transported to a TC in comparison with 88% of younger patients [37]. In the USA, older trauma patients, when they met the triage criteria, were only half as likely as younger adults to be transported to designated TCs [46]. More recent evidence from the USA also showed that of all older trauma patients meeting the triage criteria, only 38% were transported to level I/II TCs [43]. Significantly high rates of under-triage was identified in older trauma patients whose closest facility was non-TC whether it had less than 200 beds or had 200 or more beds (adjusted OR 4.48, P < 0.001; adjusted OR 8.53, P < 0.001, respectively) [56].
For older trauma patients meeting the physiological criteria of the prehospital triage tool, another piece of more recent evidence showed that only 24% of hypotensive patients (SBP < 90 mmHg), 22.6% of those who had an abnormal respiratory rate (< 10 or > 29 breaths per minute), and 26% of those who had a GCS < 13 were transported to a TC [50]. With respect to distance, even when older patients were injured in places close to a TC, they were less likely to be transported to these centres than younger adults [47]. Indeed, 55.8% of older trauma patients living in urban regions were transported to lower or non-TCs [42].
Destination compliance and developed geriatric-specific triage criteria
Caterino et al. [45] found that developing geriatric-specific triage criteria significantly improved the identification of trauma, however, the rate of initial transportation only increased by 1% while the rate of initial transportation and inter-hospital transfers increased by 2%; indicating an issue of destination non-compliance for patients meeting the triage criteria. In the USA, only 47% of older patients who met the geriatric-specific trauma triage criteria were initially transported to level I/II TCs and 59% were ultimately transported to these centres [44]. Of those, patients who lived in regions with level I/II TCs had the highest rates of being transported to these centres whereas patients in regions with level III TCs had the lowest rates of higher-level TC transport [44]. This means that patients in regions with no TCs had a better chance for level I or II TC transport either initially or ultimately than those in regions with level III TCs [44].
Factors leading to destination non-compliance
It is still unclear which factors have led to under-triage among older trauma patients; reduced sensitivity of the triage guidelines or factors such as ageism, patient choice, or other inherent variations relevant to indications of severe trauma in this population [51]. It is also argued that decision-making during the triage of older trauma patients could be affected by paramedics’ subjective judgments [37].
One of the possible factors leading to destination noncompliance for older trauma patients is patient or relative choice as evidence showed that most hospital selections were driven by the choice of the patient or relative [52] (Table 4). However, there were inconsistent findings regarding the benefits this may confer in terms of improving care for older patients [52]. Furthermore, the assessment of socioeconomic factors showed a possibility of bias with respect to ethnicity, age, and sex (towards female sex) which needs more rigorous assessment and investigation [41, 55,56,57] (Table 4). Additionally, surveys of paramedics showed other paramedic-related factors which could impact appropriate triage decisions for older trauma patients including insufficient training, unfamiliarity with protocols, possible ageism, and feeling unwelcomed when bringing patients to a TC [46] (Table 4).
Trauma triage and outcomes
Older patients had significantly higher mortality than younger adults following injury [37, 47]. The odds of death for trauma patients increased by 8% for each year at the age cut-off > 55 years (OR 1.08; 95% CI 1.07–1.09) [37]. This is consistent with other research findings which found increasing mortality rates with age [39, 40]; highlighting the need for a better understanding of trauma outcomes for older patients. Larger proportion of older patients died at non-TCs (32%) than TCs (20%) [37]. The lower odds of transporting older trauma patients to TCs was associated with 1.7 times increased likelihood of their in-hospital deaths (95% CI 1.04–2.7) [58]. Under-triaged older trauma patients, compared to younger adults, had higher rates of mortality (21% vs. 6%), disability (22% vs. 6%), and complications (39% vs. 23%) [49].
Benefits of trauma centre access
A recent study by Garwe et al. [55] found contradicting evidence as the TC treatment for patients aged ≥ 55 years was associated with longer in-hospital stay (mean [SD], 7.6 (7.2) vs 5.8 (5.6), p < 0.0001) and had higher un-adjusted mortality (10.2% vs. 7.5%, p < 0.0001) than those treated at non-TCs [55]. In the multivariate Cox regression analyses, treatment at TCs was significantly associated with a lower likelihood of death within the first 7-days after adjusting for potential confounding factors and this effect was much stronger for patients aged 55 to 64 years (Hazard Ratio [HR] 0.45, 95% CI 0.36–0.56) compared to those aged ≥ 65 years (HR 0.65, 95% CI 0.58–0.73) [55]. The protective effect for treating patients at TCs was also observed in those who survived beyond 7 days (HR 0.69, 95% CI 0.56–0.83) [55]. Furthermore, after adjusting for potential confounders, transfer to TCs was associated with significantly lower 30-day mortality for patients aged 55 to 64 years (HR 0.36, 95% CI 0.27–0.49) and also for those aged ≥ 65 years (HR 0.55, 95% CI 0.48–0.64) [55]. Another piece of evidence also showed that the treatment of trauma patients aged ≥ 65 years at TCs was associated with a significant positive change in the probability of survival (marginal effect of 3.9% at the 5% level) although, when patients were stratified by age, patients aged ≥ 85 years had no statistical significance of the effect of TC treatment on their probability of survival at the 5% level (marginal effect of 3.6%) compared to patients aged 65 to 74 years (marginal effect of 7%) and patients aged 75 to 84 years (marginal effect of 4%) [40]. Conversely, Staudenmayer et al. [53] showed that the unadjusted 60-day mortality rate for older trauma patients transported to non-TC with an ISS > 15 was not significantly different from those with the same score who were transported to TCs (16% vs. 17%, p = 0.87). The transportation of older patients with major trauma (ISS > 15) to TCs was associated with higher costs than non-TCs (Total costs, $, median [IQR], 35,069 [19,321—88,357] vs. 14,332 [5112—29,321]) and longer in-hospital stays (Length of stay, days, median [IQR], 6.0 [3.0—14.0] vs. 5.0 [1.5—8.0]) [53]. However, the study did not adjust for important confounders such as comorbidities, specific patterns of injury such as head injury, and the mortality analysis was based on only 41 deaths which may have impacted the precision of the estimated effect [53].
Outcomes and the development of geriatric-specific trauma triage criteria
The application of a geriatric-specific trauma triage tool was shown to have no significant difference in mortality rates after its application compared to pre-application (7%), which may be attributed to destination non-compliance for patients meeting the developed triage criteria [45]. Patients with ISS < 10 were the only group who benefit from applying the developed triage tool (decreased mortality from 3.0 to 2.5%) [45]. Evidence showed that a large proportion of older trauma patients died after sustaining minor to mild injuries [53]. In contrast, ISS > 15 was shown to be the highest level of serious injury that predicts increased in-hospital mortality rates for injured patients aged ≥ 65 [52]. Applying the geriatric-specific trauma triage tool resulted in a minimal unadjusted increase from 34% (95% CI 33–35%) to 35% (95% CI 35–35%) in the number of older patients discharged home (difference 1.2%, 95% CI of the difference 0.2–2.2%) (p = 0.02) [45].
For trauma patients aged ≥ 70 years, a decline in the GCS from 15 to 14 was associated with increased mortality (OR 1.40; 95% CI 1.07–1.83), which was not the case for younger adults (OR 1.22; 95% CI 0.88–1.71). Similarly, a decline in the GCS from 14 to 13 was also associated with increased mortality for older patients (OR 2.34; 95% CI 1.57–3.52) but not for younger adults (OR 1.45; 95% CI 0.91–2.30) [54]. Moreover, patients aged ≥ 70 years with a GCS of 14 were shown to have higher odds of mortality (OR 4.68; 95% CI 2.90–7.54) and traumatic brain injuries (OR 1.84; 95% CI 1.45–2.34) than younger adults with GCS 13; suggesting the need for modifying the GCS criterion for older trauma patients so they can possibly get the advantage of direct transport to TCs [54].
Discussion
This review showed that the findings from relevant literature showed significant rates of under-triage for older trauma patients in prehospital care. There was no substantial qualitative difference in the older versus more recent studies. Most of the current and developed trauma triage guidelines lack acceptable accuracy to identify major trauma or were not applied to all older adults. Lower rates of destination compliance represent a major issue for this population to access TCs. The review showed that the association between under-triage of seriously injured older patients and high mortality rates is inconclusive. There was a conflict of evidence about the benefits of TC access for older trauma patients with regards to their survival or mortality rates. Some papers found that under-triage is associated with high rates of mortality, disability, and complications for older trauma patients. Treatment at TCs was associated with significantly higher costs and a lengthier in-hospital stay than at non-TCs.
Older trauma patients usually have injuries compounded with multimorbidity and frailty. This could adversely affect the accuracy of prehospital trauma triage tools even when geriatric-specific triage criteria were developed to adjust for age-related anatomical and physiological changes, comorbidities, and medication use [61], as shown in this review. Therefore, integrating other assessment tools, such as frailty, into the trauma triage tool may improve the identification of high-risk patients and reduce under-triage [62]. However, paramedics’ compliance to trauma triage tools was shown to decrease with patients aged ≥ 55 years compared to younger adults [63], which is consistent with our findings. The compliance rate of paramedics to trauma triage tools ranged from 21 to 93% [63]; affecting the usefulness of applying frailty-attuned scores in prehospital care.
Understanding research priorities in geriatric trauma is complex including prehospital care [64]. Quick and accurate prehospital triage and transportation decisions for older trauma patients are needed and this review has shown that the majority of the recent efforts in the literature are looking into this area intensively. However, a recent consensus-building exercise determined that assessing the benefits of TC access for older trauma patients to be more important [65]. Our review showed that some literature found some survival benefit of triaging and transporting older trauma patients to TCs, but these findings are still uncertain. The treatment at TCs was, however, shown to increase the length of in-hospital stay and costs. These findings were consistent with other research findings which showed an inconclusive survival benefit of TC access for this population [62].
Most studies looking into outcomes in this review assessed the impact of prehospital triage decisions mainly on mortality or survival rates. No standardised Patient-Reported Outcome Measures (PROMs) were used to assess patient outcomes. A recent review highlighted the importance of assessing outcomes beyond mortality for older trauma patients [62]. It also argued that assessing both clinical and patient outcomes are important for this population to strike an ethical balance between paternalism (in healthcare provision) and autonomy (of the patient in what they expect and seek) when caring for this population [62]. Therefore, it is important to determine appropriate Clinician-Reported Outcome Measures (CROMs) and PROMs to appropriately assess the impact of prehospital trauma triage decisions and the benefits TC care for this population.
This systematic review is the first review to assess prehospital triage specifically for older trauma patients using a thematic approach. The review followed a systematic approach in searching the literature, quality assessment, and presenting the findings which was performed independently by two reviewers. However, there were some limitations evident in this review that should be highlighted. The review was restricted to papers published in English which could preclude the results from non-English papers that may have impacted the findings. Furthermore, due to the heterogeneity of the included studies, we were unable to perform a meta-analysis and a sub-group comparison between older and more recent studies.
The review has several significant implications. Because all the studies followed a retrospective design, this precludes the measurement of key factors that may have had a bearing on the findings. More studies utilising a high-quality prospective design are needed to further assess the effectiveness of current trauma triage tools and destination compliance for older patients. Furthermore, there is a need to develop more accurate geriatric-specific triage criteria and assess the integration of frailty assessment into the triage tool. The impact of triaging older trauma patients to TCs should be assessed more on both clinical and patient outcomes. Moreover, studies focusing on different healthcare systems in other countries are required to further enhance the application of effective prehospital trauma triage for older patients.
Conclusion
Prehospital under-triage of older trauma patients seems to be an ongoing issue that requires future high-quality prospective research to assess and improve the accuracy of prehospital triage criteria for this population. Decreased compliance with prehospital triage decisions for positively triaged patients with age was identified in this review and the factors leading to this issue needs further investigation and assessment. The impact of this issue on the outcomes is still uncertain. There are no standardised outcome measures for older trauma patients that can be reliably measured to assess the impact of prehospital triage decisions.
Abbreviations
- RR:
-
Relative Risk.
- TTDP:
-
Trauma Triage Destination Plans
- AUC:
-
Area Under the Curve
- PROMs:
-
Patient-Reported Outcome Measures
- CROMs:
-
Clinician-Reported Outcome Measures
- AIS:
-
Abbreviated Injury Scale
- CASP:
-
Critical Appraisal Skills Programme
- UK:
-
United Kingdom
- USA:
-
United States of Americ
- ISS:
-
Injury Severity Score
- TC:
-
Trauma Centre
- OR:
-
Odds Ratio
- CI:
-
Confidence Interval
- PICO:
-
Population, Intervention, Comparison, and Outcome
- PRISMA:
-
Preferred Reporting Items for Systematic Reviews and Meta-Analyses
- NISS:
-
New Injury Severity Score
- HEMS:
-
Helicopter Emergency Medical Services
- FTTA:
-
Florida Trauma Triage Algorithm
- IQR:
-
Interquartile Range
- SBP:
-
Systolic Blood Pressure
- HR:
-
Heart Rate
- GCS:
-
Glasgow Coma Scale
- SD:
-
Standard Deviation
- HR:
-
Hazard Ratio
References
Office for National Statistics. https://www.ons.gov.uk/peoplepopulationandcommunity/populationandmigration/populationestimates/bulletins/annualmidyearpopulationestimates/mid2016. Accessed 2019 May 15
Office for National Statistics. https://www.ons.gov.uk/peoplepopulationandcommunity/populationandmigration/populationprojections/bulletins/nationalpopulationprojections/2016basedstatisticalbulletin. Accessed 2019 May 15
European Commission: The ageing Europe - Looking at the lives of older people in the EU: The Publications Office of the European Union, 2020
Mitra B, Cameron PA (2012) Optimising management of the elderly trauma patient. Injury 43(7):973–975
Trauma Audit and Research Network (TARN): Major trauma in older people. In: Salford/United Kingdom.
Keller JM, Sciadini MF, Sinclair E, O’Toole RV (2012) Geriatric trauma: demographics, injuries, and mortality. J Orthop Trauma 26(9):e161–e165
Newgard CD, Rudser K, Hedges JR, Kerby JD, Stiell IG, Davis DP, Morrison LJ, Bulger E, Terndrup T, Minei JP et al (2010) A critical assessment of the out-of-hospital trauma triage guidelines for physiologic abnormality. J Trauma 68(2):452–462
Sasser SM, Hunt RC, Faul M, Sugerman D, Pearson WS, Dulski T, Wald MM, Jurkovich GJ, Newgard CD, Lerner EB et al (2012) Guidelines for field triage of injured patients: recommendations of the National Expert Panel on Field Triage, 2011. MMWR Recomm Rep 61(1):1–20
Rehn M, Eken T, Krüger AJ, Steen PA, Skaga NO, Lossius HM (2009) Precision of field triage in patients brought to a trauma centre after introducing trauma team activation guidelines. Scand J Trauma Resusc Emerg Med 17(1):1
Rogers A, Rogers F, Bradburn E, Krasne M, Lee J, Wu D, Edavettal M, Horst M (2012) Old and undertriaged: a lethal combination. Am Surg 78(6):711–715
Rotondo M, Cribari C, Smith R (2014) American College of Surgeons Committee on Trauma: Resources for optimal care of the injured patient, vol 6. American College of Surgeons, Chicago
Heffernan DS, Thakkar RK, Monaghan SF, Ravindran R, Adams CA Jr, Kozloff MS, Gregg SC, Connolly MD, Machan JT, Cioffi WG (2010) Normal presenting vital signs are unreliable in geriatric blunt trauma victims. J Trauma 69(4):813–820
Martin JT, Alkhoury F, O’Connor JA, Kyriakides TC, Bonadies JA (2010) ‘Normal’vital signs belie occult hypoperfusion in geriatric trauma patients. Am Surg 76(1):65–69
Sampalis JS, Nathanson R, Vaillancourt J, Nikolis A, Liberman M, Angelopoulos J, Krassakopoulos N, Longo N, Psaradellis E (2009) Assessment of mortality in older trauma patients sustaining injuries from falls or motor vehicle collisions treated in regional level I trauma centers. Ann Surg 249(3):488–495
Spaniolas K, Cheng JD, Gestring ML, Sangosanya A, Stassen NA, Bankey PE (2010) Ground level falls are associated with significant mortality in elderly patients. J Trauma 69(4):821–825
Negin J, Martiniuk A, Cumming RG, Naidoo N, Phaswana-Mafuya N, Madurai L, Williams S, Kowal P (2012) Prevalence of HIV and chronic comorbidities among older adults. AIDS 26:55–63
Collard RM, Boter H, Schoevers RA, Oude Voshaar RC (2012) Prevalence of frailty in community-dwelling older persons: a systematic review. J Am Geriatr Soc 60(8):1487–1492
Song X, Mitnitski A, Rockwood K (2010) Prevalence and 10-year outcomes of frailty in older adults in relation to deficit accumulation. J Am Geriatr Soc 58(4):681–687
Fortuna GR, Mueller EW, James LE, Shutter LA, Butler KL (2008) The impact of preinjury antiplatelet and anticoagulant pharmacotherapy on outcomes in elderly patients with hemorrhagic brain injury. Surgery 144(4):598–605
Sartorius D, Le Manach Y, David J-S, Rancurel E, Smail N, Thicoïpe M, Wiel E, Ricard-Hibon A, Berthier F, Gueugniaud P-Y et al (2010) Mechanism, glasgow coma scale, age, and arterial pressure (MGAP): a new simple prehospital triage score to predict mortality in trauma patients. Crit Care Med 38(3):831–837
Candefjord S, Asker L, Caragounis E-C (2020) Mortality of trauma patients treated at trauma centers compared to non-trauma centers in Sweden: a retrospective study. Eur J Trauma Emerg Surg 2020:1–12
MacKenzie EJ, Weir S, Rivara FP, Jurkovich GJ, Nathens AB, Wang W, Scharfstein DO, Salkever DS (2010) The value of trauma center care. J Trauma 69(1):1–10
Elkins MY (2010) Using PICO and the brief report to answer clinical questions. Nursing 40(4):59–60
Moher D, Liberati A, Tetzlaff J, Altman DG (2009) Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Ann Intern Med 151(4):264–269
Critical Appraisal Skills Programme. https://casp-uk.net/casp-tools-checklists/. Accessed 24 Feb 2020
Aveyard H (2014) Doing a literature review in health and social care: a practical guide. Open University Press, London
Chu I, Vaca F, Stratton S, Chakravarthy B, Hoonpongsimanont W, Lotfipour S (2007) Geriatric trauma care: challenges facing emergency medical services. Cal J Emerg Med 8(2):51–55
Neely J, Abbott H (2018) National standards for triaging elderly trauma patients. Anaesthesia 73(2):258
Platts-Mills TF, Evans CS, Brice JH (2016) Prehospital triage of injured older adults: thinking slow inside the golden hour. J Am Geriatr Soc 64(10):1941–1943
Scheetz LJ (2010) Prehospital factors associated with severe injury in older adults. Injury 41(9):886–893
Demetriades D, Sava J, Alo K, Newton E, Velmahos GC, Murray JA, Belzberg H, Asensio JA, Berne TV (2001) Old age as a criterion for trauma team activation. J Trauma 51(4):754–757
Fuller G, Pandor A, Essat M, Sabir L, Buckley-Woods H, Chatha H, Holt C, Keating S, Turner J (2021) Diagnostic accuracy of prehospital triage tools for identifying major trauma in elderly injured patients: a systematic review. J Trauma Acute Care Surg 90(2):403–412
Shifflette VK, Lorenzo M, Mangram AJ, Truitt MS, Amos JD, Dunn EL (2010) Should age be a factor to change from a level II to a level I trauma activation? J Trauma 69(1):88–92
Benjamin ER, Khor D, Cho J, Biswas S, Inaba K, Demetriades D (2018) The age of undertriage: current trauma triage criteria underestimate the role of age and comorbidities in early mortality. J Emerg Med 55(2):278–287
Newgard CD, Richardson D, Holmes JF, Rea TD, Hsia RY, Mann NC, Staudenmayer K, Barton ED, Bulger EM, Haukoos JS et al (2014) Physiologic field triage criteria for identifying seriously injured older adults. Prehosp Emerg Care 18(4):461–470
Brown JB, Gestring ML, Forsythe RM, Stassen NA, Billiar TR, Peitzman AB, Sperry JL (2015) Systolic blood pressure criteria in the National Trauma Triage Protocol for geriatric trauma: 110 is the new 90. J Trauma Acute Care Surg 78(2):352–359
Cox S, Morrison C, Cameron P, Smith K (2014) Advancing age and trauma: triage destination compliance and mortality in Victoria, Australia. Injury 45(9):1312–1319
Davis JS, Allan BJ, Sobowale O, Ivascu F, Orion K, Schulman CI (2012) Evaluation of a new elderly trauma triage algorithm. South Med J 105(9):447–451
Phillips S, Rond Iii PC, Kelly SM, Swartz PD (1996) The failure of triage criteria to identify geriatric patients with trauma: results from the Florida Trauma Triage Study. J Trauma 40(2):278–283
Pracht EE, Langland-Orban B, Flint L (2011) Survival advantage for elderly trauma patients treated in a designated trauma center. J Trauma Acute Care Surg 71(1):69–77
Scheetz LJ, Orazem JP (2020) The influence of sociodemographic factors on trauma center transport for severely injured older adults. Health Serv Res 55(3):411–418
Kodadek LM, Selvarajah S, Velopulos CG, Haut ER, Haider AH (2015) Undertriage of older trauma patients: is this a national phenomenon? J Surg Res 199(1):220–229
Newgard CD, Lin A, Eckstrom E, Caughey A, Malveau S, Griffiths D, Zive D, Bulger E (2019) Comorbidities, anticoagulants, and geriatric-specific physiology for the field triage of injured older adults. J Trauma Acute Care Surg 86(5):829–837
Amoako J, Evans S, Brown NV, Khaliqdina S, Caterino JM (2019) Identifying predictors of undertriage in injured older adults after implementation of statewide geriatric trauma triage criteria. Acad Emerg Med 2019:648–656
Caterino JM, Brown NV, Hamilton MW, Ichwan B, Khaliqdina S, Evans DC, Darbha S, Panchal AR, Shah MN (2016) Effect of geriatric-specific trauma triage criteria on outcomes in injured older adults: a statewide retrospective cohort study. J Am Geriatr Soc 64(10):1944–1951
Chang DC, Bass RR, Cornwell EE, MacKenzie EJ (2008) Undertriage of elderly trauma patients to state-designated trauma centers. Arch Surg 143(8):776–781
Garwe T, Stewart K, Stoner J, Newgard CD, Scott M, Zhang Y, Cathey T, Sacra J, Albrecht RM (2017) Out-of-hospital and inter-hospital under-triage to designated tertiary trauma centers among injured older adults: a 10-year statewide geospatial-adjusted analysis. Prehosp Emerg Care 21(6):734–743
Ichwan B, Darbha S, Shah MN, Thompson L, Evans DC, Boulger CT, Caterino JM (2015) Geriatric-specific triage criteria are more sensitive than standard adult criteria in identifying need for trauma center care in injured older adults. Ann Emerg Med 65(1):92–100
Lehmann R, Beekley A, Casey L, Salim A, Martin M (2009) The impact of advanced age on trauma triage decisions and outcomes: a statewide analysis. Am J Surg 197(5):571–575
Meyers MH, Wei TL, Cyr JM, Hunold TM, Shofer FS, Cowden CS, Moss CF, Jensen CE, Platts-Mills TF, Brice JH (2019) The triage of older adults with physiologic markers of serious injury using a state-wide prehospital plan. Prehosp Disaster Med 34(5):497–505
Nakamura Y, Daya M, Bulger EM, Schreiber M, Mackersie R, Hsia RY, Mann NC, Holmes JF, Staudenmayer K, Sturges Z et al (2012) Evaluating age in the field triage of injured persons. Ann Emerg Med 60(3):335–345
Newgard CD, Holmes JF, Haukoos JS, Bulger EM, Staudenmayer K, Wittwer L, Stecker E, Dai M, Hsia RY (2016) The Western Emergency Services Translational Research Network (WESTRN) Investigators: improving early identification of the high-risk elderly trauma patient by emergency medical services. Injury 47(1):19–25
Staudenmayer KL, Hsia RY, Mann NC, Spain DA, Newgard CD (2013) Triage of elderly trauma patients: a population-based perspective. J Am Coll Surg 217(4):569–576
Caterino JM, Raubenolt A, Cudnik MT (2011) Modification of Glasgow Coma Scale criteria for injured elders. Acad Emerg Med 18(10):1014–1021
Garwe T, Stewart KE, Newgard CD, Stoner JA, Sacra JC, Cody P, Oluborode B, Albrecht RM (2020) Survival benefit of treatment at or transfer to a tertiary trauma center among injured older adults. Prehosp Emerg Care 24(2):245–256
Horst MA, Morgan ME, Vernon TM, Bradburn EH, Cook AD, Shtayyeh T, D’Andrea L, Rogers FB (2020) The geriatric trauma patient: a neglected individual in a mature trauma system. J Trauma Acute Care Surg 89(1):192–198
Uribe-Leitz T, Jarman MP, Sturgeon DJ, Harlow AF, Lipsitz SR, Cooper Z, Salim A, Newgard CD, Haider AH (2020) National study of triage and access to trauma centers for older adults. Ann Emerg Med 75(2):125–135
Brown E, Tohira H, Bailey P, Fatovich D, Pereira G, Finn J (2019) Older age is associated with a reduced likelihood of ambulance transport to a trauma centre after major trauma in Perth. Emerg Med Australas 31(5):763–771
McCoy CE, Chakravarthy B, Lotfipour S (2013) Guidelines for field triage of injured patients: in conjunction with the Morbidity and Mortality Weekly Report published by the Center for Disease Control and Prevention. West J Emerg Med 14(1):69–76
Freshwater ES, Crouch R (2015) Technology for trauma: testing the validity of a smartphone app for pre-hospital clinicians. Int Emerg Nurs 23(1):32–37
Alshibani A, Singler B, Conroy S (2021) Towards improving prehospital triage for older trauma patients. Z Gerontol Geriatr
Alshibani A, Banerjee J, Lecky F, Coats TJ, Alharbi M, Conroy S (2021) New Horizons in understanding appropriate prehospital identification and trauma triage for older adults. Open Access Emerg Med 13:117–135
van Rein EA, van der Sluijs R, Raaijmaakers AM, Leenen LP, van Heijl M (2018) Compliance to prehospital trauma triage protocols worldwide: a systematic review. Injury 49(8):1373–1380
Alshibani A, Conroy S (2019) Building consensus to enhance research: a study protocol to determine the top issues to improve outcomes of silver trauma. LIAS Working Paper Series 2
Alshibani A, Banerjee J, Lecky F, Coats TJ, Prest R, Mitchell Á, Laithwaite E, Wensley M, Conroy S (2020) A consensus building exercise to determine research priorities for silver trauma. BMC Emerg Med 20(1):1–8
Funding
AA is funded by King Saud bin Abdulaziz University for Health Sciences, Saudi Arabia. The role of the fund is to cover publication fees for the systematic review.
Author information
Authors and Affiliations
Contributions
AA drafted the study protocol including the inclusion/exclusion criteria, the keywords and alternatives, the targeted databases, the appropriate critiquing tool, and the methods of reporting the study results. The study protocol was reviewed by MA and edited based on the agreement between the two authors. AA and MA individually screened the studies for inclusion and performed the quality assessment of the included studies. AA drafted the manuscript which was reviewed by MA and edited based on the agreement between the two authors. SC was a third reviewer who resolved any disagreement between the two authors during the development study protocol, performing the systematic review, and reporting its results. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no competing interests.
Ethics approval
This article does not contain any studies with human participants or animals performed by any of the authors.
Informed consent
For this type of study, no informed consent is required.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Alshibani, A., Alharbi, M. & Conroy, S. Under-triage of older trauma patients in prehospital care: a systematic review. Eur Geriatr Med 12, 903–919 (2021). https://doi.org/10.1007/s41999-021-00512-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s41999-021-00512-5