Key summary points
This scoping review examined the effectiveness of intermediate care including transitional care interventions for middle-aged and older adults on function, healthcare utilisation, and costs.
AbstractSection FindingsWhile some studies report positive outcomes on hospital utilisation, the evidence is limited for their effectiveness on emergency department attendances, institutionalisation, function, and cost-effectiveness.
AbstractSection MessageIntermediate care including transitional care interventions were associated with reduced hospital stay but this finding was not universal.
Abstract
Background and aim
Intermediate care describes services, including transitional care, that support the needs of middle-aged and older adults during care transitions and between different settings. This scoping review aimed to examine the effectiveness of intermediate care including transitional care interventions for middle-aged and older adults on function, healthcare utilisation, and costs.
Design
A scoping review of the literature was conducted including studies published between 2002 and 2019 with a transitional care and/or intermediate care intervention for adults aged ≥ 50. Searches were performed in CINAHL, Cochrane Library, EMBASE, Open Grey and PubMed databases. Qualitative and quantitative approaches were employed for data synthesis.
Results
In all, 133 studies were included. Interventions were grouped under four models of care: (a) Hospital-based transitional care (n = 8), (b) Transitional care delivered at discharge and up to 30 days after discharge (n = 70), (c) Intermediate care at home (n = 41), and (d) Intermediate care delivered in a community hospital, care home or post-acute facility (n = 14). While these models were associated with a reduced hospital stay, this was not universal. Intermediate including transitional care services combined with telephone follow-up and coaching support were reported to reduce short and long-term hospital re-admissions. Evidence for improved ADL function was strongest for intermediate care delivered by an interdisciplinary team with rehabilitation at home. Study design and types of interventions were markedly heterogenous, limiting comparability.
Conclusions
Although many studies report that intermediate care including transitional care models reduce hospital utilisation, results were mixed. There is limited evidence for the effectiveness of these services on function, institutionalisation, emergency department attendances, or on cost-effectiveness.
Similar content being viewed by others
Introduction
Intermediate care including transitional care services are models of care that support the integration and continuity of care as well as prevention of avoidable admissions to hospital [1,2,3]. They have a particular importance in preventing the onset and progression of frailty and functional decline in adults, particularly older adults [4, 5] since they provide comprehensive geriatric assessment, enablement and rehabilitation aimed at optimising independence and recovery [4,5,6]. These services are time limited [7] as they are mainly employed at times of a deterioration in health or at times of transition such as when moving from one’s home to hospital, assisted living or long-term care [8, 9].
These models operate as part of the continuum of care. They help manage preventable complications associated with hospitalisation and enable older adults to maintain or recover their functional ability following an illness, injury or hospital admission [6, 10]. A recent Delphi study examining these models emphasised that intermediate care is a broad range of time-limited services, ranging from crisis response to support over weeks to months that aims to ensure continuity, improve quality of care and promote recovery, particular at transitions between different levels of care and settings [11],transitional care interventions may be delivered as a subset of intermediate care [11, 12]. Although transitional and intermediate care services may be limited to several weeks [13, 14], they are more comprehensive than discharge planning activities or chronic care management [11]. In addition, both services provide care closer to home, support early discharge and reduce readmission to acute care [15, 16].
Despite the recent growth in their use as a bridge to care transitions, there is limited data on the impact of these relatively new models of care on activities of daily living (ADL) function-related outcomes, healthcare utilisation and cost-effectiveness for adults, particularly older, frail and multi-morbid adults [17]. Therefore, this scoping review seeks to identify and analyse a broad range of literature published in relation to the effectiveness of intermediate care including transitional care for middle-aged and older adults and to understand the benefits of these interventions, with a specific focus on health-related outcomes including function (activities of daily living), healthcare use and associated costs.
Methods
Scoping reviews are conducted as a preliminary investigation to assess the potential size and scope of available research literature on a topic [18]. They are useful in summarising evidence to show the breadth and depth of a given field [19]. This scoping review was conducted to incorporate evidence from the existing literature across a broad range of study designs regarding the effectiveness of intermediate and transitional care interventions for middle-aged and older adults. The methodological framework recommended by Arksey and O’Malley [20] for conducting a scoping review was used and the following steps were taken: 1-identification of the research question, 2-identifying relevant studies, 3-study selection, 4-charting the data, 5-collating, summarising and reporting the results.
Protocol and registration
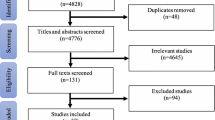
The Preferred Reporting Items for Systematic Review and Meta-Analyses (PRISMA) extension for scoping reviews (PRISMA-ScR) guidelines were used for reporting purposes [21]. The review protocol was registered on PROSPERO (CRD42019122982).
Objectives
The primary objective of this scoping review was to identify the effectiveness of intermediate care including transitional care interventions for middle-aged and older adults (aged ≥ 50) in the existing literature.
The following research questions were explored:
-
What are the models of intermediate and transitional care provided in different care settings?
-
Is there evidence for their effectiveness in improving function, and reducing hospital length of stay, Emergency Department (ED) admissions, institutionalisation, and health and social care costs for middle-aged and older adults?
-
Are intermediate and transitional care interventions effective for other outcomes such as satisfaction with care transitions, quality of life, and adherence to treatment plans?
Information sources
The search was conducted in four databases, CINAHL, Cochrane Library, EMBASE, and PubMed, using the search string: ((“intermediate care” OR “transitional care”) AND (frailty OR frail OR “older person*” OR “older adult*” OR “hospital at home” OR “reablement” OR “independ*” OR “readmission” OR “prolonged stay” OR “community hospital”)). OpenGrey was also searched with the terms “intermediate care” or “transitional care” for reports published within the same period.
Eligibility criteria
Studies that investigated the effectiveness of intermediate or transitional care interventions for adults aged 50 and over were included from peer-reviewed literature published between 01/01/2002 and 05/02/2019 in English, French, Italian or Spanish. Any care setting was considered.
Selection of sources of evidence
Articles and grey literature that met the following criteria were included: (a) report an intervention for intermediate or transitional care; (b) had a sample of adults aged 50 and over or mean age of the sample was at least 50; (c) conducted in any health care setting; (d) published in English, French, Italian or Spanish; (e) published between 01 January 2002 and 05 February 2019; and (f) had full text available. Any articles and grey literature that did not meet these criteria were excluded.
Titles and/or abstracts (where available) of the located records were independently screened by three pairs of reviewers (DS-AH, AMC-LLS, RRA-CAC) considering the inclusion and exclusion criteria. Disagreements were discussed by the pairs of reviewers and any persisting conflict was resolved by a third independent reviewer. Data extraction was performed by five reviewers (DS, AH, MOD, MS, LLS) for the full-text records.
Data charting process and data items
Data extraction was carried out using a single standard template. This template had fifteen sections including: (1) Author names, year, title, and country; (2) Evidence type; (3) Aim of study; (4) Definitions provided for transitional or intermediate care; (5) Intervention details; (6) Technology usage; (7) Population characteristics (such as mean age and sample size); (8) Health condition/problem; (9) Context/setting that the recruitment took place; (10) Structure/governance of intervention; (11) Outcomes reported (function, ED visits, hospital stay, institutionalisation, other); (12) Resource implications (such as cost and staffing); (13) Transferable lessons for policy and practice; (14) Barriers/limitations reported; and (15) Additional recommendations/comments.
Synthesis of the results
Qualitative and quantitative analyses of the included studies were performed. The included studies were read in detail and were grouped and classified according to their type and setting. The measures captured by the data extraction template guided the data synthesis process (supplementary file). Classification and synthesis of studies were discussed within the team and decisions were made with consensus. A core team of reviewers (DS, AH, MOD, MS) had regular email correspondence and virtual meetings to classify and synthesise data from included studies.
Results
The initial search yielded 1891 records. Cross-referencing of a systematic review and narrative review articles resulted in 79 additional articles. The search for grey literature added a further 14 reports, resulting in a total of 1984 articles for screening. Further details of the screening process are outlined in Fig. 1 (PRISMA-ScR flow diagram). In total, 133 studies measuring the effectiveness of transitional and/or intermediate care interventions in middle-aged and older adults (aged ≥ 50) were identified. Details on the characteristics and outcomes of these studies are summarised in the supplementary file. In summary, the total number of participants in the included studies were 703,523, with the sample sizes ranging between 21 and 552,414 (available for 130 studies). Most studies were from the USA (n = 75). Eighty studies reported the mean age of their participants, which ranged between 50–86.2 years. Overall, the mean age was 73.6 ± 9.48 years. Twenty-nine interventions were delivered to high-risk patient populations, e.g. those with advanced age, high risk of readmission, multimorbidity, though there was no standard description for high-risk. Only three interventions were designed primarily for frail older adults. Interventions were heterogeneous, and most were complex, consisting of a mixture of multiple elements delivered in hospital and/or in the community settings. In total, sixty-five studies were delivered by interdisciplinary teams. As illustrated in Tables 1, 2 and Fig. 2, the interventions were grouped under four main categories based on the type of evidence, location, timing of care and healthcare outcomes:
Transitional care interventions delivered only in the hospital
Only eight studies examined transitional care interventions delivered exclusively in the hospital. These focused on co-ordination and hospital-based education for patients and/or caregivers and implemented discharge planning, of which the majority were a nurse or social worker-led interventions. Reduced readmission was observed for coaching delivered by social workers [22], as well as some transitional care interventions delivered by hospitalists or nurses [23, 24]. While no reductions in readmissions were reported for a combination of patient education and discharge planning by nurses or social workers, reduced rates of admission to long-term care was observed [25].
Transitional care interventions delivered at discharge and up to 30 days after discharge
Many studies (53%) reported on transitional care delivered in hospital and for up to 30 days after discharge, with fifty-five conducted in the USA or Canada, six in Hong Kong, six in Europe, and three in Australia. Most comprised a complex bundle of interventions in hospital and in the community delivered by a nurse, pharmacist or social worker; and 22 (30%) were interdisciplinary. Since these complex multi-component interventions were very heterogenous, the studies were further classified according to their provider, approach and specific focus, to better describe the potential benefits and value. Some studies were included under more than one category.
Service provider and approach
Outreach by hospital professional(s) (n = 51)
The majority of studies implemented and evaluated combined interventions including education, assessment, follow-up, medication management and other interventions but were markedly heterogenous. Outreach by a hospital-based professional, often a nurse, was described in most of the transitional care models. Key positive outcomes of these interventions were on hospital readmissions (n = 34), ED visits (n = 8), and costs (n = 6). Only one study reported positive outcomes related to function [26], none were reported for institutional care. For example, a telephone-based nurse-led outreach model, aiming at empowering older adults and caregivers in medication management and encouraging them to contact healthcare providers when needed, reduced 30-day re-hospitalisation rates from 34 to 23% [27] and led to estimated net healthcare cost savings of $663 per person [28].
One-third of the outreach interventions associated with reduced hospital stay were delivered via interdisciplinary teams. An example of an outreach transitional care programme is The Bridge Care Coordinator model, which involves discussion of the cases within a multidisciplinary hospital team, review of inpatient medical records by a social worker, and home follow-up visits. The Bridge Care model also reported reductions in 30-day re-hospitalisation by 20% [29], with average hospital costs reduced by $14,150 per person per episode of care [30].
Community based or in-reach models (n = 24)
Community-based providers were involved in less than half of the post-discharge transitional care interventions. These models were mostly associated with reduced hospital stay [31], fewer rehospitalisations (reductions ranged between 2.2–43%) (n = 17), and lower costs (ranged between $192–1964 per patient, where applicable) (n = 7). Few illustrated positive outcomes on ED visits (n = 3) and ADL function (n = 3). None reported outcomes on institutional care. Almost all the models (n = 16) that were associated with reduced hospital stay consisted of combined interventions, six of which were delivered via interdisciplinary teams. All interventions that reported reduced costs implemented patient or carer education and used telephone support.
A large retrospective study of The Preventable Admissions Care Team, an in-reach model involving a social worker-led in-hospital holistic assessment and personalised care planning, followed by home-based post-discharge care coordination, illustrated significantly lower readmissions at 30, 60 and 90 days, and reduced mortality at over 180 days [32]. Similarly, a transitional case management programme in the USA involved immediate identification and telephone services for recently discharged patients (mean age 58) [33], reduced readmissions at 30 and 180 days. Pre- and post-discharge assessments for care needs, medication reconciliation, support for self-care delivered by a primary care-based nurse care coordinator reduced post-discharge costs among 638 Medicare fee-for-service beneficiaries discharged from hospital and the primary care provider in the USA [34].
Transitional care clinics (n = 7)
Transitional care clinics were assessed in seven studies and were often combined with telephone and/or nurse follow up. A retrospective study [35] reported reduced rehospitalisation for patients who completed a scheduled transition clinic appointment compared with those who neither attended the transition clinic nor their primary care physician. Similarly, a reduction in re-hospitalisation, as well as potential Medicare savings were observed by Baldwin et al. [36] for patients attending a multidisciplinary discharge clinic in the USA.
Focus of the interventions
Telephone follow-up (n = 69)
Forty-eight studies illustrated a variety of telephone support interventions ranging from one or two ‘light touch’ prompts in the first few days after discharge to more frequent calls for up to 30 days after discharge. The effectiveness of telephone support was mixed. For example, a RCT including 1950 participants (974 intervention, 975 control) aged ≥ 65 (mean age 74) [37] reported insignificant results for a single scripted telephone call from a trained nurse following discharge from the ED for 30-day rehospitalisation or death. However, a pre-discharge holistic assessment and telephone support by a social worker at 30 days for medical and surgical inpatients aged ≥ 65 improved adherence with follow-up appointments in primary care settings [38].
Twenty-one studies (30%) conducted home visits alongside telephone follow-up as part of their intervention. There was mixed evidence for a reduction in re-hospitalisation for interventions delivered by different healthcare professionals. For example, a pilot study [39] investigating home visits by social workers in 620 high-risk patients in the USA reported lower ED visits and rehospitalisation at 30 days post-discharge. Similarly, home visits on day five post-discharge by a pharmacist [40] reduced 90-day unplanned rehospitalisation and improved compliance in those aged ≥ 60 (median age 74) in Australia. However, in another study, home visits by pharmacists at two and eight weeks post-discharge were linked to increased hospitalisation in 872 patients with emergency admission aged ≥ 80 (mean age 85) in the United Kingdom [41].
Patient and caregiver education or coaching (n = 65)
Almost all transitional care interventions included patient and/or carer education or coaching. There was a specific focus on medication management in half of the studies while the others investigated the effects of coaching and support to prevent additional treatment or review. Results in relation to costs and readmissions were generally positive [42,43,44]. Other outcomes included improvements in patient satisfaction [45,46,47], quality of life [47, 48], improved information sharing and communication with members of the healthcare team and self-management [49, 50], as well as improved self-rated health and self-efficacy [47, 51].
Decision support systems (n = 5)
Electronic health records and patient information tools were used in most studies; however, few (n = 5) described specific decision support tools as the main element of their intervention. Although they provided mixed evidence on readmissions [52,53,54], there were positive outcomes in relation to healthcare adherence and quality of care [54, 55]. For example, a RCT implementing electronic transfer of patient discharge forms reported improved post-discharge outpatient follow-up rates in a diverse group of patients (mean age 58) admitted to a small community teaching hospital in the USA [55]. Another study in the USA, deploying a transitional care bundle using patient-centred electronic data collection tools, supported the spread of transitional care across multiple sites and reduced medication errors in patients with a mean age of 54, half of whom had a high risk of readmission [54].
Intermediate care delivered at home
Forty-one studies of intermediate care delivered at home were identified with thirteen studies conducted in North America, 12 in Australia or New Zealand, 11 in Europe, four in Singapore and one in Thailand. While 12 studies had a focus on medication reconciliation and review, all combined several interventions including telephone advice and support, coaching for self-management and recovery, and follow up care.
Several intermediate care interventions delivered at home reported no evidence on length of hospital stay [56, 57] or reduced hospital readmission rates [56, 58,59,60]. However, many combined interventions had positive effects on reducing short-term and long-term (re)hospitalisation rates [61,62,63,64,65,66,67,68,69] reducing ED visits [65], improving quality of life [61], and reducing costs [69].
Due to heterogeneity between studies, the interventions were grouped by the professionals supporting the interventions and their approach to care (Table 3).
Professionals delivering the interventions
Interdisciplinary support with rehabilitation (n = 19)
Interdisciplinary rehabilitation was included in 46% of the intermediate care interventions at home. Many were geriatrician or physician-led programmes with collaboration of a team of nurses, allied health professionals, and social care workers, and employed a comprehensive geriatric assessment approach. Their focus was on improving function in middle-aged and older adults and re-able them to be independent in their ADL. For example, an early supported discharge with an intensive multidisciplinary community rehabilitation programme in England [13] reduced mean length of hospital stay by nine days and led to improved ADL and psychological well-being in older adults aged ≥ 65 (median age 80). Similarly, an Australian study [62] reported improvements in instrumental ADL scores from a combined nurse and physiotherapy intervention at home delivered to 128 participants aged ≥ 65 (mean age 78).
Interdisciplinary support without rehabilitation (n = 12)
Half of the interdisciplinary programmes did not deliver a rehabilitation intervention but used combined approaches including time-limited case management usually by a trained nurse. Those were mostly from the USA (n = 5) and Singapore (n = 3), followed by a few European countries. For example, Hernández et al. [70] reported reduced in-hospital days following a hospital outreach telemedicine monitoring service for a large group of patients with chronic illnesses (n = 4165). Furthermore, all patients, carers and health professionals involved in the programme expressed high levels of satisfaction (98%) with the service.
On the other hand, intermediate care at home for recovery and self-management illustrated mixed outcomes for ADL and IADL scores. A transitional care bridge programme delivered by a transitional care nurse and geriatrician, without rehabilitation, showed no effect on ADL functioning but decreased 6-month post-hospitalisation risk of death [7].
Single profession led interventions (n = 10)
Ten studies included uni-disciplinary support, mostly nurse-delivered interventions. They were mostly associated with positive outcomes related to hospital utilisation and readmissions. For example, an extended transitional case management programme delivered by an advance nurse practitioner decreased 3-month rehospitalisation and total hospital days, resulting in decreased health care costs [66]. Similarly, support for self-management and coaching by a nurse coordinator reduced rehospitalisation and ED attendance at 4–6 weeks post-discharge and increased quality of life and self-rated health [71].
Approach to care
Crisis response or hospital admission avoidance (n = 7)
Seven studies reported outcomes of hospital avoidance or crisis response models, while some of them were built on an established early supported discharge service. They had limited evidence on cost effectiveness [72] but reported positive outcomes for patients and caregivers [3, 72,73,74]. For example, a nurse-led multidisciplinary hospital at home intervention via a hospital outreach programme increased patient satisfaction and decreased Caregiver Strain Index scores [72]. Despite the fact that this hospital at home service was not cost effective, this was explained as being due to not operating the service at its full capacity. Avoided costs were not reported [72].
The setting for follow-up
Except one, all intermediate care at home interventions implemented home visits. Follow-up services delivered via home visits during the post-discharge period were associated with improved communication [56] and patient satisfaction with care [75]. In addition, compared to outpatient provider visits, home visits within a week following discharge from a skilled nursing facility (SNF) reduced the risk of 30-day rehospitalisation [76].
Intermediate care delivered in a community hospital, care home or post-acute facility
Fourteen studies reported the effectiveness of bed-based intermediate care. These were mostly from Europe (n = 8), followed by North America (n = 5) and Australia (n = 1). Many investigated the effect of having beds dedicated to rehabilitation in community hospitals or residential care units. For example, a discharge to intermediate care hospital intervention resulted in fewer days spent in intermediate care beds during a 1-year period [77]. The most frequently reported outcome was hospitalisation, with 11 studies reporting reduced length of stay or readmissions. Three out of five studies considering long term care as their endpoint observed reduced institutionalisation [78,79,80].
All the facilities aimed to ensure recovery and provide rehabilitation via teams consisting of nurses, allied health professionals, or social care workers. Since there were differences in relation to the content of the services, the timing of transfer, and support provided for staff members, the interventions were grouped according to several features.
Assessment and rehabilitation (n = 11)
Eleven studies implemented interdisciplinary rehabilitation via in-reach support or in patient facilities (community hospitals). Most of the rehabilitation activities were delivered on site or by telephone advice by interdisciplinary teams led by physicians. The main outcomes included reduced hospitalisation and improved function. For example, telephone-based medical consultations delivered by telephone to support on-site care teams decreased hospital costs and shortened the length of hospital stay [81]. Another intervention by a community hospital providing intermediate care closer to home and to social and care networks increased independence and reduced mortality at 12 months [82, 83].
Rapid transfer from acute care (n = 3)
Three studies conducted in different community settings addressed early transfer from acute care settings to bed-based intermediate care. In general, they had positive effects on function and independence [79, 84]. For example, Young and colleagues [84] reported that early transfer to a community hospital for older patients with complex care needs improved their ADL.
Education and training for existing staff (n = 3)
Three studies considered the effectiveness of education for staff members in bed-based intermediate care units. Their outcomes included reduced readmissions and ED visits [85, 86]. For example, education and training for SNF staff members who coordinate discharges reduced 30-day rehospitalisation and enhanced patients’ preparedness for discharge [86].
Discussion
This scoping review provides an analysis of the effectiveness of a wide range of intermediate care including transitional care models for middle-aged and older adults. Since they were conducted in many different care settings, applied different inclusion criteria and evaluated a range of different outcomes (i.e. re-hospitalisation, ED admissions, and healthcare costs as well as function), the studies were inherently heterogeneous. Given this, it was challenging to identify and summarise a common pattern for effectiveness and value, questioning the generalisability of the overall findings for service planning and clinical practice. Nevertheless, following further analyses, we were able to synthesise the results and classify and group services under four different models of care: hospital-based transitional care, transitional care interventions, intermediate care at home and bed-based intermediate care, the findings of which are discussed in turn below.
Hospital-based transitional care was described in a small number of studies that reported mixed results in relation to reductions in hospital readmission of middle-aged and older adults, for all disciplines that conducted a planning and coaching based transitional care intervention. In the literature, a Cochrane review by Griffiths et al. [15] reported limited evidence for the effectiveness of nursing-led units for care transitions. Although there were improved processes and positive outcomes for preparing patients for discharge within those units, more research was recommended to prove their effectiveness. In our scoping review, the strongest evidence for effectiveness and costs was from interventions for older adults utilising a multidisciplinary Comprehensive Geriatric Assessment (CGA) [87], where €519 was saved per person and ED or hospital (re)admissions were reduced by 7.5% over three months post-discharge.
Transitional care interventions in both hospital outreach and community settings illustrated positive outcomes including positive patient experience, self-management, self-efficacy, and self-rated health. Benefits were also observed at the healthcare system level with reductions in early hospital readmissions as well as ED admissions. Transitional care interventions can bridge the gap between acute care and community settings and so ensure the continuity of care [88]. They can also help address the changing needs of middle-aged and older adults at post-discharge periods [89]. We identified that post-discharge telephone follow-up was a low-cost intervention that reached a high volume of patients in transitional services yet the evidence for their effectiveness is limited.
Intermediate care at home showed benefits for short-term and long-term re-hospitalisation rates, ED admissions, function, and healthcare costs. Evidence was strongest for discharge supported by an interdisciplinary team and rehabilitation at home. This outcome was also encouraging for hospital avoidance of middle-aged and older adults but there was a limited number of empirical studies to support this evidence. In practice settings, both early supported discharge and intermediate care at home are provided by services considering the individualised needs of the patients and families. A systematic (Cochrane) review of 16 RCTs for admission avoidance using hospital at home models [90] concluded that if this type of service provides the option of hospital transfers when needed, it could be an effective alternative to hospital care. Services providing early supported discharge can offer crisis response as well as hospital at home alternatives, which aid building confidence and capacity in patients and their families and/or informal caregivers for managing clinical risks. However, more evidence in this area is needed.
Shepperd et al. [91] reported in their Cochrane review that early discharge to a hospital at home model is a cost-effective alternative to usual care and it also aids improvements in health. However, a more recent version of this systematic review [92] concluded that although early discharge hospital at home services are cheaper options compared to inpatient care, there is no strong evidence for their economic efficiency or support for improvements in health. Although we found some evidence for cost benefits and positive outcomes for intermediate care at home, more research is needed to identify cost-effectiveness at scale.
Bed-based intermediate care interventions reported reduced readmission rates and length of hospital stay, although few reported reduced admissions to long-term institutional care. Enhanced specialist team support was most likely to be effective, however, there was no evidence to specifically identify the ideal provider or optimal care setting. In addition, no studies made comparisons between intermediate care provided in different settings such as a community hospital, nursing facility, residential care home, or transitional care unit.
This paper has a number of strengths and weaknesses. This scoping review was conducted by academics and clinicians from a variety of disciplines across multiple European countries providing an international and interdisciplinary standpoint. A broad perspective on the transitional and intermediate care interventions was ensured since no restrictions were placed on the setting or level of evidence. Despite these factors, this review has some limitations. Firstly, the heterogeneous nature of the interventions resulted in barriers to data synthesis, which did not make it possible to perform a systematic review and meta-analysis. To overcome this issue, the data were classified according to the timing and setting of interventions and synthesised according to their principal elements. Secondly, given our broad focus on middle-aged and older adults, we did not include condition-specific interventions, such as stroke rehabilitation (e.g. ESD for stroke). We did, however, identify and include three studies [59, 60, 93] deploying interventions designed for frail older adults. Once again, these interventions were markedly different in their approach.
Intermediate care and COVID-19
Although this review includes papers published before the ongoing global COVID-19 pandemic, it is important to acknowledge the important role intermediate care is playing in managing those with and without COVID-19. COVID-19 is known to disproportionally affect older adults, particularly those who are frail [94, 95]. Worldwide, alternatives to hospital treatment have been scaled-up during the pandemic through virtual consultations and access to intermediate care at home and in step-up and step-down facilities. Although the challenges and effectiveness of delivering intermediate care during this pandemic are yet to be investigated, it features in pathways for those recovering from COVID-19 who require support and rehabilitation as they transition to home or long-term care [96].
Conclusions
Intermediate care generally consists of a series of multidimensional services combining transitional care with complex rehabilitation and recovery alternatives within interdisciplinary and integrated team work [4,5,6, 11, 97,98,99]. Overall, intermediate including transitional care models can provide positive outcomes for middle-aged and older adults and make an important contribution to healthcare systems, despite the challenges of delivering such complex services in different settings due to a high volume of interventions and costs. When models of care combine telephone follow-up and coaching support, they can reduce short and long term hospital re-admissions. Moreover, ‘rehabilitation at home’ services delivered via an interdisciplinary team, demonstrated improvements in ADL function. Although several intermediate and transitional care interventions resulted in reductions in hospital utilisation and improvements in quality of life, their effectiveness on function, ED admissions, institutionalisation for long-term care and costs remains unclear. Additional studies are now required to investigate the impact of these models on middle-aged and older adults within the broader health and social care context to compare whether outcomes vary for different settings and providers of care. Considering the heterogeneity of the interventions reported in the literature, there is a need for systematic reviews and meta-analyses with a specific focus on high-quality experimental studies and in particular healthcare settings, which may allow more robust comparisons between previously reported interventions.
Data availability
The relevant data can be provided to interested individuals on request.
References
Gillis D, Demmons J, Rocker G (2017) Expanding the INSPIRED COPD Outreach Program to the emergency department: a feasibility assessment. Int J Chron Obstruct Pulmon Dis. 12:1597–1604. https://doi.org/10.2147/COPD.S136183
Colineaux H, Pelissier F, Pourcel L, Lang T, Kelly-Irving M, Azema O et al (2019) Why are people increasingly attending the emergency department? A study of the French healthcare system. Emerg Med J 36(9):548–553. https://doi.org/10.1136/emermed-2018-208333
Mas MA, Inzitari M, Sabate S, Santaeugenia SJ, Miralles R (2017) Hospital-at-home Integrated Care Programme for the management of disabling health crises in older patients: comparison with bed-based Intermediate Care. Age Ageing 46(6):925–931. https://doi.org/10.1093/ageing/afx099
Peel NM, Hubbard RE, Gray LC (2013) Impact of post-acute transition care for frail older people: a prospective study. J Frailty Aging. 2(3):165–171. https://doi.org/10.14283/jfa.2013.24
Loeffler K (2016) Geriatric intermediate care and transitional care for frailty-related patients: Kerstin Loeffler. Eur J Public Health. 26(suppl_1):426–427. https://doi.org/10.1093/eurpub/ckw174.246
Lowthian J (2017) How do we optimise care transition of frail older people? Age Ageing 46(1):2–4. https://doi.org/10.1093/ageing/afw171
Buurman BM, Parlevliet JL, Allore HG, Blok W, van Deelen BA, Moll van Charante EP et al (2016) Comprehensive geriatric assessment and transitional care in acutely hospitalized patients: the transitional care bridge randomized clinical trial. JAMA Intern Med. 176(3):302–309. https://doi.org/10.1001/jamainternmed.2015.8042
World Health Organisation (2016) Transitions of care: technical series on safer primary care. Geneva, Switzerland. https://apps.who.int/iris/bitstream/handle/10665/252272/9789241511599-eng.pdf;jsessionid=6A36810C45C0E99A4AAD8EF25ADB4B28?sequence=1. Accessed 10 Dec 2019
Coleman EA, Boult C (2003) Improving the quality of transitional care for persons with complex care needs. J Am Geriatr Soc 51(4):556–557. https://doi.org/10.1046/j.1532-5415.2003.51186.x
Naylor MD (2006) Transitional care: a critical dimension of the home healthcare quality agenda. J Healthc Qual 28(1):48–54
Sezgin D, O'Caoimh R, O'Donovan M, Salem M, Kennelly S, Samaniego LL et al (2020) Defining the characteristics of intermediate care models including transitional care: an international Delphi study. Aging Clin Exp Res. https://doi.org/10.1007/s40520-020-01579-z
Allen J, Hutchinson AM, Brown R, Livingston PM (2014) Quality care outcomes following transitional care interventions for older people from hospital to home: a systematic review. BMC Health Serv Res 15(14):346. https://doi.org/10.1186/1472-6963-14-346
Miller P, Gladman JR, Cunliffe AL, Husbands SL, Dewey ME, Harwood RH (2005) Economic analysis of an early discharge rehabilitation service for older people. Age Ageing 34(3):274–280. https://doi.org/10.1093/ageing/afi058
Khanna PB, Bhowmick B (2008) Training implications of developments in intermediate care. Rev Clin Gerontol 18(2):159–164. https://doi.org/10.1017/s0959259809002810
Griffiths PD, Edwards MH, Forbes A, Harris RL, Ritchie G (2007) Effectiveness of intermediate care in nursing-led in-patient units. Cochrane Database Syst Rev. 2:CD02214. https://doi.org/10.1002/14651858.CD002214.pub3
Kansagara D, Chiovaro JC, Kagen D, Jencks S, Rhyne K, O'Neil M et al (2016) So many options, where do we start? An overview of the care transitions literature. J Hosp Med 11(3):221–230. https://doi.org/10.1002/jhm.2502
Sezgin D, Hendry A, Liew A, O'Donovan M, Salem M, Carriazo AM et al (2020) Transitional palliative care interventions for older adults with advanced non-malignant diseases and frailty: a systematic review. J Integr Care. https://doi.org/10.1108/JICA-02-2020-0012
Grant MJ, Booth A (2009) A typology of reviews: an analysis of 14 review types and associated methodologies. Health Inf Libr J 26(2):91–108. https://doi.org/10.1111/j.1471-1842.2009.00848.x
Levac D, Colquhoun H, O'Brien KK (2010) Scoping studies: advancing the methodology. Implement Sci 5(1):69. https://doi.org/10.1186/1748-5908-5-69
Arksey H, O'Malley L (2005) Scoping studies: towards a methodological framework. Int J Soc Res Methodol 8(1):19–32. https://doi.org/10.1080/1364557032000119616
Tricco AC, Lillie E, Zarin W, O'Brien KK, Colquhoun H, Levac D et al (2018) PRISMA extension for scoping reviews (PRISMA-ScR): checklist and explanation. Ann Intern Med 169(7):467–473. https://doi.org/10.7326/M18-0850
Adler A, Lipkin C, Cooper L, Agolino M, Jones V (2009) Effect of social work intervention on hospital discharge transition planning in a special needs population. Managed care 18(11):50–53
Dedhia P, Kravet S, Bulger J, Hinson T, Sridharan A, Kolodner K et al (2009) A quality improvement intervention to facilitate the transition of older adults from three hospitals back to their homes. J Am Geriatr Soc 57(9):1540–1546. https://doi.org/10.1111/j.1532-5415.2009.02430.x
Hwang U, Dresden SM, Rosenberg MS, Garrido MM, Loo G, Sze J et al (2018) Geriatric emergency department innovations: transitional care nurses and hospital use. J Am Geriatr Soc 66(3):459–466. https://doi.org/10.1111/jgs.15235
Steeman E, Moons P, Milisen K, De Bal N, De Geest S, De Froidmont C et al (2006) Implementation of discharge management for geriatric patients at risk of readmission or institutionalization. Int J Qual Health Care 18(5):352–358. https://doi.org/10.1093/intqhc/mzl026
Wilcox D, McCauley PS, Delaney C, Molony SL (2018) Evaluation of a Hospital: community partnership to reduce 30-day readmissions. Prof Case Manag 23(6):327–341. https://doi.org/10.1097/NCM.0000000000000311
Kind AJH, Jensen L, Barczi S, Bridges A, Kordahl R, Smith MA et al (2012) Low-cost transitional care with nurse managers making mostly phone contact with patients cut rehospitalization at A VA Hospital. Health Aff 31(12):2659–2668. https://doi.org/10.1377/hlthaff.2012.0366
Kind AJ, Brenny-Fitzpatrick M, Leahy-Gross K, Mirr J, Chapman E, Frey B et al (2016) Harnessing protocolized adaptation in dissemination: successful implementation and sustainment of the veterans affairs coordinated-transitional care program in a non-veterans affairs hospital. J Am Geriatr Soc 64(2):409–416. https://doi.org/10.1111/jgs.13935
Boutwell AE, Johnson MB, Watkins R (2016) Analysis of a social work-based model of transitional care to reduce hospital readmissions: preliminary data. J Am Geriatr Soc 64(5):1104–1107. https://doi.org/10.1111/jgs.14086
Xiang X, Zuverink A, Rosenberg W, Mahmoudi E (2019) Social work-based transitional care intervention for super utilizers of medical care: a retrospective analysis of the bridge model for super utilizers. Soc Work Health Care. 58(1):126–141. https://doi.org/10.1080/00981389.2018.1547345
Misky GJ, Wald HL, Coleman EA (2010) Post-hospitalization transitions: examining the effects of timing of primary care provider follow-up. J Hosp Med 5(7):392–397. https://doi.org/10.1002/jhm.666
Weerahandi H, Basso Lipani M, Kalman J, Sosunov E, Colgan C, Bernstein S et al (2015) Effects of a psychosocial transitional care model on hospitalizations and cost of care for high utilizers. Soc Work Health Care. 54(6):485–498. https://doi.org/10.1080/00981389.2015.1040141
Farrell WT, Farrell TW (2015) Impact of an integrated transition management program in primary care on hospital readmissions. J Healthc Qual 37(1):81–92. https://doi.org/10.1097/01.JHQ.0000460119.68190.98
Kranker K, Barterian LM, Sarwar R, Peterson GG, Gilman B, Blue L et al (2018) Rural hospital transitional care program reduces medicare spending. Am J Manag Care 24(5):256–260
Chakravarthy V, Ryan MJ, Jaffer A, Golden R, McClenton R, Kim J et al (2018) Efficacy of a transition clinic on hospital readmissions. Am J Med 131(2):178–184. https://doi.org/10.1016/j.amjmed.2017.08.037
Baldwin SM, Zook S, Sandford J (2018) Implementing posthospital interprofessional care team visits to improve care transitions and decrease hospital readmission rates. Prof Case Manag 23(5):264–271. https://doi.org/10.1097/NCM.0000000000000284
Biese KJ, Busby-Whitehead J, Cai J, Stearns SC, Roberts E, Mihas P et al (2018) Telephone follow-up for older adults discharged to home from the emergency department: a pragmatic randomized controlled trial. J Am Geriatr Soc 66(3):452–458. https://doi.org/10.1111/jgs.15142
Altfeld SJ, Shier GE, Rooney M, Johnson TJ, Golden RL, Karavolos K et al (2013) Effects of an enhanced discharge planning intervention for hospitalized older adults: a randomized trial. Gerontologist 53(3):430–440. https://doi.org/10.1093/geront/gns109
Basso Lipani M, Holster K, Bussey S (2015) The preventable admissions care team (PACT): a social work-led model of transitional care. Soc Work Health Care. 54(9):810–827. https://doi.org/10.1080/00981389.2015.1084970
Naunton M, Peterson GM (2003) Evaluation of home-based follow-up of high-risk elderly patients discharged from hospital. J Pharm Pract Res 33(3):176–182
Holland R, Lenaghan E, Harvey I, Smith R, Shepstone L, Lipp A et al (2005) Does home based medication review keep older people out of hospital? The HOMER randomised controlled trial. BMJ 330(7486):293. https://doi.org/10.1136/bmj.38338.674583.AE
Galbraith AA, Meyers DJ, Ross-Degnan D, Burns ME, Vialle-Valentin CE, Larochelle MR et al (2017) Long-Term Impact of a Postdischarge Community Health Worker Intervention on Health Care Costs in a Safety-Net System. Health Serv Res 52(6):2061–2078. https://doi.org/10.1111/1475-6773.12790
Hendrix C, Tepfer S, Forest S, Ziegler K, Fox V, Stein J et al (2013) Transitional Care Partners: a hospital-to-home support for older adults and their caregivers. J Am Assoc Nurse Pract 25(8):407–414. https://doi.org/10.1111/j.1745-7599.2012.00803.x
Voss R, Gardner R, Baier R, Butterfield K, Lehrman S, Gravenstein S (2011) The care transitions intervention: translating from efficacy to effectiveness. Arch Intern Med 171(14):1232–1237. https://doi.org/10.1001/archinternmed.2011.278
Finn KM, Heffner R, Chang Y, Bazari H, Hunt D, Pickell K et al (2011) Improving the discharge process by embedding a discharge facilitator in a resident team. J Hosp Med 6(9):494–500. https://doi.org/10.1002/jhm.924
Forster AJ, Clark HD, Menard A, Dupuis N, Chernish R, Chandok N et al (2005) Effect of a nurse team coordinator on outcomes for hospitalized medicine patients. Am J Med 118(10):1148–1153. https://doi.org/10.1016/j.amjmed.2005.04.019
Wong FK, Ho MM, Yeung S, Tam SK, Chow SK (2011) Effects of a health-social partnership transitional program on hospital readmission: a randomized controlled trial. Soc Sci Med 73(7):960–969. https://doi.org/10.1016/j.socscimed.2011.06.036
Wong FKY, Chau J, So C, Tam SKF, McGhee S (2012) Cost-effectiveness of a health-social partnership transitional program for post-discharge medical patients. BMC Health Serv Res 12(479):1–8. https://doi.org/10.1186/1472-6963-12-479
Arbaje AI, Maron DD, Yu Q, Wendel VI, Tanner E, Boult C et al (2010) The geriatric floating interdisciplinary transition team. J Am Geriatr Soc 58(2):364–370. https://doi.org/10.1111/j.1532-5415.2009.02682.x
Coleman EA, Smith JD, Frank JC, Min SJ, Parry C, Kramer AM (2004) Preparing patients and caregivers to participate in care delivered across settings: the Care Transitions Intervention. J Am Geriatr Soc 52(11):1817–1825. https://doi.org/10.1111/j.1532-5415.2004.52504.x
Chow SK, Wong FK (2014) A randomized controlled trial of a nurse-led case management programme for hospital-discharged older adults with co-morbidities. J Adv Nurs 70(10):2257–2271. https://doi.org/10.1111/jan.12375
Bowles KH, Hanlon A, Holland D, Potashnik SL, Topaz M (2014) Impact of discharge planning decision support on time to readmission among older adult medical patients. Prof Case Manag 19(1):29–38. https://doi.org/10.1097/01.PCAMA.0000438971.79801.7a
Gurwitz JH, Field TS, Ogarek J, Tjia J, Cutrona SL, Harrold LR et al (2014) An electronic health record-based intervention to increase follow-up office visits and decrease rehospitalization in older adults. J Am Geriatr Soc 62(5):865–871. https://doi.org/10.1111/jgs.12798
Rice YB, Barnes CA, Rastogi R, Hillstrom TJ, Steinkeler CN (2016) Tackling 30-day, all-cause readmissions with a patient-centered transitional care bundle. Popul Health Manag 19(1):56–62. https://doi.org/10.1089/pop.2014.0163
Balaban RB, Weissman JS, Samuel PA, Woolhandler S (2008) Redefining and redesigning hospital discharge to enhance patient care: a randomized controlled study. J Gen Intern Med 23(8):1228–1233. https://doi.org/10.1007/s11606-008-0618-9
Ornstein K, Smith KL, Foer DH, Lopez-Cantor MT, Soriano T (2011) To the hospital and back home again: a nurse practitioner-based transitional care program for hospitalized homebound people. J Am Geriatr Soc 59(3):544–551. https://doi.org/10.1111/j.1532-5415.2010.03308.x
Young JB, Robinson M, Chell S, Sanderson D, Chaplin S, Burns E et al (2005) A whole system study of intermediate care services for older people. Age Ageing 34(6):577–583. https://doi.org/10.1093/ageing/afi179
Armstrong CD, Hogg WE, Lemelin J, Dahrouge S, Martin C, Viner GS et al (2008) Home-based intermediate care program vs hospitalization: cost comparison study. Can Fam Phys 54(1):66–73
Heppenstall CP, Chiang A, Hanger HC (2018) Readmissions to hospital in a frail older cohort receiving a community-based transitional care service. N Z Med J 131(1484):38–45
Sahota O, Pulikottil-Jacob R, Marshall F, Montgomery A, Tan W, Sach T et al (2017) The community in-reach rehabilitation and care transition (CIRACT) clinical and cost-effectiveness randomisation controlled trial in older people admitted to hospital as an acute medical emergency. Age Ageing 46(1):26–32. https://doi.org/10.1093/ageing/afw149
Courtney M, Edwards H, Chang A, Parker A, Finlayson K, Hamilton K (2009) Fewer emergency readmissions and better quality of life for older adults at risk of hospital readmission: a randomized controlled trial to determine the effectiveness of a 24-week exercise and telephone follow-up program. J Am Geriatr Soc 57(3):395–402. https://doi.org/10.1111/j.1532-5415.2009.02138.x
Courtney MD, Edwards HE, Chang AM, Parker AW, Finlayson K, Bradbury C et al (2012) Improved functional ability and independence in activities of daily living for older adults at high risk of hospital readmission: a randomized controlled trial. J Eval Clin Pract 18(1):128–134. https://doi.org/10.1111/j.1365-2753.2010.01547.x
Hawes EM, Smith JN, Pinelli NR, Adams R, Tong G, Weir S et al (2018) Accountable care in transitions (ACTion): a team-based approach to reducing hospital utilization in a patient-centered medical home. J Pharm Pract 31(2):175–182. https://doi.org/10.1177/0897190017707118
Low LL, Tan SY, Ng MJ, Tay WY, Ng LB, Balasubramaniam K et al (2017) Applying the integrated practice unit concept to a modified virtual ward model of care for patients at highest risk of readmission: a randomized controlled trial. PLoS ONE 12(1):e0168757. https://doi.org/10.1371/journal.pone.0168757
Morrison J, Palumbo MV, Rambur B (2016) reducing preventable hospitalizations with two models of transitional care. J Nurs Scholarsh 48(3):322–329. https://doi.org/10.1111/jnu.12210
Naylor MD, Hirschman KB, Hanlon AL, Bowles KH, Bradway C, McCauley KM et al (2014) Comparison of evidence-based interventions on outcomes of hospitalized, cognitively impaired older adults. J Comp Eff Res 3(3):245–257. https://doi.org/10.2217/cer.14.14
Naylor MD, Bowles KH, McCauley KM, Maccoy MC, Maislin G, Pauly MV et al (2013) High-value transitional care: translation of research into practice. J Eval Clin Pract 19(5):727–733. https://doi.org/10.1111/j.1365-2753.2011.01659.x
Parry C, Min SJ, Chugh A, Chalmers S, Coleman EA (2009) Further application of the care transitions intervention: results of a randomized controlled trial conducted in a fee-for-service setting. Home Health Care Serv Q 28(2–3):84–99. https://doi.org/10.1080/01621420903155924
Shah MN, Hollander MM, Jones CM, Caprio TV, Conwell Y, Cushman JT et al (2018) Improving the ED-to-home transition: the community paramedic-delivered care transitions intervention-preliminary findings. J Am Geriatr Soc 66(11):2213–2220. https://doi.org/10.1111/jgs.15475
Hernandez C, Aibar J, Seijas N, Puig I, Alonso A, Garcia-Aymerich J et al (2018) Implementation of home hospitalization and early discharge as an integrated care service: a ten years pragmatic assessment. Int J Integr Care 18(2):12. https://doi.org/10.5334/ijic.3431
Wee SL, Loke CK, Liang C, Ganesan G, Wong LM, Cheah J (2014) Effectiveness of a national transitional care program in reducing acute care use. J Am Geriatr Soc 62(4):747–753. https://doi.org/10.1111/jgs.12750
Harris R, Ashton T, Broad J, Connolly G, Richmond D (2005) The effectiveness, acceptability and costs of a hospital-at-home service compared with acute hospital care: a randomized controlled trial. J Health Serv Res Policy 10(3):158–166. https://doi.org/10.1258/1355819054338988
Mas MÀ, Santaeugènia SJ, Tarazona-Santabalbina FJ, Gámez S, Inzitari M (2018) Effectiveness of a hospital-at-home integrated care program as alternative resource for medical crises care in older adults with complex chronic conditions. J Am Med Dir Assoc 19(10):860–863. https://doi.org/10.1016/j.jamda.2018.06.013
Wilson A, Wynn A, Parker H (2002) Patient and carer satisfaction with ‘Hospital at Home’: quantitative and qualitative results from a randomised controlled trial. Br J Gen Pract 52(474):9–13
Lee KH, Low LL, Allen J, Barbier S, Ng LB, Ng MJ et al (2015) Transitional care for the highest risk patients: findings of a randomised control study. Int J Interg Care. https://doi.org/10.5334/ijic.2003
Carnahan JL, Slaven JE, Callahan CM, Tu W, Torke AM (2017) Transitions from skilled nursing facility to home: the relationship of early outpatient care to hospital readmission. J Am Med Dir Assoc 18(10):853–859. https://doi.org/10.1016/j.jamda.2017.05.007
Dahl U, Steinsbekk A, Johnsen R (2015) Effectiveness of an intermediate care hospital on readmissions, mortality, activities of daily living and use of health care services among hospitalized adults aged 60 years and older—a controlled observational study. BMC Health Serv Res. 15:351. https://doi.org/10.1186/s12913-015-1022-x
Goodwin JS, Li S, Middleton A, Ottenbacher K, Kuo YF (2018) Differences between skilled nursing facilities in risk of subsequent long-term care placement. J Am Geriatr Soc 66(10):1880–1886. https://doi.org/10.1111/jgs.15377
Herfjord JK, Heggestad T, Ersland H, Ranhoff AH (2014) Intermediate care in nursing home after hospital admission: a randomized controlled trial with one year follow-up. BMC Res Notes 9(7):889. https://doi.org/10.1186/1756-0500-7-889
Manville M, Klein M, Bainbridge L (2014) Improved outcomes for elderly patients who received care on a transitional care unit. Can Fam Phys 60(5):e263–e271
Blewett LA, Johnson K, McCarthy T, Lackner T, Brandt B (2010) Improving geriatric transitional care through inter-professional care teams. J Eval Clin Pract 16(1):57–63. https://doi.org/10.1111/j.1365-2753.2008.01114.x
Garåsen H, Windspoll R, Johnsen R (2008) Long-term patients' outcomes after intermediate care at a community hospital for elderly patients: 12-month follow-up of a randomized controlled trial. Scand J Public Health 36(2):197–204. https://doi.org/10.1177/1403494808089685
Garasen H, Windspoll R, Johnsen R (2007) Intermediate care at a community hospital as an alternative to prolonged general hospital care for elderly patients: a randomised controlled trial. BMC Public Health. 7:68. https://doi.org/10.1186/1471-2458-7-68
Young J, Green J (2010) Effects of delays in transfer on independence outcomes for older people requiring postacute care in community hospitals in England. J Clin Gerontol Geriatr 1(2):48–52. https://doi.org/10.1016/j.jcgg.2010.10.009
Rosen BT, Halbert RJ, Hart K, Diniz MA, Isonaka S, Black JT (2018) The enhanced care program: impact of a care transition program on 30-day hospital readmissions for patients discharged from an acute care facility to skilled nursing facilities. J Hosp Med. 13(4):229–236. https://doi.org/10.12788/jhm.2852
Berkowitz RE, Fang Z, Helfand BK, Jones RN, Schreiber R, Paasche-Orlow MK (2013) Project ReEngineered Discharge (RED) lowers hospital readmissions of patients discharged from a skilled nursing facility. J Am Med Dir Assoc 14(10):736–740. https://doi.org/10.1016/j.jamda.2013.03.004
Legrain S, Tubach F, Bonnet-Zamponi D, Lemaire A, Aquino JP, Paillaud E et al (2011) A new multimodal geriatric discharge-planning intervention to prevent emergency visits and rehospitalizations of older adults: the optimization of medication in AGEd multicenter randomized controlled trial. J Am Geriatr Soc 59(11):2017–2028. https://doi.org/10.1111/j.1532-5415.2011.03628.x
Donald F, Kilpatrick K, Reid K, Carter N, Bryant-Lukosius D, Martin-Misener R et al (2015) Hospital to community transitional care by nurse practitioners: a systematic review of cost-effectiveness. Int J Nurs Stud 52(1):436–451. https://doi.org/10.1016/j.ijnurstu.2014.07.011
Fabbre VD, Buffington AS, Altfeld SJ, Shier GE, Golden RL (2011) Social work and transitions of care: observations from an intervention for older adults. J Gerontol Soc Work. 54(6):615–626. https://doi.org/10.1080/01634372.2011.589100
Shepperd S, Iliffe S, Doll HA, Clarke MJ, Kalra L, Wilson AD et al (2016) Admission avoidance hospital at home. Cochrane Database Syst Rev. 9:CD007491. https://doi.org/10.1002/14651858.CD007491.pub2
Shepperd S, Doll H, Broad J, Gladman J, Iliffe S, Langhorne P et al (2009) Early discharge hospital at home. Cochrane Database Syst Rev 1:CD00356. https://doi.org/10.1002/14651858.CD000356.pub3
Goncalves-Bradley DC, Iliffe S, Doll HA, Broad J, Gladman J, Langhorne P et al (2017) Early discharge hospital at home. Cochrane Database Syst Rev. 6:CD000356. https://doi.org/10.1002/14651858.CD000356.pub4
Peel NM, Navanathan S, Hubbard RE (2014) Gait speed as a predictor of outcomes in post-acute transitional care for older people. Geriatr Gerontol Int 14(4):906–910. https://doi.org/10.1111/ggi.12191
Lithander FE, Neumann S, Tenison E, Lloyd K, Welsh TJ, Rodrigues JC, Higgins J, Scourfield L, Christensen H, Haunton VJ, Henderson EJ (2020) COVID-19 in older people: a rapid clinical review. Age Ageing 49(4):501–515. https://doi.org/10.1093/ageing/afaa093
O’Caoimh R, Kennelly S, Ahern E, O’Keeffe S, Ortuño RR (2020) COVID-19 and the challenges of frailty screening in older adults. J Frailty Aging. https://doi.org/10.14283/jfa.2020.30
Swiss Society Of Intensive Care Medicine (2020) Recommendations for the admission of patients with COVID-19 to intensive care and intermediate care units (ICUs and IMCUs). Swiss Medical Weekly 150:w20227. https://doi.org/10.4414/smw.2020.20227
Baillie L, Gallini A, Corser R, Elworthy G, Scotcher A, Barrand A (2014) Care transitions for frail, older people from acute hospital wards within an integrated healthcare system in England: a qualitative case study. Int J Integr Care 14(27):e009. https://doi.org/10.5334/ijic.1175
Allen J, Hutchinson AM, Brown R, Livingston PM (2018) User experience and care for older people transitioning from hospital to home: Patients' and carers' perspectives. Health Expect 21(2):518–527. https://doi.org/10.1111/hex.12646
Inzitari M, Gual N, Roig T, Colprim D, Pérez-Bocanegra C, San-José A et al (2015) Geriatric screening tools to select older adults susceptible for direct transfer from the emergency department to subacute intermediate-care hospitalization. J Am Med Dir Assoc 16(10):837–841. https://doi.org/10.1016/j.jamda.2015.04.009
Funding
This work was completed as part of the Joint Action on Frailty Prevention ‘grant number 724099/ADVANTAGE’, which has received funding from the European Union’s 3rd Health Programme (2014–2020).
Author information
Authors and Affiliations
Consortia
Contributions
Design and planning DS, AH, ROC, AMC. Screening of titles and abstracts: DS, AH, MOD, MOS, AMC, LLS, CAC, RRA. Data extraction: DS, AH, MOD, MOS, LLS. Data analysis: DS, AH. Drafting of manuscript: All. Proofreading and confirmation of final version of manuscript: All.
Corresponding author
Ethics declarations
Conflict of interest
On behalf of all authors, the corresponding author states that there is no conflict of interest.
Disclaimer
The content of this article represents the views of the authors only and is their sole responsibility; it cannot be considered to reflect the views of the European Commission and/or the Consumers, Health, Agriculture and Food Executive Agency or any other body of the European Union. The European Commission and the Agency do not accept any responsibility for use that may be made of the information it contains.
Ethics approval
Not applicable.
Consent to participate
Not applicable.
Consent for publication
Not applicable.
Code availability
Not applicable.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Sezgin, D., O’Caoimh, R., Liew, A. et al. The effectiveness of intermediate care including transitional care interventions on function, healthcare utilisation and costs: a scoping review. Eur Geriatr Med 11, 961–974 (2020). https://doi.org/10.1007/s41999-020-00365-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s41999-020-00365-4