Abstract
Schizophrenia is considered a serious mental disorder that affects over 21 million people worldwide, and is associated with disability that frequently affects the patient’s educational and working performance. In Argentina, two of the most widely used antipsychotics in the treatment of this disorder are haloperidol and risperidone. Both are provided free to patients without health coverage in public healthcare facilities. In this paper we seek to review the clinical and economic benefits of prescribing psychotropic therapies based on haloperidol (a first-generation antipsychotic that is part of the butyrophenone group of drugs) versus risperidone [an atypical or second-generation antipsychotic (neuroleptic) drug] in adult patients who have been diagnosed with schizophrenia. To achieve this objective, an exhaustive search of relevant articles published between 2006 and April 2017 was conducted. This literature search showed that intermittent treatment usually fails to prevent relapses due to irregular protection, therefore continuous treatment is more effective. Although the injectable formats of both drugs [haloperidol depot and long-acting injectable risperidone (LAIR)] have not proven to have significant differences with regard to clinical effectiveness vis-à-vis the tablet formats, they showed a lower cost-effectiveness ratio by reducing patients’ relapses. Moreover, LAIR exhibits superior cost effectiveness compared with haloperidol depot. Haloperidol is less expensive than risperidone but is less cost effective; in comparison with haloperidol, treatment with risperidone produces (1) an improvement in quality-adjusted life-years, and (2) a significant reduction in negative symptoms. In most cases, antipsychotic treatments are effective in controlling the positive and negative symptoms associated with schizophrenia, allowing patients to live in their communities without any impairments. However, it is extremely important to combine pharmacological treatment with other measures that constitute psychosocial therapy.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Schizophrenia is a very expensive disorder. Psychotropic drug expenses and repeated hospitalizations due to relapses involve the biggest costs. |
Intermittent antipsychotic therapy is not cost effective because of the higher incidence of relapses. |
Depot versions of haloperidol and risperidone are preferable to oral intake versions since they facilitate the compliance of treatment by patients, reducing the odds of relapse. |
Although risperidone is more expensive, it exhibits a lower cost-effectiveness ratio than haloperidol, and fewer side effects. |
1 Introduction
Schizophrenia is defined as a mental illness that involves positive symptoms associated with excesses (alterations in thoughts or delirium, alterations in perception or hallucinations, alterations in behavior, incoherence, illogicality, distractibility, tachylalia, etc.) and negative symptoms related to deficiencies (lack of energy and motivation, emotional disorders, social withdrawal, immutable facial expression, low visual contact, absence or deficiency of vowel expressions when speaking, etc.).
People with schizophrenia have a life expectancy 15–30 years shorter than the general population. Approximately 2 million new cases are recorded each year worldwide, and prevalence rates do not show significant quantitative differences between ethnic groups and geographical regions. At least two-thirds of patients need to be hospitalized once in their lives because of this disease [1].
Schizophrenia is an extremely expensive disorder; psychotropic drug expenses involve the biggest costs, along with relapses and repeated hospitalization due to patients’ lack of commitment to treatments [2]. Loss of autonomy and reduced labor productivity that come with having schizophrenia do not only affect patients but also their families, either through the need to deliver personal care services to patients or their own health deterioration as a result of these duties. Caring activities usually involve a group of quite heterogeneous actions aimed mainly at covering the patients’ lack of autonomy that comes with this disorder [3].
According to clinical practice guides from the National Institute for Health and Care Excellence (NICE) [4], schizophrenia treatment must complement antipsychotic medication, along with therapeutic counseling. The treatment of schizophrenia with antipsychotic medication may require a multidimensional approach that should take into account the efficacy (the ability of an intervention to get the desired result under ideal conditions), effectiveness (the degree to which the intended effect is obtained under routine clinical practice conditions or settings) and efficiency (value of the intervention as relative to its cost to the individual or society) [5]. Selection of the best drug available must be made by the professional alongside the patient, taking into account the results of an integral medical check-up. The WHO Model List of Essential Medicines details four injectable antipsychotics for the treatment of schizophrenia and considers them part of the minimum set of medicines necessary for basic healthcare and as the most cost effective and safe medicines for this purpose: chlorpromazine, fluphenazine, haloperidol and risperidone [6].Footnote 1
In Argentina, approximately 400,000 people have schizophrenia [1], with adults and adolescents of low socioeconomic status (SES) showing an increased risk of developing this type of disorder [7]. In this country, haloperidol and risperidone are the two most widely used antipsychotics in the treatment of schizophrenia disorder [8]. Both are provided free to patients without health coverage in public healthcare facilities, although the population receiving risperidone is 10% higher than the population receiving haloperidol [9]. This situation raises the question as to whether there is evidence of clinical and economic benefits supporting the prescription of one drug over the other.
2 Objectives
The general objective of this paper consisted of reviewing the clinical and economic benefits of psychotropic therapies based on haloperidol and risperidone administered to adult patients who have been diagnosed with schizophrenia following Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-5)Footnote 2 guidelines. Specific objectives include:
-
(a)
identifying the most commonly prescribed drugs for the treatment of each stage of schizophrenia disorder in Argentina;
-
(b)
inquiring about the relative advantages of different psychotropic administration therapies, particularly between (1) continuous versus intermittent treatment (of the psychotic episode), and (2) long-acting injectable versions versus oral versions of daily intake;
-
(c)
analyzing the results of cost effectiveness and clinical studies performed in relation to haloperidol and risperidone, particularly those comparing both drugs.
3 Methodology
To accomplish the first objective, an interview with key informants of the Argentinean public health sector was performed, including three psychiatrists, two psychologists, one nurse, one toxicology biochemist, one pharmacist, and two general practitioners. We also reviewed the clinical guidelines proposed by the Argentinean Ministry of Health.
For objectives two and three, a comprehensive search of the Google Scholar and Cochrane electronic databases for peer-reviewed articles published in English was conducted in the last week of September 2016 and updated in April 2017. Search terms were ‘schizophrenia’, ‘schizophrenic disorders’, ‘pharmacoeconomic analysis’, ‘drug economic evaluation’, ‘haloperidol’, ‘risperidone’, ‘drug therapy’, and ‘pharmacotherapy’. In addition, a hand search of the reference lists of published articles was also conducted. Only scientific papers published from 2006 until the present were considered, so as to be able to use updated sources. Using this procedure, we identified 118 potentially relevant scientific articles. First, we excluded studies in which patients presented with any other pathology, such as hypothyroidism, cardiac or pulmonary conditions, hypocalcemia, cancer, Parkinson’s disease, epilepsy, diabetes, and liver or kidney failure, etc. Studies that included pregnant patients or patients with drinking or smoking problems were also excluded. Finally, we excluded articles that evaluated the clinical and economic benefits of haloperidol and risperidone therapies for diseases other than schizophrenia (e.g. delirium).
The remaining articles were assessed for their suitability, assigning each a relevance rating (from 0 to 10), taking into account both the methodological quality and degree of response to each of the questions posed in the present review. In order to define the scoring, the quality guide for economic studies developed by NICE [4] was used. Those items that had a relevance score < 5 were excluded. After this assessment, 24 scientific papers were included in the study.
4 Results
4.1 Objective 1
Schizophrenia is a mental disorder that has three phases. The acute phase or crisis is characterized by a psychotic outbreak that is an abrupt manifestation of the positive symptomatology of schizophrenia for a short period of time and involves a temporary rupture of reality; patients under this state have hallucinations or delirium with their consequent decompensation. When a psychotic outbreak occurs, the patient should be hospitalized.
All key informants agreed that, in Argentina, the combined use of haloperidol and lorazepam is the most common indication for emergency care in the acute phase of this disease, in the absence of a previous medication regimen. Haloperidol has an excellent acute antipsychotic profile but is not very sedative, therefore it should be accompanied by an anxiolytic and hypnotic, such as lorazepam [10]. It is recommended to provide 2–10 mg of haloperidol orally or intramuscularly, together with 2 mg of lorazepam orally or intramuscularly every 60 min (or 30 min, if necessary) until stabilization of, and decreased agitation in, the patient [11].
The stabilization or post-crisis phase covers the 6 months (up to 12 months) after the acute episode, where the patient’s functionality improves. In this phase, it is recommended the antipsychotic medication be maintained. Continuous psychosocial care should also be provided. In Argentina, this instance is not contemplated, therefore patients move directly from the acute to the maintenance phase.
Finally, the stable or maintenance phase is where patients may not present symptoms, or present symptoms such as tension, irritability, depression, negative symptoms, and cognitive impairment. Positive symptoms (hallucinations, delusions, behavioral disturbances) of the acute phase may persist in some patients, but to a lesser extent [12]. During this phase, the main objectives are promoting the social and work re-integration of the patient and minimizing the risk of relapses, without the drug causing severe adverse effects that alter the patients’ quality of life. In that sense, a maintenance dose can be used (reaching 20% of the effective dose through a slow and gradual decrease) [13]. In Argentina, patients who go through this phase are mainly treated with risperidone or, to a lesser extent, haloperidol. Both drugs are used to treat positive and negative symptoms, and have a similar active substance.
4.2 Objective 2
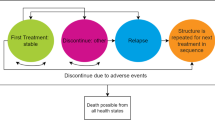
Some professionals consider that intermittent pharmacological treatment, which refers to the use of medication during periods close to relapse of the symptoms of schizophrenia, has superior efficacy with respect to the continuous administration of psychoactive drugs [14]. Intermittent pharmacological treatment includes intervention based on prodrome (which evaluates the risk of the initial stage of relapse), and intervention in times of crisis during an acute episode or deterioration of mental health and the gradual increase of periods without drugs. The objective is to reduce exposure to drugs and reduce side effects [15]. However, Sampson et al. [16] showed that (1) intermittent antipsychotic treatment is not as effective as continuous treatment, and (2) although costs are reduced for patients (and third-party payers) when they do not consume drugs on a daily basis, they are increased by the higher rates of hospitalization experienced by these individuals.
Continuous treatment for schizophrenia disorder can be administered orally (by taking daily tablets) or by injections (with applications approximately every 15 days). Treatment with long-acting injections has demonstrated a reduction in hospital admissions and patient relapses, and, despite being more expensive than oral treatments, a better cost-effectiveness ratio [17].
The final result of treatment is affected by the patient’s cultural and social surroundings, education level, personality traits, and age. Some patients do not comply with treatment due to the belief that they have not been treated or diagnosed accurately or that the drugs they are taking are not effective, or because they do not fully understand the explanations given by their doctor [18]. At other times, the cause of the ineffectiveness of treatment lies in simple forgetfulness or having difficulty obtaining the medication they need [19]. As a result of the abovementioned reasons, the best way to avoid all problems related to keeping up with treatment is to use injectable long-acting medication in order to circumvent all the hassle that comes with the daily taking of oral tablets for schizophrenic patients [20].
4.3 Objective 3
According to the Vademecum (2016), haloperidol is a classic or first-generation antipsychotic drug (AT) that is part of the butyrophenone group of drugs. It was one of the first antipsychotics used in the 20th century for the treatment of mental illnesses, and can be administered orally through an intramuscular injection or intravenous line. This psychotropic agent is a potent antagonist of cerebral dopaminergic receptors and is therefore included among the high-potency neuroleptics. Haloperidol features neither antihistamine nor anticholinergic activity. On the other hand, risperidone belongs to the group of atypical or second-generation (AA) antipsychotics (neuroleptics), which show a similar clinical effectiveness in comparison to first-generation antipsychotics. The mechanism of action of risperidone is unknown, but it is thought that its activity takes place due to combined blocking of the dopaminergic receptors D2 and the serotonergic receptors S2 (dopaminergic-serotonergic antagonist). Other effects that risperidone produces might be explained by the blocking of adrenergic-histaminergic α2 receptors. This psychotropic is well-absorbed by the gastrointestinal mucous membrane and is also fully metabolized by the liver.
Every antipsychotic has a common mechanism of action—the antidopaminergic effect.Footnote 3 First-generation antipsychotics are the oldest and their action is mainly antidopaminergic, while second-generation psychotropics are characterized by simultaneously blocking the dopaminergic and serotonergic receptors.Footnote 4
Long-acting injections of first-generation antipsychotics were the first to be developed, particularly those of haloperidol. Haloperidol depot (injectable version) has not shown any significant differences regarding medical effectiveness, side effects, and behavioral responses in relation to haloperidol in tablets [21]. Dold et al. [22] have demonstrated that, in comparison with other first-generation, high-potency antipsychotics,Footnote 5 haloperidol produces fewer side effects and reduces the positive symptoms of the disease more effectively. Nevertheless, studies performed to date do not show haloperidol’s superiority in comparison with low-potency antipsychotics [23].
Haloperidol is usually prescribed alongside benzodiazepines (such as diazepam, lorazepam, clonazepam, etc.) since these drugs have a sedative effect on patients that increases the neuroleptic sedative action of haloperidol. However, treatment carried out with only benzodiazepines is neither effective nor safe for patients [24].
In comparison with other typical antipsychotics such as chlorpromazine, haloperidol has produced not only better results in terms of patient adherence to treatment but also a higher incidence rate of movement disorders, as a result of their continued use [25].
Risperidone was the first second-generation antipsychotic available in long-acting formulations [26]. The long-acting injectable risperidone (LAIR) presents, in general, the same effectiveness as risperidone in tablet formulations. In a pairwise comparison between depot injections of risperidone and their equivalent oral formulations, Tiihonen et al. [27] found that the risk of rehospitalization for patients receiving depot medications was approximately one-third of that for patients receiving oral medications. In addition, a study by Barnett et al. [28] reported that 45% of patients in the oral treatment group and 39% of patients in the LAIR group were hospitalized. Although the LAIR contributes to reducing treatment dropout, it is much more expensive [29].
Nielsen et al. [30] conducted a retrospective inception cohort study of adults with schizophrenia using nationwide Danish registers from 1995 to 2009, and comparing outcomes between patients receiving first-generation antipsychotic long-acting injections (FGA-LAIs) or long-acting risperidone injections. Among 4532 patients who initiated treatment with long-acting injectables, 2078 received LAIR and 2454 received FGA-LAIs (zuclopenthixol decanoate = 52.2%, perphenazine decanoate = 37.2%, haloperidol decanoate = 5.0%, flupenthixol decanoate = 4.4%, fluphenazine decanoate = 1.3%). LAIR was not superior to FGA-LAIs in regard to time to psychiatric hospitalization, all-cause discontinuation, and duration of hospitalization.
After carrying out a study of 77 patients diagnosed with schizophrenia who belonged to the Early Intervention Program on Psychosis of the Mental Health Institute of Singapore, Chee et al. [31] concluded that risperidone effectively reduces most of the negative symptoms of this disorder compared with haloperidol, as well as being better tolerated by patients. Tamrakar et al. [32] discovered that after 1 week of treatment, patients who were treated with risperidone did much better than those who were taking haloperidol, in terms of (1) total Positive and Negative Syndrome Scale (PANSS) score, (2) Negative Symptoms Scale, and (3) General Psychopathology Scale.
Ahmed et al. [33] performed a review aimed at comparing the efficacy of haloperidol versus risperidone, and concluded that in schizophrenic patients, both drugs showed similar performance, although, compared with haloperidol, risperidone exhibited slightly higher efficacy and a lower incidence of extrapyramidal symptoms (EPSs).Footnote 6
According to Escamilla [34], individuals who have been affected by schizophrenia disorder for more than 1 year frequently develop some kind of affective disorder, such as mania or depression. In such cases, pharmacological treatment poses a real challenge since it is not recommended to administer antidepressants to a patient who is already receiving antipsychotics [35]. Second-generation antipsychotics (such as risperidone) have been shown to be more effective when treating these types patients, compared with first-generation antipsychotics (such as haloperidol) [36].
A Belgian cost-effectiveness analysis conducted by De Graeve et al. [37] found that long-acting risperidone is more effective and less costly than depot haloperidol. LAIR appears to represent a favorable first-line strategy for patients with schizophrenia requiring long-term maintenance treatment. A study performed in Taiwan by Yang et al. [38] using the Kaplan–Meier method also showed that LAIR is more cost effective than haloperidol administered via depot intramuscular injections. On the other hand, a scientific study performed in Sweden by Hensen et al. [39] found that treatment with LAIR produces an improvement in quality-adjusted life-years (QALYs), alongside long-term savings in relation to haloperidol depot. Together with olanzapine, risperidone is one of the most used second-generation antipsychotics in the UK, and has proven to be the most cost effective; it is expected that this tendency will become worldwide in the following years [40]. In most countries, atypical long-acting (especially risperidone)/extended-release antipsychotic medication is likely to be a cost-effective, first-line strategy for managing schizophrenia
5 Discussion
The four main objectives of schizophrenia treatment are controlling symptoms, reducing the frequency and severity of psychotic episodes, improving quality of life, and facilitating the socio-labor and family integration of the schizophrenic patient. Early diagnosis and adherence to treatment are key elements to improving the prognosis of patients with schizophrenia. The challenge faced by health practitioners is the creation of an empathic therapeutic relationship with the patient and his/her family. Once created, an individualized therapeutic plan taking into account biological, psychological, familiar and social aspects should be developed [41].
Although in this review the usual distinction between first- (e.g. haloperidol) and second-generation antipsychotics (e.g. risperidone) is adopted, some studies suggest that this straightforward classification could be misleading. Antipsychotics do not form homogeneous classes, showing significant differences in terms of efficacy, side effects, cost, and pharmacology [42]. Thus, neither first- nor second-generation antipsychotics could be considered to consistently outperform its counterpart [43]. Leucht et al. [44] proposed an alternative criterion based on the development of hierarchies of drugs in terms of seven outcomes: efficacy, all-cause discontinuation, weight gain, extrapyramidal side effects, prolactin increase, QTc prolongation, and sedation. The information provided by these hierarchies could help clinicians to adapt the choice of antipsychotic drug to the needs of individual patients.
Although in most cases antipsychotic treatments have allowed patients with schizophrenia to live in their communities without any impairments, it is extremely important to combine pharmacological treatment with other types of care that constitute psychosocial therapy, which requires assistance mechanisms such as counseling services, occupational workshops, day centers, and self-help groups [45].
In 2010, Argentina passed the National Law of Mental Health (Law 26,657), which promotes the social insertion of patients with mental health disorders. The law established the closure of specialized mental hospitals by the year 2020, and the integration of mental healthcare in general hospitals. The law also contemplated the creation of assistance mechanisms to provide the specific therapies required by patients with mental health disorders, but 7 years after its approval, more than half of the mental health budget has been spent in specialized mental hospitals, and, in some regions of Argentina, assistance mechanisms do not exist or are scarce in relation to their need [46].
Schizophrenic patients in Argentina are guaranteed access to pharmacological treatment irrespective of his/her SES; however, psychosocial therapy is not assured in most cases. This calls for a coordinated effort of all involved (patients, families, healthcare staff, healthcare institutions, health insurance organizations, and the government) to revert this situation.
6 Conclusions
In Argentina, the most usual indication for emergency care in the acute phase of schizophrenia is the combined use of haloperidol and lorazepam. Meanwhile, during the maintenance phase, patients are treated with risperidone or, in a lesser proportion, haloperidol.
Intermittent treatment often fails to prevent relapses due to irregular protection. This is why continuous treatment is more effective and, in particular, the injectable modality is the most recommended since it facilitates the compliance of treatment by the patient in a simple way and with little interference in the patient’s life, reducing the discomfort of treatment with daily oral tablets.
Based on the revision carried out, we can conclude that (1) risperidone features fewer side effects than haloperidol; (2) treatment with risperidone produces an improvement in QALYs; (3) risperidone significantly reduces negative symptoms in relation to haloperidol; (4) LAIR is more effective in the treatment of patients with schizophrenia who later develop depression or mania; (5) LAIR is not superior to haloperidol in regard to time to psychiatric hospitalization, all-cause discontinuation, and duration of hospitalization; and (6) haloperidol is less expensive than risperidone, but is less cost effective.
Data Availability Statement
Data sharing was not applicable to this article as no datasets were generated or analyzed during the current study.
Notes
The WHO Model List of Essential Medicines has been updated every 2 years since 1977. The current versions are the 19th WHO Essential Medicines List and the 5th WHO Essential Medicines List for Children, updated in April 2015.
The DSM, edited by the American Psychiatry Association, develops a classification of mental disorders that provides clear descriptions of the diagnostic categories, so as to allow physicians and health researchers to diagnose, study and exchange information and treat different mental disorders. The last updated version is the 5th edition, known as DSM-5, which was published on 18 May 2013.
The positive symptoms of schizophrenia disorder are related to the mesolimbic pathway, which is overactive (too much dopamine), and the negative effects are related to the mesocortical pathway, which is underactive (too little dopamine). The same neurotransmitter (dopamine) affects part of the nervous system by excess, and others by default, whereby antipsychotics perform the dopaminergic blocking function.
It is currently believed that the dopamine hypothesis is excessively simplistic, which has resulted in some researchers posing the serotonergic hypothesis of schizophrenia disorder, in which it is presumed that this neurotransmitter also plays an important role in this disorder.
Traditional antipsychotics (first-generation) are classified into two groups, high potency and low potency, depending on the amount of necessary doses in order to achieve a certain result.
EPSs are side effects of antipsychotic medication, and can cause involuntary movement and muscle control problems over the entire body.
References
WHO. Schizophrenia: fact sheet N°397. Media Centre. 2016. https://goo.gl/g0ARGP.
Leucht S, Tardy M, Komossa K, Heres S, Kissling W, Davis JM. Maintenance treatment with antipsychotic drugs for schizophrenia. Cochrane Database Syst Rev. 2012;5:008016.
Oliva-Moreno J, González A, Aranda I, Hidalgo A, Vilaplana C. Cuidados informales asociados a la limitación de la autonomía en personas con esquizofrenia. En: Bobes J, Saiz J, editors. Impacto social de la esquizofrenia, vol. 1, no. 1. Barcelona: Glosa. pp. 105–29.
National Institute for Clinical Excellence. Methods for the development of NICE public health guidance. London: NICE; 2006.
Crespo-Facorro B, Bernardo M, Argimon JM, Arrojo M, Bravo-Ortiz MF, Cabrera-Cifuentes A, et al. Eficacia, eficiencia y efectividad en el tratamiento multidimensional de la esquizofrenia: proyecto Rethinking. Revista de Psiquiatría y Salud Mental. 2017;10(1):4–20.
World Health Organization. WHO model list of essential medicines: 18th list. April 2013. https://goo.gl/Ekj8yc.
Ortiz-Hernández L, López-Moreno S, Borges G. Desigualdad socioeconómica y salud mental: revisión de la literatura latinoamericana. Cadernos de saúde pública. 2007;23(6):1255–72.
Leiderman EA, Lorenzo L. Prescription patterns in the treatment of schizophrenia [in Spanish]. Vertex (Buenos Aires, Argentina). 2015;26(119):11–6.
Ministerio de Salud de la Nación (MSN). Primer Registro Centralizado de patologías cognitivas en Argentina (ReDeCAr). 2011. https://goo.gl/5r6Hoy.
Cornejo-León F, Dragotto M, Ramos G, Klein R, Vernimmen P, Corral RM. Tratamiento farmacológico en pacientes con esquizofrenia. Alcmeon. 2006;13(3):20–9.
Ministerio de Salud de la Nación (MSN), Lineamientos para la atención de la urgencia en Salud Mental. Red de servicios de Salud Mental con base en la comunidad. 2013. https://goo.gl/77ttzk.
Agència d’Avaluació de Tecnologia i Recerca Mèdiques de Cataluña (AATRMC). Guía de Práctica Clínica sobre la Esquizofrenia y el Trastorno Psicótico Incipiente. GuiaSalud. 2009. https://goo.gl/9NjZuO.
Alvano SA. Pautas de tratamiento y manejo clínico. ALCMEON Revista Argentina de Clínica Neuropsiquiátrica. 2000;9:361–6.
Schooler NR. Maintenance medication for schizophrenia: strategies for dose reduction. Focus. 2004;2(1):175–86. doi:10.1176/foc.2.1.175.
Brissos S, Veguilla MR, Taylor D, Balanzá-Martinez V. The role of long-acting injectable antipsychotics in schizophrenia: a critical appraisal. Ther Adv Psychopharmacol. 2014;4(5):198–219.
Sampson S, Joshi K, Mansour M, Adams CE. Intermittent drug techniques for schizophrenia. Schizophr Bull. 2013;39(5):960–1.
Olivares JM, Rodriguez-Martinez A, Burón JA, Alonso-Escolano D, Rodriguez-Morales A. Cost-effectiveness analysis of switching antipsychotic medication to long-acting injectable risperidone in patients with schizophrenia. Appl Health Econ Health Policy. 2008;6(1):41–53.
Alarcón RD. Culture, cultural factors and psychiatric diagnosis: review and projections. World Psychiatry. 2009;8(3):131–9.
Jin J, Sklar GE, Oh VMS, Li SC. Factors affecting therapeutic compliance: a review from the patient’s perspective. Ther Clin Risk Manag. 2008;4(1):269.
Kirson NY, Weiden PJ, Yermakov S, Huang W, Samuelson T, Offord SJ, Wong SJ. Efficacy and effectiveness of depot versus oral antipsychotics in schizophrenia: synthesizing results across different research designs. J Clin Psychiatry. 2013;74(6):568–75.
Quraishi SN, David A, Brasil MA, Alheira FV. Depot haloperidol decanoate for schizophrenia. Cochrane Database Syst Rev. 2011;(1):24–40.
Dold M, Samara MT, Li C, Tardy M, Leucht S. Haloperidol versus first-generation antipsychotics for the treatment of schizophrenia and other psychotic disorders. Cochrane Database Syst Rev. 2015;(1):152–77.
Tardy M, Huhn M, Kissling W, Engel RR, Leucht S. Haloperidol versus low-potency first-generation antipsychotic drugs for schizophrenia. Cochrane Database Syst Rev. 2014;(7):CD009268.
Dold M, Li C, Tardy M, Khorsand V, Gillies D, Leucht S. Benzodiazepines for schizophrenia. Cochrane Database Syst Rev. 2012;(11):95–116.
Leucht C, Kitzmantel M, Kane J, Leucht S, Chua WLLC. Haloperidol versus chlorpromazine for schizophrenia. The Cochrane Library. 2008. https://goo.gl/mIqm72.
Chue P, Chue J. The cost–effectiveness of risperidone long-acting injection in the treatment of schizophrenia. Expert Rev Pharmacoecon Outcomes Res. 2012;12(3):259–69.
Tiihonen J, Haukka J, Taylor M, Haddad PM, Patel MX, Korhonen P. A nationwide cohort study of oral and depot antipsychotics after first hospitalization for schizophrenia. Am J Psychiatry. 2011;168(6):603–9.
Barnett PG, Scott JY, Krystal JH, Rosenheck RA. Cost and cost-effectiveness in a randomized trial of long-acting risperidone for schizophrenia. J Clin Psychiatry. 2012;73(5):696–702.
Sampson S, Hosalli P, Furtado VA, Davis JM. Risperidone (depot) for schizophrenia. The Cochrane Library. Cochrane Database Syst Rev. 2016;(4):89–120.
Nielsen J, Jensen SO, Friis RB, Valentin JB, Correll CU. Comparative effectiveness of risperidone long-acting injectable vs first-generation antipsychotic long-acting injectables in schizophrenia: results from a nationwide, retrospective inception cohort study. Schizophr Bull. 2015;41(3):627–36.
Chee AWS, Abidin EB, Verma SK. Short term effectiveness of haloperidol versus risperidone in first-episode schizophrenia. Proc Singapore Healthc. 2016;25(2):72–9.
Tamrakar SM, Nepal MK, Koirala NR, Sharma VD, Gurung CK, Adhikari SR. An open, randomized, comparative study of efficacy and safety of risperidone and haloperidol in schizophrenia. Kathmandu Univ Med J. 2006;4(2):152–60.
Ahmed SP, Siddiq AFSHAN, Baig SG, Khan RA. Comparative efficacy of haloperidol and risperidone: a review. Pak J Pharmacol. 2007;24(2):55–64.
Escamilla MA. Diagnosis and treatment of mood disorders that co-occur with schizophrenia. Psychiatr Serv. 2001;52:911–9.
Emsley RA, Jones AM. Treatment of depressive symptoms in partially refractory schizophrenia: efficacy of quetiapine versus haloperidol. Eur Neuropsychopharmacol. 2001;11:S264–5.
Furtado VA, Srihari V, Kumar A. Atypical antipsychotics for people with both schizophrenia and depression. The Cochrane Library. 2008. https://goo.gl/gqkVIv.
De Graeve D, Smet A, Mehnert A, Caleo S, Miadi-Fargier H, Mosqueda GJ, et al. Long-acting risperidone compared with oral olanzapine and haloperidol depot in schizophrenia: a Belgian cost-effectiveness analysis. Pharmacoeconomics. 2005;23(1):35–47.
Yang YK, Tarn YH, Wang TY, Liu CY, Laio YC, Chou YH, et al. Pharmacoeconomic evaluation of schizophrenia in Taiwan: model comparison of long-acting risperidone versus olanzapine versus depot haloperidol based on estimated costs. Psychiatry Clin Neurosci. 2005;59(4):385–94.
Hensen M, Heeg B, Löthgren M, van Hout B. Cost effectiveness of long-acting risperidone in Sweden. Appl Health Econ Health Policy. 2010;8(5):327–41.
Jayaram MB, Hosalli P, Stroup TS. Risperidone versus olanzapine for schizophrenia. Cochrane Database Syst Rev. 2006;(2):50–99.
Byrne P. Managing the acute psychotic episode. BMJ Br Med J. 2007;334(7595):686.
Leucht S, Corves C, Arbter D, Engel RR, Li C, Davis JM. Second-generation versus first-generation antipsychotic drugs for schizophrenia: a meta-analysis. Lancet. 2009;373(9657):31–41.
Parks J, Radke A, Parker G, Foti ME, Eilers R, Diamond M, Svendsen D, Tandon R. Principles of antipsychotic prescribing for policy makers, circa 2008. Translating knowledge to promote individualized treatment. Schizophr Bull. 2008;35(5):931–6.
Leucht S, Cipriani A, Spineli L, Mavridis D, Örey D, Richter F, Samara M, Barbui C, Engel R, Geddes JR, Kissling W, Paul Stapf M, Lässig B, Salanti G, Davis J. Comparative efficacy and tolerability of 15 antipsychotic drugs in schizophrenia: a multiple-treatments meta-analysis. Lancet. 2013;382(9896):951–62.
National Collaborating Centre for Mental Health UK. Psychosis and schizophrenia in adults. London: National Collaborating Centre for Mental Health; 2014.
Tisera A, Léale H, Lohigorry J, Pekarek AL, Joskowicz A. Salud Mental y desinstitucionalización: resistencias y obstáculos en los procesos de externación en un hospital monovalente de la zona sur de la Ciudad de Buenos Aires. Anuario de investigaciones. 2013;20(1):251–8.
Author information
Authors and Affiliations
Contributions
All authors made substantial contributions to the conception and design of this research, acquisition of data, and analysis and interpretation of data. They also participated in drafting the article and revising it critically for important intellectual content, as well as providing final approval of the version to be submitted.
Corresponding author
Ethics declarations
Funding
No funding was received.
Conflict of interest
Fernando Pablo Lago, Gisela Paula González and Nebel Silvana Moscoso declare no conflicts of interest.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution-NonCommercial 4.0 International License (http://creativecommons.org/licenses/by-nc/4.0/), which permits any noncommercial use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
About this article
Cite this article
González, G.P., Moscoso, N.S. & Lago, F.P. A Review of Clinical and Economic Evaluations Applied to Psychotropic Therapies Used in the Treatment of Schizophrenia in Argentina. PharmacoEconomics Open 2, 233–239 (2018). https://doi.org/10.1007/s41669-017-0058-8
Published:
Issue Date:
DOI: https://doi.org/10.1007/s41669-017-0058-8