Abstract
Objectives
To provide an overview of the current literature regarding the neurobiological treatments of psychopharmacology, neuromodulation, oxytocin therapy, and psychological resilience, as treatments for autism-related difficulties, and to distil the research findings from those treatments for everyday clinical application.
Methods
Instead of producing another specific systematic summary of the efficacy of these treatments, this review took an overview of each field of research, identified its key research findings, and evaluated the treatment-ready status of each of them in terms of their evidence base. From this information, a set of recommendations were derived for their clinical applications, so as to inform practice in the field.
Results
These treatments represent relatively recent and neurobiologically based approaches to the challenges of autism, and are in the development stage. Each treatment is promising, and has some evidential basis for its success, but all need further research to establish their evidence-based validity for everyday clinical usage.
Conclusions
While most of these treatments can be applied with caution, clinicians should acknowledge their restrictive benefits and costs, that are described herein. Within those caveats, each of these treatments should be considered as an emerging therapy that clinicians should consider utilising in appropriate settings and with specific cases.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Increased awareness of variations in autism symptom profiles and daily functioning has led to a consideration of the bases on which individual differences in autistic characteristics might be established, including neurological, behavioural, and biological factors (Nordahl et al., 2022). With this trend to consider autism beyond the traditional diagnostic features (APA, 2022), further focus has been applied to greater breadth of therapy/intervention modalities beyond psychosocial, educational, and behavioural approaches. Some of these treatment approaches have included attempts to directly alter various aspects of neurobiological functioning.
These neurobiological treatment models represent a new and promising approach to the challenges faced by autistic people, and cover a wide range of treatments, including a focus on the role of mitochondria in autism (Frye, 2020; Frye et al., 2021), adjustment of the gut microbiome (Taniya et al., 2022), dietary folate (Rossignol & Frye, 2021), and even stem cells (Riordan et al., 2019). Some of these are still in their infancy, but three treatment approaches that have received a good deal of research attention and which hold promise for clinical settings are psychopharmacology, neuromodulation, and the use of oxytocin. Each of these will be described and discussed below, not to provide exhaustive reviews of the research underpinning them, but rather to draw the key findings from that research, and thence distil the major implications for clinicians who work with autistic people.
Method
Each of the two authors blindly searched PubMed, Psych Info, and Google Scholar for the last 23 years (2000 onwards) in March–May, 2023, using the descriptors, “autism” and “psychopharmacology” and “neuromodulation” and “oxytocin”. Reference lists from all papers were also searched by hand, with the overall aim of identifying those key papers which provided overviews of the respective treatments, or were valuable examples of how research was conducted in that field. From the papers identified, a common list was compiled that each author endorsed. Unlike a systematic review or meta-analysis, the major aim was not to provide an exhaustive list of papers and their content in an historical model, but rather to glean a maximumly informative overview for clinicians and professionals in the field. On that basis, the preference was to select the most recent papers for comprehensiveness of information. All of these papers are cross-referenced in the review presented below, with details shown in the reference list.
Because this was not a systematic review as defined by PRISMA, but rather aimed at providing an overview of the field as it related to clinical practice, only those PRISMA items that were relevant were followed, including Introduction (PRISMA items 3, 4) and Methods (PRISMA items 5–8). Inclusion criteria were that all major empirical and review papers on these topics identified from the search process described above were included if both of the authors independently judged that the paper made a contribution rated at least 7/10 on 10-point scale where 10 = vital to the field and informative to clinicians. Using these papers, PRISMA items 23a to 23d (Discussion) were followed to provide a general interpretation of the results in the context of other evidence, describe limitations of the evidence reviewed, and discuss the implications of the research findings for clinical practice.
Psychopharmacological Treatments
Currently, there are no approved psychopharmacological treatments that have been developed to target the core features of autism (i.e., impaired social communication and social interaction, plus presence of restricted and repetitive behaviour patterns) (Boksha et al., 2023). Vorstman et al. (2017) and Chawner et al. (2021) argued that incapacity to address autism impairment arises from the fact that current medications were not developed concurrently with an explicitly stated a priori autism-related molecular target. Because behavioural intervention and psychosocial therapy modalities continue to form the foundation for systematically addressing core features of ASD (Carthy et al., 2023), the principal role for psychotropic medications is to act as an adjunctive treatment option aimed at managing “high frequency—high intensity” behavioural challenges and comorbid conditions (Feroe et al., 2021; Siafis et al., 2022).
There is evidence that, even within the current adjunctive role that psychotropic medication occupies in autism treatment models, medication is given to about a third (31%) of autistic children and adolescents (Rasmussen et al., 2019). In an Australian study, the most frequently- supplied medications were for symptoms of ADHD and (to a lesser extent) depression (Rasmussen et al., 2019). For autistic adults, Lim et al. (2021) found that 72% were taking at least one psychotropic medication, with 35% of participants receiving antidepressants (most commonly sertraline and escitalopram), 11% taking antipsychotics (most commonly quetiapine and risperidone), and 10% had prescriptions for hypnotics. Figures on the percentage of autistic people on psychotropic medication for Australia and the UK (e.g., Alfageh et al., 2020) appear lower than those for North America and Europe, where approximately 50% of autistic children/adolescents receive medication (Henneberry et al., 2021). Despite evidence that treatment via psychotropic medication is increasing, the prescribing process is challenging due to the complex presentation that arises from heterogeneity in symptom expression and severity, the high rates of co-existing disorders, and increased susceptibility to medication side effects (Genovese & Ellerbeck, 2022).
Considering that the reason for including psychotropic medication in an autism-specific treatment plan is to remediate the adverse effects of behavioural disturbances and/or comorbid conditions, it is worthwhile noting the efficacy of these medications for this purpose. Specific behavioural targets include irritability, physical aggression, outbursts, hyperactivity, self-injurious behaviour, emotion dysregulation, and sleep disturbances. Risperidone is the approved psychotropic treatment for challenging behaviours involving irritability and aggression in autistic people under 18 years of age (Lim et al., 2021). Efficacy-oriented systematic reviews, such as that conducted by de Pablo et al. (2023), agree that risperidone and aripiprazole are efficacious as interventions for irritability and emotional dysregulation but, despite this, researchers emphasise that these medications can only comprise one element of a multicomponent intervention and are best prescribed for only short-term usage. Seok et al. (2023) conducted a network meta-analysis of randomised control trials of the comparative efficacy of psychotropic medications prescribed to treat disruptive behaviour in young people (diagnoses included autism, ADHD, conduct disorder, disruptive behaviour disorder) and found that second-generation psychotropic medications with greater dopaminergic receptor affinity (e.g., risperidone) showed significant efficacy in reducing disruptive behaviour (Seok et al., 2023).
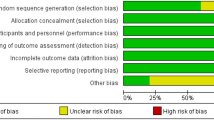
A longstanding caveat for this treatment is the recommendation to closely monitor autistic patients to establish tolerances and to identify the possible presence of adverse side effects (e.g., weight gain, insulin resistance, intense drowsiness, anxiety). Of further concern when considering the research basis for applying psychotropic medication with autistic persons is the argument made by Carthy et al. (2023), who found that pharmacological studies often contain a number of methodological flaws that do not permit generalizability of their findings across participant groups. Such flaws (e.g., inter-study variation in design and outcome measures, poor differentiation between the symptoms of autism and comorbid conditions, bias towards child participants) restrict the confidence with which clinicians are able to employ the findings from this field of research to make prescribing decisions for psychotropic medication (Bertelli, 2023).
In terms of future developments of psychotropic medications suitable for use with autistic people, Aishworiya et al. (2022) suggested that there is a solid foundation for targeted medications (e.g., oxytocin, metformin) capable of improving the core impairments in clearly differentiated autism subgroups. The definition of such autism subgroups depends on the use of neurobiological parameters that are inclusive of the clinical, behavioural, and biological variation inherent in autism. Boksha et al. (2023) proposed that these parameters should be developed from multi-method classifications (e.g., clinical assessment of behaviour, in-depth genetic investigation, brain/neural/molecular profiling) and embedded in studies involving large participant numbers in order to capture the full range of neurobiological domains that would require biomedical treatment. Further focussing of psychotropic medications on the specific underlying neural circuits involved in (for example) prosocial behaviour (Walsh et al., 2023) also has the potential to deliver individualised treatment protocols for autistic persons (Insel, 2013).
Neuromodulation Treatment
Neuromodulation is an umbrella term for a group of procedures in which brain function is altered by applying weak electrical current to particular brain regions that are thought to be responsible for specific behaviours, and which communicate with other brain regions via neural “connectivity” (Thivierge & Marcus, 2007). Although this “brain region-behaviour” model has been recently challenged by findings that suggest the shape of the brain may be more important than connectivity between brain regions in determining cortical activity (Pang et al., 2023), ongoing research still supports a role for the connectivity-across-regions explanation of brain-behaviour communication (Cabral et al., 2023; Murphy, 2023), including in autistic youth (Bitsika et al., 2023; Sarmukadam et al., 2023).
Neuromodulation may be undertaken by enhancing, suppressing, adjusting, and regulating neural activity and functioning (Henry et al., 2016) and is primarily used to treat disorders known to be under the influence of atypical nervous system functionality. Neuromodulation techniques are generally classed as being invasive (i.e., a surgical procedure is used to implant a stimulation device) or non-invasive (i.e., stimulation electrodes are placed on the cranium and removed after each session). Depending on the disorder under treatment, electrodes may be applied to the brain, spinal cord, and/or peripheral nerve tracks. Non-invasive techniques include transcranial magnetic stimulation (TMS) and direct current stimulation (DCS), with these modalities delivering magnetic stimulation (for TMS) or electrical current (for DCS) through probes positioned outside the head (for TMS) or on the surface of the skull (for DCS) over multiple sessions (indicated by the prefix r before TMS or DCS) (Lewis et al., 2016). (DCS may also have the prefix t, to denote transcranial application.) Non-invasive DCS and TMS techniques have been examined as therapeutic options for reducing the pathological neuroplasticity of autism, with particular improvements targeted for autism symptomatology, neurophysiological functions, and behavioural difficulties (Khaleghi et al., 2020).
In terms of efficacy, Khaleghi et al.’s (2020) systematic review of 32 studies of tDCS and rTMS (8 tDCS, 23 rTMS, and 1 tDCS plus rTMS studies) with autistic participants reported positive effects on repetitive and restricted behaviour, socialisation, and some aspects of executive cognitive functions. However, those authors cautioned against overly optimistic interpretations of the findings they reviewed, citing methodological limitations arising from poor study design, heterogeneity of data resulting from variations in stimulation protocols (e.g., the number of sessions ranged from single- to multiple applications), and bias towards adolescent/adult participant groups causing findings to be of low generalisability to children. These sentiments were echoed in Garcia-Gonzales et al.’s (2021) systematic review and meta-analysis of the use and effectiveness of tDCS in 16 studies of autistic children and adults. The left dorsolateral prefrontal cortex was the most frequently chosen brain site for stimulation, with improvements in socialisation, behavioural difficulties (e.g., irritability, agitation), and overall functionality. Like Khaleghi et al. (2020), Garcia-Gonzales et al. (2021) noted that the veracity of research findings was undermined by variation in methodology across studies, with a preponderance of studies not suited to evaluating efficacy across studies (e.g., n = 1 designs). Additionally, Smith et al. (2022) reviewed clinical trials involving the use of TMS to remediate behavioural and cognitive symptoms in autistic children/adolescents that were classified as being cognitively capable. Mild to moderate improvements were noted for restricted and repetitive behaviours, and strong increases were found in cognitive functions. However, despite these reasonably promising findings, Smith et al. (2022) also emphasised that limitations in study design needed to be addressed prior to these findings being translated into clinical recommendations. Most recently, Griff et al. (2023) discussed the therapeutic components and relative efficacy of non-invasive brain modulation techniques (e.g., tDCS, rTMS) in modifying pathological neuroplasticity in autism. Their analysis of findings from pilot and cohort studies plus clinical trials, suggested that there was some evidence that tDCS and rTMS created therapeutic improvements in the atypical behaviour and cognitive patterns observed in autism. However, those authors also suggested that research to date is unable to support a conclusive case for meaningful conclusions to be drawn, particularly regarding the issues of clinical significance and maintenance of effects over time.
Overall, these reviews were unanimous in their caution about voicing strong support for neurostimulation effects, principally due to persistent methodological flaws in study design and delivery. In offering suggestions for future research, they recommended development of standardised brain stimulation protocols and agreement on the outcome measures used to evaluate efficacy (Garcia-Gonzalez et al., 2021; Griff et al., 2023), use of design standards to aid accurate efficacy analyses (including randomised, double-blind controlled trials with embedded follow-up periods (Khaleghi et al., 2020)), use of technological advances such as neuronavigation software (Smith et al., 2022), exploration of a greater number of brain regions in which to deliver neurostimulation (Khaleghi et al., 2020), and incorporation of inter-disciplinary teams to create more insightful data-collection and data-interpretation processes (Zhang et al., 2021). On the bases of these reviews and studies, at present, it is most accurate to conclude that neuromodulation holds definite promise as a treatment for some of the core symptoms and associated features of autism, but cannot be recommended as an evidence-based treatment for this purpose yet.
Oxytocin Therapy
Oxytocin is a neuropeptide synthesised in the hypothalamus and secreted into the blood stream by the posterior pituitary. It is known to exert significant effects on social functioning and, due to this, has drawn interest as a biochemical treatment option for some of the features of autism (Tanaka et al., 2018). As a basis for treatment studies, oxytocin levels are lower in autistic people compared to same-age neurotypical peers. For example, in their meta-analysis of 31 studies that measured oxytocin concentration in plasma/serum (26 studies), saliva (4 studies), and cerebrospinal fluid (1 study) in 1233 autistic and 1304 neurotypical participants, John and Jaeggi (2021) reported significantly lower oxytocin levels in blood samples of autistic children compared to their neurotypical peers. Those authors also found positive correlations between oxytocin levels and autism symptom severity, supporting the hypothesis that the oxytocin system is implicated in onset and/or expression of autism impairment. However, this finding is not universal: Moerkerke et al. (2021) reported meta-analytic data indicating that oxytocin levels of autistic adolescents adults did not differ from those of their neurotypical counterparts.
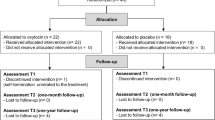
Four examples of empirical investigations of the effects of oxytocin on autistic symptoms provide an indication of the state of therapeutic research in this field. First, Daniels et al. (2023) employed a double-blind, randomised, placebo-controlled study to investigate the effects of a 4-week administration (12 IU delivered two times per day) of intranasal oxytocin on social responsiveness in 80 autistic children (age range = 8 to 12 years; 61 boys). Data were collected from parent-reported Social Responsiveness Scale (SRS-2) (Constantino & Gruber, 2012) responses. Children were randomly allocated to an oxytocin or placebo group, and oxytocin effects were measured at two time points (i.e., immediately after delivery of the final oxytocin dose and at 4-week follow-up). Daniels et al. (2023) reported significant improvement in social responsiveness for both oxytocin and placebo groups, leading to the conclusion that these positive effects were not solely an outcome of exposure to intranasal oxytocin.
Second, Guastella et al. (2023) reported contrasting results to those of Daniels et al. (2023) in their randomised, placebo-controlled clinical trial of intranasal efficacy in 87 autistic children (age range = 3 to 12 years). Intranasal oxytocin (32 IU = 16 IU morning + 16 IU evening) was administered to the treatment group over a 12-week period while the placebo group received a neutral spray delivered under the same conditions. Social functioning was measured using the parent-reported SRS-2 at pre- and-post trial. Overall, oxytocin had no significant effect on social responsiveness, and no significant effects were found for general mental well-being as rated by clinicians, nor for secondary measures involving repetitive and atypical behaviour.
Third, Sikich et al. (2021) confirmed the trend towards no significant oxytocin effect in their placebo-controlled trial of intranasal oxytocin in children/adolescents (age range 3 to 17 years) which extended over a 24-week period during which participants received 48 IU of oxytocin per day. Based on mean change scores on the Social Withdrawal Scale of the Aberrant Behaviour Checklist (Aman et al., 1985), Sikich et al. (2021) reported no significant treatment versus control group differences in social functioning over the 24-week trial period.
Fourth, a double-blind, randomised, placebo-controlled parallel design was used by Bernaerts et al. (2020) to address the issue of longer term effects of oxytocin. A sample of 40 adult autistic men received intranasal oxytocin (24 IU once per morning) for a 4-week period. Measures of autism symptomatology using the adult version of the SRS (Constantino, 2005) were taken at baseline, immediately following the 4-week trial, and at follow-up of 4 weeks, and 12-month post-treatment. Data were collected via self- and informant-reporting of status in relation to social impairment, repetitive behaviour, and attachment (Bernaerts et al., 2020), but no significant oxytocin treatment-related effects were found (men in both the treatment and placebo groups stated that they had experienced social improvements). However, treatment-related reductions were observed for secondary measures of repetitive behaviour and feelings of avoidance in the oxytocin group compared to the placebo group.
Although these four empirical studies suggest that the efficacy of oxytocin as a treatment for social interaction and communication difficulties in autism has yet to be proven, a meta-analysis of 28 studies (autistic participants = 726; mean age = 32.93 years; percentage male = 96.11%) by Huang et al. (2021) reported strong evidence of positive change in social, but not non-social behaviour (e.g., repetitive responses, stereotypies).
These results are not conclusive, and it is relevant to note the comment made by Ford and Young (2022) that, while oxytocin may facilitate social learning, there is no evidence that it also directly causes prosocial behaviour. Those authors argued that future studies of oxytocin ought to incorporate behaviour therapy protocols to actually teach social behaviour rather than relying on the effects of the neurohormone per se.
Oxytocin is a powerful stimulant, and is not without its negative sequalae. For example, in their systematic review and meta-analysis on the adverse events (i.e., side effects) associated with long-term intranasal oxytocin treatment in autistic participants, Cai et al. (2018) analysed findings from five randomised controlled trials (total participants = 223; intranasal oxytocin group = 123; placebo group = 100) and classified adverse events into mild and severe categories. The percentage of participants who experienced a mild adverse event ranged from 4.5 to 14.3%. Severe adverse events were infrequent (aggression = 3 participants; seizures = 2 participants). Although Cai et al. (2018) concluded that intranasal oxytocin was relatively well tolerated, they also urged the establishment of large clinical trials to evaluate its efficacy as a treatment modality. In terms of everyday clinical settings, it may be risky to assume that every autistic child will avoid side effects from oxytocin therapy. Furthermore, although oxytocin treatment may be a beneficial treatment option in some individuals, trends are not universal, and reported effects relate mostly to immediate rather than long-term change. The question of whether oxytocin effects are maintained over time can only be clarified with repeated post-treatment measures (Yamasue et al., 2020).
It is useful to reflect on several key points regarding this brief overview of the efficacy of oxytocin for treating social communication difficulties in autistic persons. First, the reported findings on oxytocin benefits are inconsistent in both child and adult participant groups. Second, despite being heavily populated by double-blind, randomised, placebo-controlled clinical trials that are well suited to efficacy research, methodological limitations exist. These are particularly related to issues such as over-reliance on informant-reporting methods to measure change, limited control, and accounting of additional exposures (e.g., social skill training) that are likely to influence participant performance, wide variation in oxytocin administration (e.g., dose and frequency/time of delivery), and lack of consistency in treatment duration. In assessing oxytocin treatment effects, minimal attention has been paid to instituting follow-up measures which would allow for conclusions to be drawn on longevity or maintenance of improvements in participant functioning. Most importantly, female participants continue to be under-represented in this line of biomedical research. Tabak and colleagues (Tabak et al., 2023) have provided a valuable state-of-the-art review regarding methodological issues in oxytocin efficacy studies, including the tissue source from which oxytocin is collected (saliva, plasma, urine, cerebrospinal fluid), the methods of extracting oxytocin from these fluids, the processes use to detect concentrations of oxytocin, the nature of the experimental task (vs baseline) which is being measured for its effect due to oxytocin administration, the heterogeneity of the autistic sample, and the methods of diagnosis and assessment of the particular neurodevelopmental disorder being studied. These are considerable challenges, and with the variety in outcomes reported from the small (but representative) sample of studies and reviews described here, leave oxytocin as a treatment with promise but yet to be evidence-based.
A Place for Individual Resilience?
Neurobiological investigations have generally centred on delineating the biological and environmental risk factors for autism in order to permit more accurate predictions of the manner in which core impairments are likely to influence functioning across the lifespan. While such studies have contributed to an array of specialised treatment approaches capable of assisting positive change, they have also unintentionally minimised exploration of individual’s unique strengths and talents as well as any protective factors that could aid positive development. On this point, Szatmari (2018) and Clark and Adams (2022) have argued for more studies into autism resiliency and the protective factors that influence the potential for resilient responses.
For some time, the positive psychology literature has defined resilience as the person’s capacity to resist the detrimental impacts of any adverse stressors encountered in life, and to continue functioning despite their presence (Herrman et al., 2011). Furthermore, resilience enhances adaptation to difficult experiences via use of cognitive, emotional, and behavioural strategies plus adjustment to environmental demands (Luthar & Cicchetti, 2000). Szatmari (2018) hypothesised that this definition can be applied to autism by conceptualising the diagnosis or exposure to risk factors as the adverse event, and “doing better than expected” in the face of a diagnosis/risk factors as the outcome (p. 225). Within this framework, protective factors (i.e., sex differences, infant siblings, natural history) may act to reduce the influence of risks that lead to poorer functional outcomes across the lifespan. There is evidence that resilience can help autistic boys cope more effectively with being bullied at school (Bitsika et al., 2022), and also is of value to their parents in managing their own stress, anxiety, and depression (Bitsika et al., 2013). The challenge to research thus centres not only on identifying specific protective variables but also mapping their influence from a longitudinal perspective. For example, Stallworthy and Masten (2023), using high-risk infant siblings as their example, have expanded on the importance of maintaining a resilient perspective as a counterpoint to risk-oriented views to help explain which resilience factors are significant to positive development despite presence of risk factors in early childhood. Those researchers differentiated between promotive variables (e.g., communication, self-regulation) and protective processes (e.g., female protective effect), arguing that investigation of predictors is necessary to explain how both sets of factors affect adaptive development and the time spent in this positive phase.
An example of a scale to measure resilience can provide a more detailed explanation of the protective factors underlying resilience. One of the most-used measures of what those authors refer to as “Psychological Resilience” (PR) is the Connor-Davison Resilience Scale (Connor & Davidson, 2003), which asks respondents to rate their level of agreement with 25 statements such as: I am able to adapt to change, When things look hopeless, I don’t give up, and I am in control of my life. As defined by Connor and Davidson (2003), PR is composed of five underlying components: personal competence, high standards, and tenacity; trust in one’s instincts, tolerance of negative affect; positive acceptance of change, secure relationships; control over one’s life; and spiritual influences. Not all of these have protective effects. Some data show that, although the first four components are significant inverse correlates of stress and depression in cancer patients, this is not so for the fifth component (Sharpley et al., 2017). Differential effects of the underlying components of PR as measured by the CDRISC are yet to be reported in autistic samples.
This paper is focussed upon neurobiological treatments for autism and comorbid conditions. Resilience is relevant because, although it was originally defined in psychological and behaviour terms, it has been shown to have profound biological, neurobiological, and environmental aspects (Paban et al., 2019; Velamuri et al., 2022), with a recent research focus on using EEG and MRI to define and describe the neurobiological processes that underlie resilient behaviour (Hasan et al., 2022; Long et al., 2019; Watanabe & Takeda, 2022). In their major reviews of the biology of resilience, Feder et al. (2019) and Boyce et al., (2021) noted that specific genes interact with environmental factors to influence the development of the neural circuitry that influences an individual’s responses to stress. These interactions occur particularly during developmental periods, and act via epigenetic mechanisms to influence the way that brain regions activate to mediate a threat, regulate emotional responses, producing adaptive neural pathways that enhance self-management of changing environmental settings and challenges. Therefore, resilience may be conceived as a psycho-neurobiological factor rather than simply a set of behavioural attributes. As such, clinical settings might reasonably emphasise the value of training resilience behaviours, aware that these processes may have an underlying neurobiological stratum that can be influenced by behavioural training.
Implications for Clinical Settings
Based upon the findings drawn from the key research papers briefly reviewed above, Table 1 focusses this information towards informing clinicians by presenting the major research findings, resources needed, and recommendations for use in clinical settings for each of the four treatments outlined above. As mentioned in the Introduction to this paper, there is no attempt to provide a detailed exhaustive review of all of the research on these treatments—that has been done before in other papers. Instead, this discussion is aimed at distilling the key information from those previous reviews, plus major individual empirical studies, so that these can be presented to clinicians in meaningful and (hopefully) valuable summary format.
Overall, these treatments represent relatively recent and neurobiologically based approaches to the challenges of autism. As such, most are in the development stage, and still reliant upon further research to establish their evidence-based validity for clinical applications. However, within that limitation, each holds clear promise (at least) of being of some value in assisting autistic persons to manage the particular demands of their individual features. While most should be applied with caution, or acknowledgement of their restrictive benefit (e.g., medication for comorbidities rather than autism core features), and the relative costs of their resources (e.g., TMS) and utilisation (e.g., medical training for psychopharmacology), each of these may be of value with specific clinical cases, and for designated purposes. Clinicians need to remain abreast of developments in their fields, and this brief summary provides an overview of the current information state in regard to these treatments which are based upon the underlying neurobiological concomitants of autism.
Data Availability
No new data were used in this report.
References
Aishworiya, R., Valica, T., Hagerman, R., & Restrepo, B. (2022). An update on psychopharmacological treatment of autism spectrum disorder. Neurotherapeutics, 19(1), 248–262. https://doi.org/10.1007/s13311-022-01183-1
Alfageh, B. H., Man, K. K., Besag, F. M., Alhawassi, T. M., Wong, I. C., & Brauer, R. (2020). Psychotropic medication prescribing for neuropsychiatric comorbidities in individuals diagnosed with autism spectrum disorder (ASD) in the UK. Journal of Autism and Developmental Disorders, 50(2), 625–633. https://doi.org/10.1007/s10803-019-04291-8
Aman, M., Singh, N., Stewart, A., & Field, C. (1985). The aberrant behavior checklist: A behavior ratings scale for the assessment of treatment effects. American Journal of Mental Deficiency, 89, 485–491.
APA. (2022). Diagnostic and Statistical Manual of Mental Disorders 5th Ed Text Revision. American Psychiatric Association. https://doi.org/10.1176/appi.books.9780890425787
Bernaerts, S., Boets, B., Bosmans, G., Steyaert, J., & Alaerts, K. (2020). Behavioral effects of multiple-dose oxytocin treatment in autism: A randomized, placebo-controlled trial with long-term follow-up. Molecular Autism, 11(1), 6. https://doi.org/10.1186/s13229-020-0313-1
Bertelli, M. O. (2023). Psychotropic medication for problem behaviours in intellectual disability and autism spectrum disorder: The need for caution. British Journal of Psychiatry Advances, 1–3. https://doi.org/10.1192/bja.2023.22
Bitsika, V., Sharpley, C. F., & Bell, R. (2013). The buffering effect of resilience upon stress, anxiety and depression in parents of a child with an autism spectrum disorder. Journal of Developmental and Physical Disabilities, 25(5), 533–543. https://doi.org/10.1007/s10882-013-9333-5
Bitsika, V., Heyne, D. A., & Sharpley, C. F. (2022). The inverse association between psychological resilience and emerging school refusal among bullied autistic youth. Research in Developmental Disabilities, 120, 104121. https://doi.org/10.1016/j.ridd.2021.104121
Bitsika, V., Sarmukadam, K., & Sharpley, C. F. (2023). Directional alpha frontoparietal connectivity and anxiety in autistic boys. Journal of Developmental and Physical Disabilities. https://doi.org/10.1007/s10882-023-09893-w
Boksha, I. S., Prokhorova, T. A., Tereshkina, E. B., Savushkina, O. K., & Burbaeva, G. S. (2023). Differentiated approach to pharmacotherapy of autism spectrum disorders: Biochemical aspects. Biochemistry (Moscow), 88(3), 303–318.
Boyce, W. T., Levitt, P., Martinez, F. D., McEwen, B. S., & Shonkoff, J. P. (2021). Genes, environments, and time: The biology of adversity and resilience. Pediatrics, 147(2). https://doi.org/10.1542/peds.2020-1651
Cabral, J., Fernandes, F. F., & Shemesh, N. (2023). Intrinsic macroscale oscillatory modes driving long range functional connectivity in female rat brains detected by ultrafast fMRI. Nature Communications, 14(1), 375. https://doi.org/10.1038/s41467-023-36025-x
Cai, Q., Feng, L., & Yap, K. Z. (2018). Systematic review and meta-analysis of reported adverse events of long-term intranasal oxytocin treatment for autism spectrum disorder. Psychiatry and Clinical Neurosciences, 72(3), 140–151. https://doi.org/10.1111/pcn.12627
Carthy, E., Ross, C., & Murphy, D. (2023). Psychotropic medication prescribing in people with autism spectrum disorders with and without psychiatric comorbidity. British Journal of Psychiatry Advances, 29(2), 131–140. https://doi.org/10.1192/bja.2021.32
Chawner, S. J., Doherty, J. L., Anney, R. J., Antshel, K. M., Bearden, C. E., Bernier, R., Chung, W. K., Clements, C. C., Curran, S. R., & Cuturilo, G. (2021). A genetics-first approach to dissecting the heterogeneity of autism: Phenotypic comparison of autism risk copy number variants. American Journal of Psychiatry, 178(1), 77–86. https://doi.org/10.1176/appi.ajp.2020.20010015
Clark, M., & Adams, D. (2022, 2022/03/01). Resilience in autism and intellectual disability: A systematic review. Review Journal of Autism and Developmental Disorders, 9(1), 39–53. https://doi.org/10.1007/s40489-021-00239-w
Connor, K., & Davidson, J. (2003). Development of a new resilience scale: The Connor-Davidson resilience scale (CD-RISC). Depression and Anxiety, 18(2), 76–82. https://doi.org/10.1002/da.10113
Constantino, J., & Gruber, C. (2012). Social Responsiveness Scale second edition (SRS-2). Western Psychological Services.
Constantino, J. (2005). Social Responsiveness Scale-Adult Research Version. Western Psychological Services.
Daniels, N., Moerkerke, M., Steyaert, J., Bamps, A., Debbaut, E., Prinsen, J., Tang, T., Van der Donck, S., Boets, B., & Alaerts, K. (2023). Effects of multiple-dose intranasal oxytocin administration on social responsiveness in children with autism: A randomized, placebo-controlled trial. Molecular Autism, 14(1), 16. https://doi.org/10.1186/s13229-023-00546-5
de Pablo, G. S., Pastor Jordá, C., Vaquerizo-Serrano, J., Moreno, C., Cabras, A., Arango, C., Hernández, P., Veenstra-VanderWeele, J., Simonoff, E., Fusar-Poli, P., Santosh, P., Cortese, S., & Parellada, M. (2023). Systematic review and meta-analysis: Efficacy of pharmacological interventions for irritability and emotional dysregulation in autism spectrum disorder and predictors of response. Journal of the American Academy of Child & Adolescent Psychiatry, 62(2), 151–168. https://doi.org/10.1016/j.jaac.2022.03.033
Feder, A., Fred-Torres, S., Southwick, S. M., & Charney, D. S. (2019). The biology of human resilience: Opportunities for enhancing resilience across the life span. Biological Psychiatry, 86(6), 443–453. https://doi.org/10.1016/j.biopsych.2019.07.012
Feroe, A. G., Uppal, N., Gutierrez-Sacristan, A., Mousavi, S., Greenspun, P., Surati, R., Kohane, I. S., & Avillach, P. (2021). Medication use in the management of comorbidities among individuals with autism spectrum disorder from a large nationwide insurance database. JAMA Pediatrics, 175(9), 957–965. https://doi.org/10.1001/jamapediatrics.2021.1329
Ford, C. L., & Young, L. J. (2022). Refining oxytocin therapy for autism: Context is key. Nature Reviews Neurology, 18(2), 67–68. https://doi.org/10.1038/s41582-021-00602-9
Frye, R. E. (2020). Mitochondrial dysfunction in autism spectrum disorder: Unique abnormalities and targeted treatments. Seminars in Pediatric Neurology, 35, 100829. https://doi.org/10.1016/j.spen.2020.100829
Frye, R. E., Cakir, J., Rose, S., Delhey, L., Bennuri, S. C., Tippett, M., Melnyk, S., James, S. J., Palmer, R. F., & Austin, C. (2021). Prenatal air pollution influences neurodevelopment and behavior in autism spectrum disorder by modulating mitochondrial physiology. Molecular Psychiatry, 26(5), 1561–1577. https://doi.org/10.1038/s41380-020-00885-2
Garcia-Gonzalez, S., Lugo-Marin, J., Setien-Ramos, I., Gisbert-Gustemps, L., Arteaga-Henriquez, G., Diez-Villoria, E., & Ramos-Quiroga, J. A. (2021). Transcranial direct current stimulation in autism spectrum disorder: A systematic review and meta-analysis. European Neuropsychopharmacology, 48, 89–109. https://doi.org/10.1016/j.euroneuro.2021.02.017
Genovese, A., & Ellerbeck, K. (2022). Autism spectrum disorder: A review of behavioral and psychiatric challenges across the lifespan. SN Comprehensive Clinical Medicine, 4(1), 217. https://doi.org/10.1007/s42399-022-01302-1
Griff, J. R., Langlie, J., Bencie, N. B., Cromar, Z. J., Mittal, J., Memis, I., Wallace, S., Marcillo, A. E., Mittal, R., & Eshraghi, A. A. (2023). Recent advancements in noninvasive brain modulation for individuals with autism spectrum disorder. Neural Regeneration Research, 18(6), 1191–1195. https://doi.org/10.4103/1673-5374.360163
Guastella, A. J., Boulton, K. A., Whitehouse, A. J., Song, Y. J., Thapa, R., Gregory, S. G., Pokorski, I., Granich, J., DeMayo, M. M., & Ambarchi, Z. (2023). The effect of oxytocin nasal spray on social interaction in young children with autism: A randomized clinical trial. Molecular Psychiatry, 28(2), 834–842. https://doi.org/10.1038/s41380-022-01845-8
Hasan, R. A., Ali, S. S. A., Tang, T. B., & Yusoff, M. S. B. (2022). Finding the EEG footprint of stress resilience. International Conference on Artificial Intelligence for Smart Community: AISC 2020, 17–18 December, Universiti Teknologi Petronas, Malaysia.
Henneberry, E., Lamy, M., Dominick, K. C., & Erickson, C. A. (2021). Decades of progress in the psychopharmacology of autism spectrum disorder. Journal of Autism and Developmental Disorders, 51, 4370–4394. https://doi.org/10.1007/s10803-021-05237-9
Henry, R., Deckert, M., Guruviah, V., & Schmidt, B. (2016). Review of neuromodulation techniques and technological limitations. IETE Technical Review, 33(4), 368–377.
Herrman, H., Stewart, D. E., Diaz-Granados, N., Berger, E. L., Jackson, B., & Yuen, T. (2011). What is resilience? The Canadian Journal of Psychiatry, 56(5), 258–265. https://doi.org/10.1177/0706743711056005
Huang, Y., Huang, X., Ebstein, R. P., & Yu, R. (2021). Intranasal oxytocin in the treatment of autism spectrum disorders: a multilevel meta-analysis. Neuroscience & Biobehavioral Reviews, 122, 18–27. https://doi.org/10.1016/j.neubiorev.2020.12.028
Insel, T. (2013). Transforming diagnosis. National Institute of Mental Health. Retrieved May 27 from https://www.nimh.nih.gov/about/director/2013/transforming-diagnosis-shtml
John, S., & Jaeggi, A. V. (2021). Oxytocin levels tend to be lower in autistic children: A meta-analysis of 31 studies. Autism, 25(8), 2152–2161. https://doi.org/10.1177/13623613211034
Khaleghi, A., Zarafshan, H., Vand, S. R., & Mohammadi, M. R. (2020). Effects of non-invasive neurostimulation on autism spectrum disorder: A systematic review. Clinical Psychopharmacology and Neuroscience, 18(4), 527. https://doi.org/10.9758/cpn.2020.18.4.527
Lewis, P. M., Thomson, R. H., Rosenfeld, J. V., & Fitzgerald, P. B. (2016). Brain neuromodulation techniques: A review. The Neuroscientist, 22(4), 406–421. https://doi.org/10.1177/1073858416646707
Lim, R., Moffat, A. K., Young, R., & Kalisch Ellett, L. M. (2021). Use of medicines in adults with autism spectrum disorder in Australia. Journal of Pharmacy Practice and Research, 51(5), 410–414. https://doi.org/10.1002/jppr.1745
Long, Y., Chen, C., Deng, M., Huang, X., Tan, W., Zhang, L., Fan, Z., & Liu, Z. (2019). Psychological resilience negatively correlates with resting-state brain network flexibility in young healthy adults: A dynamic functional magnetic resonance imaging study. Annals of Translational Medicine, 7(24), 809. https://doi.org/10.21037/atm.2019.12.45
Luthar, S., & Cicchetti, D. (2000). The construct of resilience: Implications for interventions and social policies. Development and Psychopathology, 12(4), 857–885. https://doi.org/10.1017/s0954579400004156
Moerkerke, M., Peeters, M., de Vries, L., Daniels, N., Steyaert, J., Alaerts, K., & Boets, B. (2021). Endogenous oxytocin levels in autism—A meta-analysis. Brain Sciences, 11(11), 1545. https://doi.org/10.3390/brainsci11111545
Murphy, E. (2023). ROSE: A neurocomputational architecture for syntax. arXiv preprint arXiv:2303.08877. https://www.ncbi.nlm.nih.gov/pubmed/36994166
Nordahl, C. W., Andrews, D. S., Dwyer, P., Waizbard-Bartov, E., Restrepo, B., Lee, J. K., Heath, B., Saron, C., Rivera, S. M., & Solomon, M. (2022). The autism phenome project: Toward identifying clinically meaningful subgroups of autism. Frontiers in Neuroscience, 15, 786220. https://doi.org/10.3389/fnins.2021.786220
Paban, V., Modolo, J., Mheich, A., & Hassan, M. (2019). Psychological resilience correlates with EEG source-space brain network flexibility. Network Neuroscience, 3(2), 539–550. https://doi.org/10.1162/netn_a_00079
Pang, J. C., Aquino, K. M., Oldehinkel, M., Robinson, P. A., Fulcher, B. D., Breakspear, M., & Fornito, A. (2023). Geometric constraints on human brain function. Nature, 618(7965), 1–9. https://doi.org/10.1038/s41586-023-06098-1
Rasmussen, L., Pratt, N., Roughead, E., & Moffat, A. (2019). Prevalence of psychotropic medicine use in Australian children with autism spectrum disorder: A drug utilization study based on children enrolled in the longitudinal study of Australian children. Journal of Autism and Developmental Disorders, 49, 227–235. https://doi.org/10.1007/s10803-018-3718-3
Riordan, N. H., Hincapié, M. L., Morales, I., Fernández, G., Allen, N., Leu, C., Madrigal, M., Paz Rodríguez, J., & Novarro, N. (2019). Allogeneic human umbilical cord mesenchymal stem cells for the treatment of autism spectrum disorder in children: Safety profile and effect on cytokine levels. Stem Cells Translational Medicine, 8(10), 1008–1016. https://doi.org/10.1002/sctm.19-0010
Rossignol, D. A., & Frye, R. E. (2021). Cerebral folate deficiency, folate receptor alpha autoantibodies and leucovorin (folinic acid) treatment in autism spectrum disorders: A systematic review and meta-analysis. Journal of Personalized Medicine, 11(11), 1141. https://doi.org/10.3390/jpm11111141
Sarmukadam, K., Bitsika, V., & Sharpley, C. F. (2023). Frontoparietal connectivity, sensory features, and anxiety in children and adolescents with autism spectrum disorder. Advances in Neurodevelopmental Disorders, 7(1), 14–26. https://doi.org/10.1007/s41252-022-00271-9
Seok, J.-W., Soltis-Vaughan, B., Lew, B. J., Ahmad, A., Blair, R., & Hwang, S. (2023). Psychopharmacological treatment of disruptive behavior in youths: Systematic review and network meta-analysis. Scientific Reports, 13(1), 6921. https://doi.org/10.1038/s41598-023-33979-2
Sharpley, C., Christie, D., Bitsika, V., Agnew, L., Andronicos, N., & McMillan, M. (2017). Does psychological resilience buffer against the link between the 5-HTTLPR polymorphism and depression following stress? Physiology and Behavior, 180, 53–59. https://doi.org/10.1016/j.physbeh.2017.07.029
Siafis, S., Çıray, O., Wu, H., Schneider-Thoma, J., Bighelli, I., Krause, M., Rodolico, A., Ceraso, A., Deste, G., & Huhn, M. (2022). Pharmacological and dietary-supplement treatments for autism spectrum disorder: A systematic review and network meta-analysis. Molecular Autism, 13(1), 1–17. https://doi.org/10.1186/s13229-022-00488-4
Sikich, L., Kolevzon, A., King, B. H., McDougle, C. J., Sanders, K. B., Kim, S.-J., Spanos, M., Chandrasekhar, T., Trelles, M. P., & Rockhill, C. M. (2021). Intranasal oxytocin in children and adolescents with autism spectrum disorder. New England Journal of Medicine, 385(16), 1462–1473. https://doi.org/10.1056/NEJMoa2103583
Smith, J. R., DiSalvo, M., Green, A., Ceranoglu, T. A., Anteraper, S. A., Croarkin, P., & Joshi, G. (2022). Treatment response of transcranial magnetic stimulation in intellectually capable youth and young adults with autism spectrum disorder: A systematic review and meta-analysis. Neuropsychology Review, 1–22. https://doi.org/10.1007/s11065-022-09564-1
Stallworthy, I. C., & Masten, A. S. (2023). Advancing research on early autism through an integrated risk and resilience perspective. Development and Psychopathology, 35(1), 44–61. https://doi.org/10.1017/S0954579421001437
Szatmari, P. (2018). Risk and resilience in autism spectrum disorder: A missed translational opportunity? Developmental Medicine & Child Neurology, 60(3), 225–229. https://doi.org/10.1111/dmcn.13588
Tabak, B. A., Leng, G., Szeto, A., Parker, K. J., Verbalis, J. G., Ziegler, T. E., Lee, M. R., Neumann, I. D., & Mendez, A. J. (2023). Advances in human oxytocin measurement: Challenges and proposed solutions. Molecular Psychiatry, 28(1), 127–140. https://doi.org/10.1038/s41380-022-01719-z
Tanaka, A., Furubayashi, T., Arai, M., Inoue, D., Kimura, S., Kiriyama, A., Kusamori, K., Katsumi, H., Yutani, R., & Sakane, T. (2018). Delivery of oxytocin to the brain for the treatment of autism spectrum disorder by nasal application. Molecular Pharmaceutics, 15(3), 1105–1111. https://doi.org/10.1021/acs.molpharmaceut.7b00991
Taniya, M. A., Chung, H.-J., Al Mamun, A., Alam, S., Aziz, M. A., Emon, N. U., Islam, M. M., Podder, B. R., Ara Mimi, A., & Aktar Suchi, S. (2022). Role of gut microbiome in autism spectrum disorder and its therapeutic regulation. Frontiers in Cellular and Infection Microbiology, 12, 998. https://doi.org/10.3389/fcimb.2022.915701
Thivierge, J.-P., & Marcus, G. F. (2007). The topographic brain: From neural connectivity to cognition. Trends in Neurosciences, 30(6), 251–259. https://doi.org/10.1016/j.tins.2007.04.004
Velamuri, R., Hobson, N., Johnson, M., Skene, P., Dzirasa, K., & Hultman, R. (2022). P208. Stress resilience in amygdala cellular subpopulation. Biological Psychiatry, 91(9), S171. https://doi.org/10.1016/j.biopsych.2022.02.442
Vorstman, J. A., Parr, J. R., Moreno-De-Luca, D., Anney, R. J., Nurnberger, J. I., Jr., & Hallmayer, J. F. (2017). Autism genetics: Opportunities and challenges for clinical translation. Nature Reviews Genetics, 18(6), 362–376. https://doi.org/10.1038/nrg.2017.4
Walsh, J. J., Christoffel, D. J., & Malenka, R. C. (2023). Neural circuits regulating prosocial behaviors. Neuropsychopharmacology, 48(1), 79–89. https://doi.org/10.1038/s41386-022-01348-8
Watanabe, N., & Takeda, M. (2022). Neurophysiological dynamics for psychological resilience: A view from the temporal axis. Neuroscience Research, 175, 53–61. https://doi.org/10.1016/j.neures.2021.11.004
Yamasue, H., Okada, T., Munesue, T., Kuroda, M., Fujioka, T., Uno, Y., Matsumoto, K., Kuwabara, H., Mori, D., & Okamoto, Y. (2020). Effect of intranasal oxytocin on the core social symptoms of autism spectrum disorder: A randomized clinical trial. Molecular Psychiatry, 25(8), 1849–1858. https://doi.org/10.1038/s41380-018-0097-2
Zhang, Y., Liu, X., Guo, R., Xu, W., Guo, Q., Hao, C., Ni, X., & Li, W. (2021). Biological implications of genetic variations in autism spectrum disorders from genomics studies. Bioscience Reports, 41(7). https://doi.org/10.1042/BSR20210593
Funding
Open Access funding enabled and organized by CAUL and its Member Institutions No funding was received for this study
Author information
Authors and Affiliations
Contributions
VB and CFS devised the concept; VB and CFS searched the literature; VB wrote the first draft of the ms; CFS revised the ms; both VB and CFS approved the final version of the ms.
Corresponding author
Ethics declarations
Ethics Approval
No human or animal participants were recruited for this study
Conflict of Interest
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Bitsika, V., Sharpley, C.F. Current Status of Psychopharmacological, Neuromodulation, and Oxytocin Treatments for Autism: Implications for Clinical Practice. Adv Neurodev Disord 8, 355–364 (2024). https://doi.org/10.1007/s41252-023-00364-z
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s41252-023-00364-z