Abstract
Numerous studies have determined that lifestyle factors (smoking, drinking, snacking, etc.) and the bedroom environment can influence sleep. We developed a new sleep scale—the 3-Dimensional Sleep Scale (3DSS)—which measures three elements of sleep: phase, quality, and quantity. The purpose of this study is to determine which risk factors of sleep complaints are associated with these sleep elements. Data were obtained from 366 Japanese day workers (302 men and 64 women). Sleep condition was assessed with the 3DSS, and we also assessed various habits within 2 h of going to bed, including smoking, drinking, snacking, caffeine intake, mobile phone use, and working. We also asked about bedroom environmental conditions (noise, lighting, and temperature and humidity). Multivariate logistic regression analysis using the backward selection method (likelihood ratio) was used, with 3DSS scores as the outcome (i.e., over or under the cutoff). The results showed that smoking was associated with significantly greater odds ratio [2.71 (1.65–4.44)] of disordered sleep phase, while lighting as well as temperature and humidity led to greater odds [3.67 (1.55–8.68), 1.93 (1.20–3.11)] of poor sleep quality. Finally, only noise was significantly related to greater odds [1.98 (1.13–3.46)] of low sleep quantity. These findings indicated the various risk factors of sleep complaints could be associated with different sleep elements. This might help in the effective treatment of sleep complaints.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Japanese people are well-known to be hard workers, and they often think that working at the cost of sleep is a virtue. Ironically, sleep is essential for working efficiently and for the health of workers. Obesity, hypertension, diabetes, and depression, all of which are common diseases among workers, are associated with sleep complaints [1,2,3,4]. Beyond such health problems, sleep complaints are frequently implicated in workplace problems, such as low productivity, risk of accidents, and conflict in personal relationships [5,6,7,8]. Thus, neglect of sleep can lead to considerable disadvantages in both individuals and organizations.
Although individuals with serious sleep disorder must be referred to a medical institution, self-management is required for the majority of cases. Indeed, the major controllable risk factors of sleep disorder are behaviors or activities before bed and the bedroom environment. Smoking, drinking, snacking, and caffeine, which are together referred to as shiko-hin in Japan, have been implicated in sleep disorders [9,10,11,12]. Other relevant behaviors include use of a mobile phone and working before going to bed, which can enhance wakefulness [13, 14]. In terms of environmental risks, there are three major factors—noise, lighting, and temperature and humidity—that must be considered when attempting to achieve good sleep [15,16,17,18].
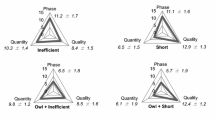
In the past, we established that sleep comprises three measurable elements—phase, quality, and quantity—which we then integrated into an original scale called the 3-Dimensional Sleep Scale (3DSS) [19, 20]. In our current 24-h society, people often exhibit problems in their sleep phase (e.g., regularity and chronotype), as well as in their sleep quality (e.g., sleep efficiency and satisfaction) and quantity (e.g., sleep duration and fullness). Previous studies have reported that sleep phase problems may be related to certain mental disorders independent of sleep quality and quantity [21]. In addition, sleep quality and quantity might have somewhat different relationships with depression [22,23,24]. In particular, the behaviors related to poor sleep quality (e.g., difficulty falling asleep) and poor sleep quantity (e.g., lack of sleep) are rather different. Given the differing properties of these sleep elements, it would be exceedingly difficult to provide organizational or clinical support correctly if the elements are not considered separately. Therefore, it is important that these sleep elements be assessed separately to fully grasp the details of individuals’ sleep problems. Problematically, most previous studies investigating the influence of bedtime habits or environment have examined only one or two of these three sleep elements (e.g., insomnia, sleep duration, or circadian rhythms); at present, we do not believe that any studies have investigated the specific risk factors of all three sleep elements. The purpose of the present study is to examine which factors are known to be associated with sleep complaints—in particular bedroom habits and environmental factors—more strongly influence these three sleep elements.
Methods
Participants
Data were collected in April 2015, with the cooperation of a company (that mainly provided manufacturing services) in Japan. We gave participants the questionnaires at their workplace and then collected the questionnaires later that day. A total of 446 Japanese employees responded; however, we ultimately excluded shift workers and respondents with missing data (n = 80), leaving 366 day workers (302 males and 64 females) for analysis. The mean ± standard deviation of age was 43.9 ± 8.8 years (males: 43.8 ± 8.9, females: 44.3 ± 8.3).
Measures
Sleep condition was measured with the 3DSS. This scale was designed for use with Japanese day workers and its reliability and validity have been established [19]. The 3DSS comprises three categories (sleep phase, quality, and quantity), each comprising 5 items (for a total of 15); all items ask about usual sleep habits in the past month. The sleep phase items are as follows: “(1) I go to bed at a fixed, regular time on weekdays and weekends”; “(2) I wake up at a fixed, regular time on weekdays and weekends”; “(3) I have a well-balanced breakfast every day;” “(4) ‘Morningness’ is better suited to me than is ‘eveningness’”; and “(5) What time do you wake up on weekdays?” The items assessing sleep quality are as follows: “(6) It takes me more than 30 min to fall asleep”; “(7) I wake up more than twice a night”; “(8) I wake up earlier than usual (over 2 h) and cannot fall asleep again;” “(9) I don’t sleep soundly”; and “(10) I worry that I cannot fall asleep”. Finally, the sleep quantity items are as follows: “(11) I sleep for less than 6 h on weekdays”; “(12) I cannot get enough sleep even though I want to”; “(13) I don’t feel free from sleepiness or fatigue when I wake up”; “(14) I feel sleepy not only in the afternoon, but also in the morning and/or evening;” and “(15) I often doze off”. To answer the items, respondents must choose the response option that best fits their sleep habits from among four choices, as follows (except for item no. 5): (1) always, (2) often, (3) rarely, and (4) never. For item no. 5, the options are (1) about 6:00 a.m. or earlier than 6:00 a.m., (2) about 6:30 a.m., (3) about 7:00 a.m., and (4) later than 7:00 a.m. As for the scoring, answers (1)–(4) are given scores of 3–0, respectively, for the sleep phase items (no. 1–5), and scores of 0–3 for the sleep quality and quantity items (no. 6–15). Each category’s score ranges from 0 to 15, with higher scores indicating better sleep condition. The cutoff scores for disordered sleep were 8/9 for sleep phase and quantity and 10/11 for sleep quality [25].
Bedtime habits were assessed as follows: “Please check all behaviors that you usually perform within the 2 h before going to bed: smoking, drinking, snacking, intake of caffeine, mobile phone use, and working”. For bedtime environmental factors, we assessed noise, lighting, and temperature and humidity in the bedroom. The specific questions and response options are the follows: “How noisy is your bedroom when you go to bed?” (1 = silent; 2 = noisy, but it does not prevent me from sleeping; 3 = noisy and it prevents me from sleeping). “How is the lighting in your bedroom when you go to bed?” (1 = dark; 2 = lit, but it does not prevent me from sleeping; 3 = lit and it prevents me from sleeping). “How is the temperature and humidity in your bedroom when you go to bed?” (1 = comfortable; 2 = uncomfortable, but it does not prevent me from sleeping; 3 = uncomfortable and it prevents me from sleeping). Only two participants selected option 3 for the noise question, and no one selected 3 for the other two questions. Thus, we decided to classify participants into two groups: those who selected 1 [i.e., environmental risk (−)] and those who selected 2 or 3 [environmental risk (+)].
Statistical analyses
IBM SPSS Statistics 23 was used for the analysis, with a significance level set at p < 0.05. We used unpaired t tests and analyses of variance (ANOVAs) as univariate analyses. Then, a multivariate logistic regression was run, using the backward selection method (likelihood ratio), to calculate odds ratios (ORs) and 95% confidence internals (CIs).
Ethical considerations
We ensured that none of the participants were pressured or harmed due to nonparticipation, and made it known that their responses to the questionnaires constituted informed consent to participate. The subjects received no reward for participation. Personal data were strictly monitored to ensure confidentiality and protect participants’ privacy. This study was approved by the Kurume University Ethics Review Board and informed consent was obtained.
Results
Table 1 shows the 3DSS scores according to gender, age, and marital status, as well as the number and percentage of participants whose 3DSS scores were under the cutoff points. A significant difference between men and women was found for sleep quality score only, with women showing a higher score than men. There were significant differences in all 3DSS scores according to participants’ age. Specifically, sleep phase score increased with age. Multiple comparisons revealed significant differences between participants in the over-50 group and participants in all other ages (p < 0.001); we also found a significant difference between participants aged under 29 and those aged 40–49 (p = 0.004). Significant differences were also apparent between the 30–39 and over-50 (p = 0.003) groups in sleep quality score and between the 40–49 and over-50 (p = 0.022) groups in sleep quantity score. We observed significant differences between single and married participants in sleep phase scores.
Table 2 shows the 3DSS scores according to bedtime habits. Sleep phase score was lower among those who were smoking and who used a mobile phone, while sleep quality score was higher among those who used a mobile phone. Sleep quantity scores were lower in those who did not drink, those who used a mobile phone, and those who worked.
Table 3 shows the 3DSS scores according to bedroom environment. Sleep quality scores significantly differed by all environmental factors, while only noise showed a significant difference in sleep quantity score.
Table 4 shows the results of the multiple regression analysis with 3DSS scores (over or under the cutoff score) set as the outcome. We found that participants who smoked had greater odds of poor sleep phase scores; snacking was also retained in the final step, but it was not significant. Furthermore, participants in the lighting (+) and temperature and humidity (+) groups both had greater odds of poor sleep quality. Finally, while mobile phone use, working, and noise remained in the final step of the analysis, only noise (+) had a significantly greater odds of low sleep quantity.
Discussion
We demonstrated which risk factors of sleep complaints (bedtime habits and environment) are associated with the three elements of sleep (phase, quality, and quantity). Whereas previous sleep studies tended to cover only one or two elements of sleep, we investigated all three and found that they were associated with different risk factors. This suggests that it is necessary to assess sleep phase, quality, and quantity separately to clarify the causes of sleep complaints and respond appropriately. Compared to a previous study [20], the prevalence of poor sleep phase in this study was lower while that of poor sleep quality or quantity were similar. Specifically, the previous study reported that the prevalence of poor sleep phase was about 44%, whereas in this study, it was 37%. The difference might be because the average age of the participants in this study was higher than was that of the previous study, given that younger individuals tend to have lower sleep phase scores.
Smoking was found to be the strongest risk factor of sleep phase problems. Nicotine has an arousal function and a half-life of around 2 h [26], which means that people who smoke within 2 h of going to bed might stay up later. Additionally, changing the number of cigarettes or start time of smoking can result in irregular sleep onset. Snacking was retained in the final step of the regression analysis, and although it was not significant, this result suggests that its connection is stronger than are those of the other risk factors. Snacking before bed might make people feel less hungry in the morning, and thus can cause them to skip breakfast. Skipping breakfast can make it difficult to synchronize the periphery circadian rhythm with the central circadian rhythm [27, 28], thereby leading to irregular sleep patterns and an eveningness lifestyle. Another possibility is that people who were classified as having an eveningness lifestyle tend to like shiko-hin [29] and pay little attention to their health. Therefore, a lack of health-consciousness might underlie the relationships between poor sleep phase, smoking, and snacking. The above-mentioned can apply to people with irregular sleep based on inadequate sleep hygiene rather than the patients suffering from delayed sleep-phase disorder.
As for sleep quality, lighting was the strongest risk factor, followed by temperature and humidity. The production of melatonin is inhibited even by normal room light (particularly over 100 lx) [30]. During sleep, light that is over 30 lx can impair both slow-wave and rapid-eye movement (REM) sleep [31]. While actual bedroom illuminance could not be measured in this study, it was still found to have a significant impact on the odds of reporting poor sleep quality. Regarding temperature and humidity, unsuitable temperatures (i.e., excessively hot or cold) can make it difficult to stay asleep and impairs both slow-wave and REM sleep [17]; high humidity can also make it difficult to stay asleep and can impair slow-wave sleep [18]. Because skin temperature increases with perspiration and the core body temperature must decrease to sleep soundly, unsuitable temperature and humidity would disturb the functioning of these systems.
Interestingly, most participants who reported these environmental risk factors did not feel that the factors actually prevented them from sleeping. This is perhaps because participants felt that even when the factors were present, they were not a problem if participants had no difficulty in falling asleep. Nevertheless, the impaired slow-wave and REM sleep due to inappropriate lighting or temperature and humidity typically manifest as difficulty in maintaining sleep rather than difficulty in falling asleep.
Noise was the strongest risk factor of sleep quantity. Noise louder than 40 dB during sleep can activate autonomic responses and increase cortisol levels on wake-up, thus leading to excessive daytime fatigue, sleepiness, and declining performance [15]. Additionally, at around 5 h after sleep onset, sleep is typically in the shallow stages (stage 1–2), which means that people are awoken more easily by noise and their sleep duration is thus cut short. Furthermore, these physical responses do not adapt to chronic exposure to noise, whereas subjective sleep satisfaction can [15]. These facts indicate why noise influences sleep quantity to a greater degree than sleep quality.
Importantly, mobile phone use and working remained at the final step of the regression analysis, albeit without significance. Some previous studies have shown that there is a relationship between lack of sleep or tiredness and these practices [13, 14, 32]. This is perhaps because they capture people’s attention before sleep, thus reducing their sleep duration. It is possible that a significant association between sleep quantity and these practices would be found if a larger sample were used. Working, in particular, had the largest effect size of all factors. It is likely that overwork could reduce sleep duration more than any other lifestyle or bedroom environment factor. Furthermore, blue light can reduce production of melatonin and thereby delay sleep phases or lead to declines in sleep quality [33]; however, some specialists have proposed that the amount of light coming from a mobile phone at a moderate distance has rather little effect on melatonin production [34]. Nevertheless, these past studies offer some support as to why mobile phone use was associated with sleep quantity, rather than sleep phase or quality.
The present study shows that the risk factors of sleep complaints appear to be associated with different sleep elements. Shiko-hin, such as smoking and snacking, is closely related to lifestyle rhythm. Lighting as well as temperature and humidity may be primarily related to the first stages of sleep (i.e., slow-wave sleep appearing), whereas noise is related to the last stages (i.e., shallow sleep and waking up easily). The differences in the characteristics of these factors might underlie their differing relationships with the various sleep elements. Therefore, when identifying patterns of sleep complaints, it would be important to focus on the risk factors present before attempting treatment.
Limitations
This study has some limitations. First, we could not infer any causal relationships between sleep elements and risk factors because the study was cross-sectional. Second, the data on noise, lighting, and temperature and humidity were not detailed because these factors were not objectively measured with equipment. Finally, we included no information on mental or physical diseases or medications being taken, or other factors important for workers such as educational attainment and job rank. In addition, the number of participants, especially in the under-29 age group and women, was insufficient to reflect the characteristics of the wider population. These are important to consider because sleep architecture and work styles differ between the young and old, as well as between men and women. Further research with more participants using stratified sampling, and including data on diseases and medicines, would be needed to better establish the associations found herein.
References
Gangwisch JE, Malaspina D, Boden-Albala B, Heymsfield SB. Inadequate sleep as a risk factor for obesity: analyses of the NHANES I. Sleep. 2005;28(10):1289–96.
Gangwisch JE, Heymsfield SB, Boden-Albala B, Buijs RM, Kreier F, Pickering TG, Rundle AG, Zammit GK, Malaspina D. Sleep duration as a risk factor for diabetes incidence in a large US sample. Sleep. 2007;30(12):1667–73.
Gottlieb DJ, Redline S, Nieto FJ, Baldwin CM, Newman AB, Resnick HE, Punjabi NM. Association of usual sleep duration with hypertension: the Sleep Heart Health study. Sleep. 2006;29(8):1009–14.
Watson NF, Harden KP, Buchwald D, Vitiello MV, Pack AI, Strachan E, Goldberg J. Sleep duration and depressive symptoms: a gene–environment interaction. Sleep. 2014;37(2):351–8.
Sarsour K, Kalsekar A, Swindle R, Foley K, Walsh JK. The association between insomnia severity and healthcare and productivity costs in a health plan sample. Sleep. 2011;34(4):443–50.
Salminen S, Oksanen T, Vahtera J, Sallinen M, Harma M, Salo P, Virtanen M, Kivimaki M. Sleep disturbances as a predictor of occupational injuries among public sector workers. J Sleep Res. 2010;19(1 Pt 2):207–13.
Niedhammer I, David S, Degioanni S, Drummond A, Philip P, Acquarone D, Aicardi F, Andre-Mazeaud P, Arsento M, Astier R, Baille H, Bajon-Thery F, Barre E, Basire C, Battu JL, Baudry S, Beatini C, Beaud’huin N, Becker C, Bellezza D, Beque C, Bernstein O, Beyssier C, Blanc-Cascio F, Blanchet N, Blondel C, Boisselot R, Bordes-Dupuy G, Borrelly N, Bouhnik D, Boulanger MF, Boulard J, Borreau P, Bourret D, Boustiere AM, Breton C, Bugeon G, Buono-Michel M, Canonne JF, Capella D, Cavin-Rey M, Cervoni C, Charreton D, Charrier D, Chauvin MA, Chazal B, Cougnot C, Cuvelier G, Dalivoust G, Daumas R, Debaille A, De Bretteville L, Delaforge G, Delchambre A, Domeny L, Donati Y, Ducord-Chapelet J, Duran C, Durand-Bruguerolle D, Fabre D, Faivre A, Falleri R, Ferrando G, Ferrari-Galano J, Flutet M, Fouche JP, Fournier F, Freyder E, Galy M, Garcia A, Gazazian G, Gerard C, Girard F, Giuge M, Goyer C, Gravier C, Guyomard A, Hacquin MC, Halimi E, Ibagnes T, Icart P, Jacquin MC, Jaubert B, Joret JP, Julien JP, Kacel M, Kesmedjian E, Lacroix P, Lafon-Borelli M, Lallai S, Laudicina J, Leclercq X, Ledieu S, Leroy J, Leroyer L, Loesche F, Londi D, Longueville JM, Lotte MC, Louvain S, Loze M, Maculet-Simon M, Magallon G, Marcelot V, Mareel MC, Martin P, Masse AM, Meric M, Milliet C, Mokhtari R, Monville AM, Muller B, Obadia G, Pelser M, Peres L, Perez E, Peyron M, Peyronnin F, Postel S, Presseq P, Pyronnet E, Quinsat C, Raulot-Lapointe H, Rigaud P, Robert F, Robert O, Roger K, Roussel A, Roux JP, Rubini-Remigy D, Sabate N, Saccomano-Pertus C, Salengro B, Salengro-Trouillez P, Samson E, Sendra-Gille L, Seyrig C, Stoll G, Tarpinian N, Tavernier M, Tempesta S, Terracol H, Torresani F, Triglia MF, Vandomme V, Vieillard F, Vilmot K, Vital N. Workplace bullying and sleep disturbances: findings from a large scale cross-sectional survey in the French working population. Sleep. 2009;32(9):1211–9.
Takaki J, Taniguchi T, Fukuoka E, Fujii Y, Tsutsumi A, Nakajima K, Hirokawa K. Workplace bullying could play important roles in the relationships between job strain and symptoms of depression and sleep disturbance. J Occup Health. 2010;52(6):367–74.
Zhang L, Samet J, Caffo B, Punjabi NM. Cigarette smoking and nocturnal sleep architecture. Am J Epidemiol. 2006;164(6):529–37.
Van Reen E, Roane BM, Barker DH, McGeary JE, Borsari B, Carskadon MA. Current alcohol use is associated with sleep patterns in first-year college students. Sleep. 2016;39(6):1321–6.
Miyata S, Noda A, Ito N, Atarashi M, Yasuma F, Morita S, Koike Y. REM sleep is impaired by a small amount of alcohol in young women sensitive to alcohol. Intern Med. 2004;43(8):679–84.
Van Dongen HP, Price NJ, Mullington JM, Szuba MP, Kapoor SC, Dinges DF. Caffeine eliminates psychomotor vigilance deficits from sleep inertia. Sleep. 2001;24(7):813–9.
Munezawa T, Kaneita Y, Osaki Y, Kanda H, Minowa M, Suzuki K, Higuchi S, Mori J, Yamamoto R, Ohida T. The association between use of mobile phones after lights out and sleep disturbances among Japanese adolescents: a nationwide cross-sectional survey. Sleep. 2011;34(8):1013–20.
Virtanen M, Ferrie JE, Gimeno D, Vahtera J, Elovainio M, Singh-Manoux A, Marmot MG, Kivimaki M. Long working hours and sleep disturbances: the Whitehall II prospective cohort study. Sleep. 2009;32(6):737–45.
Muzet A. Environmental noise, sleep and health. Sleep Med Rev. 2007;11(2):135–42.
Chellappa SL, Gordijn MC, Cajochen C. Can light make us bright? Effects of light on cognition and sleep. Prog Brain Res. 2011;190:119–33.
Haskell EH, Palca JW, Walker JM, Berger RJ, Heller HC. The effects of high and low ambient temperatures on human sleep stages. Electroencephalogr Clin Neurophysiol. 1981;51(5):494–501.
Okamoto-Mizuno K, Tsuzuki K, Mizuno K, Iwaki T. Effects of partial humid heat exposure during different segments of sleep on human sleep stages and body temperature. Physiol Behav. 2005;83(5):759–65.
Matsumoto Y, Uchimura N, Ishida T, Toyomasu K, Kushino N, Hoshiko M, Morimatsu Y, Mori M, Ishitake T. Reliability and validity of the 3 Dimensional Sleep Scale (3DSS)—day workers version—in assessing sleep phase, quality, and quantity. Sangyo Eiseigaku Zasshi. 2014;56(5):128–40.
Matsumoto Y, Uchimura N, Ishida T, Toyomasu K, Morimatsu Y, Mori M, Kushino N, Hoshiko M, Ishitake T. Day workers suffering from a wider range of sleep problems are more likely to experience suicidality. Sleep Biol Rhythms. 2016;14(4):369–76.
Kitamura S, Hida A, Watanabe M, Enomoto M, Aritake-Okada S, Moriguchi Y, Kamei Y, Mishima K. Evening preference is related to the incidence of depressive states independent of sleep–wake conditions. Chronobiol Int. 2010;27(9–10):1797–812.
Yen CF, Ko CH, Yen JY, Cheng CP. The multidimensional correlates associated with short nocturnal sleep duration and subjective insomnia among Taiwanese adolescents. Sleep. 2008;31(11):1515–25.
van Mill JG, Hoogendijk WJ, Vogelzangs N, van Dyck R, Penninx BW. Insomnia and sleep duration in a large cohort of patients with major depressive disorder and anxiety disorders. J Clin Psychiatry. 2010;71(3):239–46.
van Mill JG, Vogelzangs N, van Someren EJ, Hoogendijk WJ, Penninx BW. Sleep duration, but not insomnia, predicts the 2-year course of depressive and anxiety disorders. J Clin Psychiatry. 2014;75(2):119–26.
Matsumoto Y, Uchimura N, Ishida T, Toyomasu K, Kushino N, Hoshiko M, Morimatsu Y, Mori M, Ishitake T. The cut-off point of the 3 Dimensional Sleep Scale (3DSS)—day workers version—based on the Pittsburgh Sleep Quality Index (PSQI). Sangyo Eiseigaku Zasshi. 2015;57(4):140–3.
Benowitz NL, Kuyt F, Jacob P 3rd. Circadian blood nicotine concentrations during cigarette smoking. Clin Pharmacol Ther. 1982;32(6):758–64.
Liu C, Li S, Liu T, Borjigin J, Lin JD. Transcriptional coactivator PGC-1alpha integrates the mammalian clock and energy metabolism. Nature. 2007;447(7143):477–81.
Terazono H, Mutoh T, Yamaguchi S, Kobayashi M, Akiyama M, Udo R, Ohdo S, Okamura H, Shibata S. Adrenergic regulation of clock gene expression in mouse liver. Proc Natl Acad Sci USA. 2003;100(11):6795–800.
Chan JW, Lam SP, Li SX, Yu MW, Chan NY, Zhang J, Wing YK. Eveningness and insomnia: independent risk factors of nonremission in major depressive disorder. Sleep. 2014;37(5):911–7.
Zeitzer JM, Dijk DJ, Kronauer R, Brown E, Czeisler C. Sensitivity of the human circadian pacemaker to nocturnal light: melatonin phase resetting and suppression. J Physiol. 2000;526(Pt 3):695–702.
Okada M, Takayama K, Yanase T. The influences of the intensity of bed-room light on the sleeping process. Kaseigaku Kenkyu. 1981;28(1):58–64.
Van den Bulck J. Adolescent use of mobile phones for calling and for sending text messages after lights out: results from a prospective cohort study with a one-year follow-up. Sleep. 2007;30(9):1220–3.
Chellappa SL, Steiner R, Oelhafen P, Lang D, Gotz T, Krebs J, Cajochen C. Acute exposure to evening blue-enriched light impacts on human sleep. J Sleep Res. 2013;22(5):573–80.
Krahn L, Gordon IA. In bed with a mobile device: are the light levels necessarily too bright for sleep initiation? Sleep. 2013;36:A184 (Abstract supplement).
Acknowledgements
The authors thank the staff and participants of the companies for their important contributions. This work was supported by JSPS KAKENHI (Grant no. 26870777).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
All authors declare that they have no conflicts of interest.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. This study was approved by the Kurume University Ethics Review Board.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
About this article
Cite this article
Matsumoto, Y., Uchimura, N., Ishida, T. et al. The relationship of sleep complaints risk factors with sleep phase, quality, and quantity in Japanese workers. Sleep Biol. Rhythms 15, 291–297 (2017). https://doi.org/10.1007/s41105-017-0110-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s41105-017-0110-1