Abstract
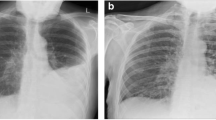
Pleural infection is a millennia-spanning condition that has proved challenging to treat over many years. Fourteen percent of cases of pneumonia are reported to present with a pleural effusion on chest X-ray (CXR), which rises to 44% on ultrasound but many will resolve with prompt antibiotic therapy. To guide treatment, parapneumonic effusions have been separated into distinct categories according to their biochemical, microbiological and radiological characteristics. There is wide variation in causative organisms according to geographical location and healthcare setting. Positive cultures are only obtained in 56% of cases; therefore, empirical antibiotics should provide Gram-positive, Gram-negative and anaerobic cover whilst providing adequate pleural penetrance. With the advent of next-generation sequencing techniques, yields are expected to improve. Complicated parapneumonic effusions and empyema necessitate prompt tube thoracostomy. It is reported that 16–27% treated in this way will fail on this therapy and require some form of escalation. The now seminal Multi-centre Intrapleural Sepsis Trials (MIST) demonstrated the use of combination fibrinolysin and DNase as more effective in the treatment of empyema compared to either agent alone or placebo, and success rates of 90% are reported with this technique. The focus is now on dose adjustments according to the patient’s specific ‘fibrinolytic potential’, in order to deliver personalised therapy. Surgery has remained a cornerstone in the management of pleural infection and is certainly required in late-stage manifestations of the disease. However, its role in early-stage disease and optimal patient selection is being re-explored. A number of adjunct and exploratory therapies are also discussed in this review, including the use of local anaesthetic thoracoscopy, indwelling pleural catheters, intrapleural antibiotics, pleural irrigation and steroid therapy.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Parapneumonic effusions are separated into distinct categories according to their biochemical, microbiological and radiological characteristics. |
It is increasingly recognised there exists heterogeneity within these groups, and there is a paucity of evidence for the optimal first-line intervention, in the form of head-to-head comparator trials. |
The causative organism varies widely according to geographical location and healthcare setting, and positive cultures are achieved in only 56% of cases. This is expected to increase with next-generation sequencing techniques. |
Whilst 16–27% of cases managed with tube thoracostomy are expected to require escalation of therapies, treatment success rates of 90% are now reported in the literature with intrapleural enzyme therapy (IET). |
Future directions will look at delivering personalised therapies according to individual patients’ ‘fibrinolytic potential’ and targeting upstream biochemical pathways. |
Digital Features
This article is published with digital features, including a summary slide, to facilitate understanding of the article. To view digital features for this article go to https://doi.org/10.6084/m9.figshare.13227905.
Introduction
Pleural infection is a disease that has plagued both the ancient and modern world [1, 2]. It has been studied and described by the great and the good, but has afflicted them in equal measure. Sir William Osler (1849–1919), hailed as the father of modern medicine, opted for surgical management of his empyema only to succumb to his illness, whilst ironically, the eminent French surgeon Guillaume Dupuytren (1777–1835) opted for conservative measures and eventually met the same fate [3,4,5]. That we still grapple with some of the same issues our forefathers did serves as a source of both comfort and frustration. Many advances have been made in the management of pleural infection, and in this review, we aim to summarise the evidence to date and outline best practice in the management of empyema in adults. It is important to note that empyema in children is a distinctively different condition from that in adults, and management recommendations for adults do not necessarily apply to children and vice versa.
Definition
‘Pleural infection’ is a stepwise progressive condition, classified into stages, and whilst there is some variation in the classification system between different international guidelines, the principles are largely similar. This is summarised in Table 1 and incorporates pertinent features from each of these guidelines.
Traditionally, it is the presence of pus within the pleural space that earns pleural infection the title of ‘empyema’; however, in the literature, the terms pleural infection, complicated parapneumonic effusion (CPPE) and empyema are used fairly interchangeably, and in clinical practice their management is identical.
It should be borne in mind that pleural fluid biomarkers are simply tests and, like any other, have varying sensitivity, specificity and likelihood ratios. They are not infallible and must be interpreted within the context of the overall clinical picture. Whilst novel pleural fluid markers have been proposed, their discussion is beyond the scope of this review [9,10,11,12,13,14].
Antimicrobials
The cornerstones of treatment in pleural infection is prompt evacuation of the infected collection from the pleural space and initiation of antimicrobial therapy [6]. Antimicrobial therapy should be guided by specific pathogen susceptibility. The bacteriology implicated in pleural infection is distinct from that of pneumonia and serves as further evidence of the two as separate clinical entities and hints at differing mechanisms of transmission (e.g. haematogenous route from oropharyngeal sources) [15, 16].
A recent systematic review has shown that pleural fluid culture is positive in only about 56% of cases and is polymicrobial in 12.9%. Within our own institution, our practice is to inoculate blood culture bottles with pleural fluid to further improve the yield. Menzies et al. demonstrated an increase in yield from 37.7 to 58.5% by adopting such simple measures [17]. There is wide variation in causative organism according to geographical location and the healthcare setting of infection (Table 2). In a recent systematic review encompassing 75 studies and more than 10,000 participants, Staphylococcus aureus (20.7%) appears to have overtaken the Streptococcus viridans group (18%) as the most commonly cultured pathogen globally [18]. Hitherto, Streptococcus milleri, the most common subgroup of S. viridans, was thought to be the commonest isolate [6, 19]. While the tropics and temperate regions had a greater incidence of Gram-positive organisms, subtropical regions had a higher incidence of Gram-negative bacteria. Community-acquired infections were often caused by Gram-positive aerobes (65%), whereas within hospital-acquired settings, Gram-negative aerobes had the larger share (38%). With the advent of next-generation techniques such as 16S ribosomal RNA (rRNA) sequencing and whole-genome sequencing (WGS), we may overcome some of the deficits of standard microscopy and culture techniques. With these techniques, prior antibiotic usage is unlikely to affect yield, polymicrobial infection will be more readily identified, and the impact of fastidious organisms in pleural infection, previously rarely cultured, will be realised [19]. Although this runs the risk of opening up a minefield of interpretation and management decisions, it will likely advance our understanding of the pleural microbiome, in disease and in health.
In culture-negative pleural infections, empirical antimicrobial therapy should be based on local resistance patterns and antimicrobial stewardship policies [18]. The British Thoracic Society (BTS) and American Association for Thoracic Surgery suggest broad-spectrum antibiotics with Gram-positive, Gram-negative and anaerobic cover until culture and sensitivities are available [6, 8]. In pneumococcal infections, anaerobic cover is rarely required; as Maskell et al. demonstrated across 74 such infections, there was not a single instance of anaerobic co-infection [20]. For pleural infection secondary to community-acquired pneumonia, where the risk of methicillin-resistant Staphylococcus aureus (MRSA) or Gram-negative bacteria is low, a second- or third-generation cephalosporin combined with metronidazole or penicillins combined with a β-lactamase inhibitor (e.g. co-amoxiclav) is recommended. Clindamycin is a suitable alternative to metronidazole for anaerobic cover [21]. Additional MRSA cover is recommended in the setting of hospital-acquired infections, as close to 60% of all S. aureus in this setting is likely to be an MRSA [18]. Since the prevalence of Mycoplasma spp. and Legionella spp. in pleural infection is low, routine use of atypical cover is not recommended [6, 20].
The penetration of antibiotics into the pleural space is an area of much debate. In a rabbit model, most antibiotics with the exception of aminoglycosides have demonstrated good penetration into the pleural space [22]. There are no data, however, on the concentration or bioavailability of antibiotics within the human pleural space. Animal studies have shown higher levels of fluoroquinolones in pleural fluid than in blood at 4–12 h after administration, and the presence of clarithromycin in pleural fluid inhibited most empyema-causing organisms [23, 24]. However, the applicability of these findings in humans is unknown. Further research on antibiotic concentrations in human pleural fluid is essential to improving rates of antibiotic failure in pleural infection [22, 25].
The duration of antimicrobial therapy in pleural infection is an evidence-free zone and is largely based on expert opinion and extrapolation from recommendations for the treatment of lung abscess. The recommended duration varies from 2 to 6 weeks, and the authors recommend a minimum of 4 weeks (in total, including intravenous and oral treatment) [26]. Current BTS guidelines recommend switching from intravenous to oral antibiotics when there has been clinical improvement with cessation of pyrexia, resolution of inflammatory markers and radiological improvement [6]. A retrospective study involving 91 patients showed that 3 weeks of antimicrobial therapy was usually adequate to prevent treatment failure [27]. With more definitive treatment options for treating pleural infection with intrapleural enzyme therapies (IET) and surgery, there may be a further argument for shorter-duration antibiotic regimes. The rising importance of antibiotic stewardship highlights the urgency for prospective well-designed trials to define optimal antibiotic duration.
Chest Tube Drainage
The earliest accounts of ‘open thoracic drainage’ date back to the ancient Greeks [28, 29]. Despite the significant risk of mortality as a result of an open pneumothorax, this remained the standard of care for centuries. Although ‘closed tube’ drainage systems had been well described by the German physician Dr. Gotthard Bülau in 1891, they only began to feature more consistently following the ‘Empyema Commission’ during World War I. Coinciding with the Great H1NI influenza pandemic, this resulted in a surge in cases of streptococcal empyema, with a mortality rate of 30% in military hospitals. Through the efforts of Dr. Evarts A. Graham and the commission, the mortality rate was reduced to 3.4% with the adoption of some simple measures as described in Fig. 1 [30].
Through his seminal body of work, Dr. Richard Light and collaborators demonstrated the need for ‘closed tube’ drainage in only those parapneumonic effusions we would now classify as belonging to the ‘fibrinopurulent’ stage [31,32,33]. This case series demonstrated the favourable outlook for uncomplicated parapneumonic effusion (UPPE), which often resolved with antibiotic use alone and has now become the standard of care [6,7,8, 19, 34]. It should however be noted that these large case series have not examined outcomes of UPPE in detail.
It is important to reassess the clinical picture if the patient makes no improvement, and this may require resampling of the pleural fluid. Some patients with an UPPE will progress to a CPPE despite prompt antimicrobial use; a proposed explanation is the heterogeneous nature of pleural fluid within loculated collections, and sampling from one locule may not be representative of the remainder [35]. Therefore, tube drainage for multi-loculated collections is also recommended, irrespective of pleural fluid characteristics [6, 7].
It is worth discussing the role of therapeutic aspiration in pleural infection. This was used extensively in the series by Light et al. as a combined diagnostic/therapeutic intervention and for effusion recurrence. Pragmatically, the use of large-volume aspiration as part of the initial diagnostic procedure for stage I infection would seem reasonable, particularly with large effusions where it is likely to provide symptomatic relief. Interestingly, Porcel et al. demonstrated in their retrospective case series of 641 patients that effusions that occupied one-half or more of the hemithorax strongly correlated with a CPPE and were likely to need tube drainage, independent of other pleural fluid characteristics [36]. Repeated thoracocentesis has been described in some case series and a single prospective observational study with reasonable rates of success (76% success, median 3 procedures), but prospective randomised controlled trial (RCT) data is lacking [37,38,39,40,41]. With the advent of small-bore catheters and minimally invasive techniques, tube drainage has largely superseded this technique, and most experts would agree that the risk of repeated entry into the pleural space outweighs that of a single, more definitive intervention [42]. Therefore, when dealing with a large parapneumonic effusion, tube drainage is recommended over multiple aspirations [6, 7, 36]. As we move into the era of ambulatory management of many conditions, spurred by the current COVID-19 pandemic, this is an area ripe for research. Indeed, there is a currently recruiting trial addressing this potential treatment option in the UK (ISRCTN84674413) [43].
Following on from this, the optimal size of intrapleural catheter in treating empyema is yet to be defined. It remains a topic of great interest and is regularly a source of debate at conferences and in editorials [44]. Medical dogma has suggested larger-bore drains to be more efficacious in managing empyema, but a number of retrospective case series have demonstrated success with small-bore drains [45,46,47,48,49,50,51,52,53,54,55]. The only study comparing differences in outcome between small- and large-bore drains in a prospectively recruited cohort comes from our unit [56]. This retrospective analysis of the MIST-1 trial data included 405 patients and demonstrated no difference in clinical outcomes by drain size (mortality or the need for surgery) or in adverse event rates, with a drain displacement rate of 17–23%. Importantly, this study noted a marked difference in pain scores; large-bore drains (> 14F), particularly those inserted via blunt dissection, were associated with a significantly higher pain score compared to small-bore drains (≤ 14F) [56, 57]. Furthermore, in subgroup analysis of the MIST-2 trial data, no difference in treatment effect was noted between large- and small-bore drains [58]. Though prospective data on drain outcomes specific to empyema are lacking, estimates from case series suggest drain occlusion rates as high as 63% and that regular saline flushes can mitigate this [8, 55, 59, 60]. This concept was taken further in the single-centre RCT ‘Pleural Irrigation Trial’ (PIT), which saw improvements in the volumes of pleural collection on CT and referral to surgery in the intervention arm receiving 250 ml 0.9% sodium chloride three times a day.
Intrapleural Enzyme Therapy (IET)
The authors prefer the term IET (rather than intrapleural fibrinolytic therapy, IPFT) as a catch-all term, and such treatment is a relatively old concept. It has long been recognised that as infected pleural fluid became more frankly purulent, it had a tendency to loculate and become more viscous, thereby making drainage difficult [61]. Indeed current evidence suggests that some 16–27% of patients treated with antibiotics and tube drainage alone will go on to require further surgical intervention to treat their pleural infection, whilst older studies quote even higher rates [57, 58, 62, 63].
Tillet and Sherry, through their pioneering work 70 years ago, recognised that it was the presence of fibrin and ‘deoxyribose nucleoprotein’ (DNA) that contributed to the purulence and viscosity of post-haemothorax pleural infection. Their attempts to overcome this problem and increase the effectiveness of tube drainage through the use of intrapleural streptokinase and deoxyribonuclease (DNase) paved the way for wider use of these agents [64,65,66].
Although the duo demonstrated in 1949 that it was the combined effects of both streptokinase and DNase that improved drainage, the latter fell out of use particularly in North America, perhaps borne out of concerns surrounding allergic reactions to the combined preparation, originally extracted from haemolytic group C streptococci [61, 64].
IPFT as sole therapy has been studied extensively through case series and RCTs, but perhaps the most robust answer comes from a Cochrane review by Altmann et al. Across 10 RCTs encompassing 993 participants, there was no difference in mortality observed between the IPFT and placebo group, but a reduction in surgical intervention and treatment failure was seen in the IPFT arm (OR 0.37, 95% CI 0.21–0.68 and 0.16, 95% CI 0.05–0.58, respectively). However, in sensitivity analysis, removing studies at high risk of bias eliminated these benefits. Importantly, the largest study (MIST-1: streptokinase vs placebo, 427 participants), also deemed to be at low risk of bias, was discordant with these findings [67]. It is important to note that the studies analysed in this latest systematic review represent both a heterogeneous population (MIST-1 recruited all patients with a diagnosis of pleural infection, whilst others specified patients with radiological evidence of loculation or failure to progress with tube drainage) and heterogeneous measured outcomes [57, 58, 62, 63, 68,69,70,71,72,73,74,75].
Adding further to the discussion came MIST-2 (210 participants), which demonstrated outcome benefit, measured through radiological clearance, surgical referral and length of stay when comparing combination tissue plasminogen activator (t-PA) and DNase to placebo and, importantly, to either individual agent alone [58]. Though an oversimplification, it is proposed that IPFT acts to disrupt the fibrin-rich adhesions via the activation of plasminogen and may have something of a lavage effect by stimulating pleural fluid production, whilst DNase reduces pleural fluid viscosity through the breakdown of extracellular DNA and biofilm formation. It is their synergistic action that results in better drainage and resolution of pleural infection [66, 76,77,78,79,80,81]. These findings build on the earlier work by Tillet and Sherry but also go some way in confirming other proof-of-concept studies [61, 64, 82, 83]. This has now become the standard of care for non-draining pleural infection in many centres, and there is an increasing body of evidence to demonstrate both efficacy, with treatment success rates of 90%, and safety, with an adverse event bleeding rate of < 5% [84,85,86,87,88]. Importantly, many of these subsequent studies have successfully incorporated their own dose adjustment regimes, highlighting the potential for precision-guided personalised medicine in treating pleural infection (Fig. 2).
The fibrinolytic pathways involved in relation to IET therapies and some novel therapeutic targets (in green are some currently developed therapies: PAI-1-neutralising antibodies, scuPA (also known as LTI-01) [89, 93,94,95]. PAI plasminogen activator inhibitor, scuPA single-chain urokinase plasminogen activator, tPA tissue plasminogen activator, LTA lipoteichoic acid
The development of IET regimes has occurred outside the usual drug development cycles observed in industry-led trials, and therefore much of the pharmacological insight a phased development process produces and that which precision medicine hinges upon has eluded us until recently [76, 89]. It is increasingly recognised that pleural infection is a form of tissue injury with subsequent activation of the clotting cascade, and understanding the delicate balance of the coagulation and fibrinolysin pathway, and by extension the ‘fibrinolytic potential’, is essential in advancing management [78, 79, 89,90,91]. Figure 2 describes some of these pathways and some novel therapeutic targets, one of which has a phase II study planned (NCT04159831) [92].
Surgery
Surgery has long been recognised as a cornerstone in the management of pleural infection, and this is reflected in all major society guidelines. Its precise role remains unclear, which gives rise to variation in the recommendations, with much of the debate revolving around patient selection [6,7,8, 96]. Some guidelines suggest all cases of empyema in stage II or greater be offered surgical management due to greater rates of treatment success and reduced length of hospital stay [96,97,98,99]. This fails to recognise some of the recent advances made in IET and the impressive rates of treatment success across a spectrum of empyema stages, with reports nearing 90% in expert centres [58, 84,85,86, 88]. The truth most likely resides somewhere in the middle, and the fairly crude separation of the stages of empyema into I, II and III in determining optimal first-line therapy runs the risk of ignoring important considerations; these are not always binary categories; there exists a spectrum of abnormality, and other differentiators also play a role [100]. The old adage that surgery be reserved for those that fail conventional medical therapy is seemingly intuitive. Despite this, a large retrospective population-based observation study demonstrated much higher levels of mortality for patients managed non-operatively, even after adjusting for differences in age and comorbidity (11.1% 30-day mortality vs 3.3%), and this finding is supported by other retrospective studies [101,102,103]. What is clear, however, is the distinct lack of head-to-head, prospective data to settle this debate [19, 26]. Even a recent Cochrane review into the question could only produce 8 trials across 391 participants, of which 6 trials were within a paediatric population. Their conclusion of no statistical differences in mortality between the surgically and non-surgically managed groups must therefore be interpreted with caution, given paediatric empyema is a clinically distinct entity with very different outcomes and microbiology [104]. Offering early aggressive treatments such as surgery, with the risks this entails, needs to be balanced against the risks associated with empyema in the first instance. The RAPID score was derived from the MIST-1 cohort and then validated in the MIST-2 cohort. The score is based on baseline serum urea (renal), patient age (age), pleural fluid purulence (purulence), infection source (community- vs healthcare-acquired infection) and serum albumin (dietary), and was shown to be independently associated with mortality at 3 months [105]. Now this score has been validated prospectively in the Pleural Infection Longitudinal Outcome (PILOT) study. Across 546 patients, the PILOT study demonstrated that low-risk patients (RAPID score 0–2) had a 3-month mortality of 2.3%, medium-risk (RAPID score 3–4) 9.2% mortality and high-risk (RAPID score 5–7) 29.3% mortality [106]. It is hoped that through the use of the RAPID score, a more nuanced approach can be taken in risk-stratifying patients and thereby informing clinicians of the optimal approaches in management.
Conceptually, surgical options for the management of empyema centre on debridement and evacuation of the infected material from the pleural space. Where the visceral pleura has developed a thickened rind, a decortication is also required to allow for lung re-expansion, crucial for maintaining a sterile pleural space thereafter. These procedures can be performed through a less invasive video-assisted thoracoscopic surgical (VATS) approach or a more invasive open thoracotomy approach [100, 107]. In comparing the two approaches, VATS has certainly been shown to have more favourable rates of complications, morbidity, mortality (in-hospital 5.7% vs 10.6%) and length of hospital stay (5 vs 8 days) whilst retaining similar efficacy as that of the open approach [96, 99, 101, 108, 109]. Whilst it would therefore seem obvious to opt for a VATS approach, and there is a clear trend towards this over the years, the reality is not quite so straightforward. There are technical difficulties in a VATS approach in late-stage empyema; dense adhesions can prevent insertion of the thoracoscope, or complete decortication may not be possible due to the location and depth of peel formation [110]. In such situations, there is a need to convert to an open thoracotomy approach, and conversion rates as high as 55% have been reported in the literature [111]. More modern studies still have a conversion rate of around 15% [100]. Inability to tolerate single-lung ventilation or severe coagulopathy are also considered contraindications to a VATS approach. Although conversion is associated with an increase in intra-operative time, it is not clear whether this has an effect on outcome [112]. Some experts argue that a thoracoscopic view of the pleural cavity via VATS may indeed be a necessary step in determining the need for an open approach [110]. The role of non-invasive investigations such as computed tomography (CT) in making these decisions has had mixed results [113,114,115]. What is clear in the literature, however, is that delays in surgical intervention are consistently the strongest predictor of the need for conversion [116, 117]. Therefore, offering surgical intervention only in cases of failed medical therapy, with its subsequent delays, or in late-stage empyema and thereby precluding patients from receiving the gold-standard surgical intervention, would seem something of a paradox [19, 118]. It is this paradox that experts are now grappling with and that has set the stage for head-to-head trials of early VATS vs early IET vs standard care with the MIST-3 feasibility study (ISRCTN18192121) [119].
Alternative Therapies and Future Directions
It is worth briefly mentioning other therapies that are either currently in use or on the horizon. Local anaesthetic thoracoscopy (LAT) has been used in the management of pleural infection, but currently sits outside the recommended guidelines [120]. It has been suggested that LAT has utility in clearing septations and allows for targeted drain insertion, although it seems unlikely to be of use in the advanced stages of empyema. In the hands of experienced operators, excellent outcomes have been reported in case series, but LAT has never been studied in head-to-head comparator trials. The ‘Studying Pleuroscopy in Routine Pleural Infection Treatment’ (SPIRIT) trial (ISRCTN98460319) was a feasibility study and is due to publish results later this year [121].
A chronically infected pleural space with a trapped lung is a challenging condition. In particularly advanced cases where patients are not fit enough to undergo decortication, the only surgical options may be limited to thoracoplasty or open window thoracostomy [107]. In the modern era, these techniques report reasonable rates of success (75–95%) and mortality (4%), aided further by the use of vacuum-assisted closure (VAC) techniques [100]. However, many patients are often not fit enough to undergo surgical intervention or have associated co-morbidity (e.g. malignant pleural disease) that precludes such treatments. In such cases, prolonged antibiotic therapy and the use of an indwelling pleural catheter (IPC) have been described in limited case reports [122]. It is important to note that this approach has not been validated through trial data, nor is it likely to be, given the small numbers of such patients. Broadly speaking, pleural infection remains a contraindication to IPC insertion and a complication thereof [26]. However, this treatment approach offers an alternative to repeated tube thoracostomy and may facilitate a more holistic approach to caring for patients on a palliative pathway.
Intrapleural antibiotic therapy has often been proposed as a way of overcoming the poor pleural penetrance seen with a number of antibiotic classes. A recent review found little evidence to support the routine use of these therapies in post-pneumonic pleural infection, although there is more evidence for its use in post-pneumonectomy infections [80]. A number of antibiotic-eluting drainage catheters are now commercially available, and a recent study was able to demonstrate sustained release of bactericidal concentrations of penicillin within the pleural space compared to an intravenous regime in healthy rabbits [123]. What effect this technique has in animal models of empyema remains to be seen before human studies can be considered.
Finally, whilst many of the treatment modalities described in this review have centred on optimal evacuation of infected pleural fluid, there is a body of work exploring methods to ‘switch off the leaky faucet’ [76]. Key inflammatory mediators [NF-κB, CCL2/MCP-1, TNF, interleukins, osteopontin (OPN)] have been identified and there is clear overlap with the processes involved in malignant pleural effusion formation. Whilst this work is still in its infancy and targeted pharmacotherapy is not yet on the horizon, it is thought that systemic steroids may attenuate some of these pathways. Its safety in pneumonia has already been demonstrated as well as a signal towards clinical efficacy [124, 125]. With the aim of combatting the exaggerated inflammatory cascade seen in pleural infection, the ‘Steroid therapy and outcome of parapneumonic pleural effusions’ (STOPPE) trial (ACTRN 12618000947202), is currently recruiting patients into a pilot multi-centre RCT, comparing 48 h of intravenous dexamethasone to placebo [126].
Conclusion
The management of pleural infection has come a long way from ancient descriptions and has enjoyed something of a renaissance in the past decade. The key areas the next decade hold include identification and refinement of targeted therapies in both early- and late-stage disease processes and finally establishing optimal first-line therapies.
References
Breasted JH. Case Forty | XIII 12–17 | A wound in the breast. In: The Edwin Smith Surgical Papyrus, Volume 1: Hieroglyphic Transliteration, Translation, and Commentary [Internet]. The Oriental Institute of the University of Chicago; [cited 2020 May 6]. p. 369–73. https://oi.uchicago.edu/research/publications/oip/edwin-smith-surgical-papyrus-volume-1-hieroglyphic-transliteration.
Hippocrates, Adams F. Preliminary Discourses (sect II) Hippocratic Treatises. In: The genuine works of Hippocrates; [Internet]. New York, W. Wood and company; 1886 [cited 2020 May 22]. p. 88–93. http://archive.org/details/genuineworkship02hippgoog.
Barondess JA. A case of empyema: notes on the last illness of Sir William Osler. Trans Am Clin Climatol Assoc. 1975;86:59–72.
Gregory P, Rahman NM, Lee YCG. Osler Centenary Papers: management of pleural infection: Osler’s final illness and recent advances. Postgrad Med J. 2019;95(1130):656–9.
Tassi G, Marchetti G. Pleural diseases: historic perspective. In: Light RW, Lee YCG, editors. Textbook of pleural diseases. 3rd ed. Boca Raton: CRC Press; 2016. p. 1–9.
Davies HE, Davies RJ, Davies CWH. Management of pleural infection in adults: British Thoracic Society Pleural Disease Guideline 2010. In: BTS Pleural Disease Guideline 2010. II. Thorax; 2010. p. 241–53.
Colice GL, Curtis A, Deslauriers J, Heffner J, Light R, Littenberg B, et al. Medical and surgical treatment of parapneumonic effusions: an evidence-based guideline. Chest. 2000;118(4):1158–71.
Shen KR, Bribriesco A, Crabtree T, Denlinger C, Eby J, Eiken P, et al. The American Association for Thoracic Surgery consensus guidelines for the management of empyema. J Thorac Cardiovasc Surg. 2017;153(6):129–46.
Porcel JM. Distinguishing complicated from uncomplicated parapneumonic effusions. Curr Opin Pulm Med. 2015;21(4):346–51.
Heffner JE, Brown LK, Barbieri C, DeLeo JM. Pleural fluid chemical analysis in parapneumonic effusions: a meta-analysis. Am J Respir Crit Care Med. 1995;151(6):1700–8.
Arnold DT, Hamilton FW, Elvers KT, Frankland SW, Zahan-Evans N, Patole S, et al. Pleural fluid suPAR levels predict the need for invasive management in parapneumonic effusions. Am J Respir Crit Care Med. 2020;201(12):1545–53.
Dixon G, Lama-Lopez A, Bintcliffe OJ, Morley AJ, Hooper CE, Maskell NA. The role of serum procalcitonin in establishing the diagnosis and prognosis of pleural infection. Respir Res. 2017;18(1):30.
Fitzgerald DB, Leong SL, Budgeon CA, Murray K, Rosenstengal A, Smith NA, et al. Relationship of pleural fluid pH and glucose: a multi-centre study of 2971 cases. J Thorac Dis. 2019;11(1):123–30.
Jiménez Castro D, Díaz Nuevo G, Sueiro A, Muriel A, Pérez-Rodríguez E, Light RW. Pleural fluid parameters identifying complicated parapneumonic effusions. Respiration. 2005;72(4):357–64.
Corcoran JP, Wrightson JM, Belcher E, DeCamp MM, Feller-Kopman D, Rahman NM. Pleural infection: past, present, and future directions. Lancet Respir Med. 2015;3(7):563–77.
Dyrhovden R, Nygaard RM, Patel R, Ulvestad E, Kommedal Ø. The bacterial aetiology of pleural empyema: a descriptive and comparative metagenomic study. Clin Microbiol Infect. 2019;25(8):981–6.
Menzies SM, Rahman NM, Wrightson JM, Davies HE, Shorten R, Gillespie SH, et al. Blood culture bottle culture of pleural fluid in pleural infection. Thorax. 2011;66(8):658–62.
Hassan M, Cargill T, Harriss E, Asciak R, Mercer RM, Bedawi EO, et al. The microbiology of pleural infection in adults: a systematic review. Eur Respir J. 2019;54(3):1900542.
Bedawi EO, Rahman NM. Pleural infection: Moving from treatment to prevention. In: Maskell NA, Laursen CB, Lee YCG, et al, editors Pleural Disease (ERS Monograph) [Internet]. Sheffield: European Respiratory Society; 2020 [cited 2020 May 6]. p. 155–71. http://public.eblib.com/choice/PublicFullRecord.aspx?p=6181621.
Maskell NA, Batt S, Hedley EL, Davies CWH, Gillespie SH, Davies RJO. The bacteriology of pleural infection by genetic and standard methods and its mortality significance. Am J Respir Crit Care Med. 2006;174(7):817–23.
Brook I, Wexler HM, Goldstein EJC. Antianaerobic antimicrobials: spectrum and susceptibility testing. Clin Microbiol Rev. 2013;26(3):526–46.
Teixeira LR, Sasse SA, Villarino MA, Nguyen T, Mulligan ME, Light RW. Antibiotic levels in empyemic pleural fluid. Chest. 2000;117(6):1734–9.
Liapakis IE. Penetration of newer quinolones in the empyema fluid. Eur Respir J. 2004;24(3):466–70.
Liapakis IE, Light RW, Pitiakoudis MS, Karayiannakis AJ, Giamarellos-Bourboulis EJ, Ismailos G, et al. Penetration of clarithromycin in experimental pleural empyema model fluid. Respiration. 2005;72(3):296–300.
Tobin CL, Lee YCG. Pleural infection: what we need to know but don’t. Curr Opin Pulm Med. 2012;18(4):321–5.
Bedawi EO, George V, Rahman NM. A new approach to pleural infection: let it be? Curr Pulmonol Rep. 2019;8(3):112–22.
Birkenkamp K, O’Horo JC, Kashyap R, Kloesel B, Lahr BD, Daniels CE, et al. Empyema management: a cohort study evaluating antimicrobial therapy. J Infect. 2016;72(5):537–43.
Christopoulou-Aletra H, Papavramidou N. “Empyemas” of the thoracic cavity in the Hippocratic Corpus. Ann Thorac Surg. 2008;85(3):1132–4.
Walcott-Sapp S, Sukumar M. A History of Thoracic Drainage: From Ancient Greeks to Wound Sucking Drummers to Digital Monitoring. [cited 2020 May 22]. https://www.ctsnet.org/article/history-thoracic-drainage-ancient-greeks-wound-sucking-drummers-digital-monitoring.
Graham EA. Some fundamental considerations in the treatment of empyema thoracis. St. Louis: The C.V. Mosby Co; 1925.
Light RW. A new classification of parapneumonic effusions and empyema. Chest. 1995;108(2):299–301.
Light RW, MacGregor MI, Ball WC, Luchsinger PC. Diagnostic significance of pleural fluid pH and PCO2. Chest. 1973;64(5):591–6.
Light RW. Parapneumonic effusions and empyema. Proc Am Thorac Soc. 2006;3(1):75–80.
Potts DE, Levin DC, Sahn SA. Pleural fluid pH in parapneumonic effusions. Chest. 1976;70(3):328–31.
Maskell NA, Gleeson FV, Darby M, Davies RJO. Diagnostically significant variations in pleural fluid pH in loculated parapneumonic effusions. Chest. 2004;126(6):2022–4.
Porcel JM, Valencia H, Bielsa S. Factors influencing pleural drainage in parapneumonic effusions. Rev Clín Esp Engl Ed. 2016;216(7):361–6.
Porcel JM. Minimally invasive treatment of complicated parapneumonic effusions and empyemas in adults. Clin Respir J. 2018;12(4):1361–6.
Storm HK, Krasnik M, Bang K, Frimodt-Moller N. Treatment of pleural empyema secondary to pneumonia: thoracocentesis regimen versus tube drainage. Thorax. 1992;47(10):821–4.
Letheulle J, Tattevin P, Saunders L, Kerjouan M, Léna H, Desrues B, et al. Iterative thoracentesis as first-line treatment of complicated parapneumonic effusion. PLoS ONE. 2014;9(1):e84788.
Simmers TA, Jie C, Sie B. Minimally invasive treatment of thoracic empyema. Thorac Cardiovasc Surg. 1999;47(2):77–81. https://doi.org/10.1055/s-2007-1013115.
Ferguson AD, Prescott RJ, Selkon JB, Watson D, Swinburn CR. The clinical course and management of thoracic empyema. QJM. 1996;89(4):285–90.
Heffner JE, Klein JS, Hampson C. Interventional management of pleural infections. Chest. 2009;136(4):1148–59.
Arnold D. Comparing aspiration to chest tube drainage for treating infected fluid around the lung [Internet]. ISRCTN registry; 2019 Apr [cited 2020 Aug 29]. Report No.: ISRCTN84674413. http://www.isrctn.com/ISRCTN84674413.
Light RW. Pleural controversy: optimal chest tube size for drainage. Respirology. 2011;16(2):244–8.
Klein JS, Schultz S, Heffner JE. Interventional radiology of the chest: image-guided percutaneous drainage of pleural effusions, lung abscess, and pneumothorax. AJR Am J Roentgenol. 1995;164(3):581–8.
Merriam MA, Cronan JJ, Dorfman GS, Lambiase RE, Haas RA. Radiographically guided percutaneous catheter drainage of pleural fluid collections. AJR Am J Roentgenol. 1988;151(6):1113–6.
Ulmer JL, Choplin RH, Reed JC. Image-guided catheter drainage of the infected pleural space. J Thorac Imaging. 1991;6(4):65–73.
van Sonnenberg E, Nakamoto SK, Mueller PR, Casola G, Neff CC, Friedman PJ, et al. CT- and ultrasound-guided catheter drainage of empyemas after chest-tube failure. Radiology. 1984;151(2):349–53.
Crouch JD, Keagy BA, Delany DJ. ‘Pigtail’ catheter drainage in thoracic surgery. Am Rev Respir Dis. 1987;136(1):174–5.
Hunnam GR, Flower CD. Radiologically-guided percutaneous catheter drainage of empyemas. Clin Radiol. 1988;39(2):121–6.
O’Moore PV, Mueller PR, Simeone JF, Saini S, Butch RJ, Hahn PF, et al. Sonographic guidance in diagnostic and therapeutic interventions in the pleural space. AJR Am J Roentgenol. 1987;149(1):1–5.
Silverman SG, Mueller PR, Saini S, Hahn PF, Simeone JF, Forman BH, et al. Thoracic empyema: management with image-guided catheter drainage. Radiology. 1988;169(1):5–9.
Stavas J, vanSonnenberg E, Casola G, Wittich GR. Percutaneous drainage of infected and noninfected thoracic fluid collections. J Thorac Imaging. 1987;2(3):80–7.
Keeling AN, Leong S, Logan PM, Lee MJ. Empyema and effusion: outcome of image-guided small-bore catheter drainage. Cardiovasc Intervent Radiol. 2008;31(1):135–41.
Horsley A, Jones L, White J, Henry M. Efficacy and complications of small-bore, wire-guided chest drains. Chest. 2006;130(6):1857–63.
Rahman NM, Maskell NA, Davies CWH, Hedley EL, Nunn AJ, Gleeson FV, et al. The relationship between chest tube size and clinical outcome in pleural infection. Chest. 2010;137(3):536–43.
Maskell NA, Gleeson FV, Woodhead MA, Davies RJO. UK controlled trial of intrapleural streptokinase for pleural infection. N Engl J Med. 2005;352(9):865–74.
Rahman NM, Phil D, Maskell NA, Teoh R, Peckham D, Kinnear W, et al. Intrapleural use of tissue plasminogen activator and DNase in pleural infection. N Engl J Med. 2011;365(6):518–26.
Cafarotti S, Dall’Armi V, Cusumano G, Margaritora S, Meacci E, Lococo F, et al. Small-bore wire-guided chest drains: safety, tolerability, and effectiveness in pneumothorax, malignant effusions, and pleural empyema. J Thorac Cardiovasc Surg. 2011;141(3):683–7.
Davies HE, Merchant S, McGOWN A. A study of the complications of small bore ‘Seldinger’ intercostal chest drains. Respirology. 2008;13(4):603–7.
Simpson G, Roomes D, Heron M. Effects of streptokinase and deoxyribonuclease on viscosity of human surgical and empyema pus. Chest. 2000;117(6):1728–33.
Bouros D, Schiza S, Tzanakis N, Chalkiadakis G, Drositis J, Siafakas N. Intrapleural urokinase versus normal saline in the treatment of complicated parapneumonic effusions and empyema: a randomized, double-blind study. Am J Respir Crit Care Med. 1999;159(1):37–42.
Davies RJ, Traill ZC, Gleeson FV. Randomised controlled trial of intrapleural streptokinase in community acquired pleural infection. Thorax. 1997;52(5):416–21.
Tillett WS, Sherry S. The effect in patients of streptococcal fibrinolysin (streptokinase) and streptococcal desoxyribonuclease on fibrinous, purulent, and sanguinous pleural exudations. J Clin Investig. 1949;28(1):173–90.
Tillett WS, Sherry S, Christensen LR. Streptococcal desoxyribonuclease: significance in lysis of purulent exudates and production by strains of hemolytic Streptococci. Exp Biol Med. 1948;68(1):184–8.
Sherry S, Tillett WS, Christensen LR. Presence and significance of desoxyribose nucleoprotein in the purulent pleural exudates of patients. Exp Biol Med. 1948;68(1):179–84.
Altmann ES, Crossingham I, Wilson S, Davies HR. Intra-pleural fibrinolytic therapy versus placebo, or a different fibrinolytic agent, in the treatment of adult parapneumonic effusions and empyema. Cochrane Airways Group, editor. Cochrane Database Syst Rev [Internet]. 2019 Oct 30 [cited 2020 Apr 23]. https://doi.org/10.1002/14651858.CD002312.pub4.
Alemán C, Porcel JM, Alegre J, Ruiz E, Bielsa S, Andreu J, et al. Intrapleural fibrinolysis with urokinase versus alteplase in complicated parapneumonic pleural effusions and empyemas: a prospective randomized study. Lung. 2015;193(6):993–1000.
Diacon AH, Theron J, Schuurmans MM, Van de Wal BW, Bolliger CT. Intrapleural streptokinase for empyema and complicated parapneumonic effusions. Am J Respir Crit Care Med. 2004;170(1):49–53.
Bouros D, Schiza S, Patsourakis G, Chalkiadakis G, Panagou P, Siafakas NM. Intrapleural streptokinase versus urokinase in the treatment of complicated parapneumonic effusions: a prospective, double-blind study. Am J Respir Crit Care Med. 1997;155(1):291–5.
Misthos P, Sepsas E, Konstantinou M, Athanassiadi K, Skottis I, Lioulias A. Early use of intrapleural fibrinolytics in the management of postpneumonic empyema: a prospective study. Eur J Cardiothorac Surg. 2005;28(4):599–603.
Thommi G, Shehan JC, Robison KL, Christensen M, Backemeyer LA, McLeay MT. A double blind randomized cross over trial comparing rate of decortication and efficacy of intrapleural instillation of alteplase vs placebo in patients with empyemas and complicated parapneumonic effusions. Respir Med. 2012;106(5):716–23.
Tuncozgur B, Ustunsoy H, Sivrikoz MC, Dikensoy O, Topal M, Sanli M, et al. Intrapleural urokinase in the management of parapneumonic empyema: a randomised controlled trial. Int J Clin Pract. 2001;55(10):658–60.
Lin J-C, Zhang C-R, Xu W-M, Li M, Cui W-L. Effectiveness and safety of intrapleural tissue plasminogen activator in the prevention of pleural thickening and loculated effusions by infective pleurisy. Int J Infect Dis. 2011;15:S104–5.
Prasad B, Bhattacharyya D, Luthra M, Mathur A. Management of empyema thoracis with pleural pigtail drainage and intrapleural thrombolytic therapy. In: C44 Pleural Disease II—Chest Tubes, Management, Pathophysiology [Internet]. American Thoracic Society; 2009 [cited 2020 Jun 27]. p. A4486. https://doi.org/10.1164/ajrccm-conference.2009.179.1_MeetingAbstracts.A4486.
Lee YCG, Idell S, Stathopoulos GT. Translational research in pleural infection and beyond. Chest. 2016;150(6):1361–70.
Tucker T, Idell S. Plasminogen–plasmin system in the pathogenesis and treatment of lung and pleural injury. Semin Thromb Hemost. 2013;39(4):373–81.
Idell S. The pathogenesis of pleural space loculation and fibrosis. Curr Opin Pulm Med. 2008;14(4):310–5.
Idell S, Girard W, Koenig KB, McLarty J, Fair DS. Abnormalities of pathways of fibrin turnover in the human pleural space. Am Rev Respir Dis. 1991;144(1):187–94.
Bedawi EO, Hassan M, McCracken D, Rahman NM. Pleural infection: a closer look at the etiopathogenesis, microbiology and role of antibiotics. Expert Rev Respir Med. 2019;13(4):337–47.
Lansley SM, Cheah HM, Varano Della Vergiliana JF, Chakera A, Lee YCG. Tissue plasminogen activator potently stimulates pleural effusion via a monocyte chemotactic protein-1-dependent mechanism. Am J Respir Cell Mol Biol. 2015;53(1):105–12.
Zhu Z, Hawthorne ML, Guo Y, Drake W, Bilaceroglu S, Misra HL, et al. Tissue plasminogen activator combined with human recombinant deoxyribonuclease is effective therapy for empyema in a rabbit model. Chest. 2006;129(6):1577–83.
Light RW, Nguyen T, Mulligan ME, Sasse SA. The in vitro efficacy of varidase versus streptokinase or urokinase for liquefying thick purulent exudative material from loculated empyema. Lung. 2000;178(1):13–8.
Piccolo F, Pitman N, Bhatnagar R, Popowicz N, Smith NA, Brockway B, et al. Intrapleural tissue plasminogen activator and deoxyribonuclease for pleural infection: an effective and safe alternative to surgery. Ann Am Thorac Soc. 2014;11(9):1419–25.
Popowicz N, Bintcliffe O, De Fonseka D, Blyth KG, Smith NA, Piccolo F, et al. Dose de-escalation of intrapleural tissue plasminogen activator therapy for pleural infection. The Alteplase dose assessment for pleural infection therapy project. Ann Am Thorac Soc. 2017;14(6):929–36.
Mehta H, Biswas A, Penley A, Jantz M. Utilizing once daily use of tissue plasminogen activator (TPA) and deoxyribonuclease (Dnase) For management of intrapleural sepsis. Am J Respir Crit Care Med. 2016;193.
McClune JR, Wilshire CL, Gorden JA, Louie BE, Farviar AS, Stefanski MJ, et al. Safety and efficacy of intrapleural tissue plasminogen activator and DNase during extended use in complicated pleural space infections. Can Respir J. 2016;2016:1–6.
Majid A, Kheir F, Folch A, Fernandez-Bussy S, Chatterji S, Maskey A, et al. Concurrent intrapleural instillation of tissue plasminogen activator and DNase for pleural infection: a single-center experience. Ann Am Thorac Soc. 2016;13(9):1512–8.
Idell S, Florova G, Shetty S, Tucker T, Idell R, Koenig K, et al. Precision-guided, personalized intrapleural fibrinolytic therapy for empyema and complicated parapneumonic pleural effusions: the case for the fibrinolytic potential. Clin Pulm Med. 2017;24(4):163–9.
Komissarov AA, Florova G, Azghani AO, Buchanan A, Boren J, Allen T, et al. Dose dependency of outcomes of intrapleural fibrinolytic therapy in new rabbit empyema models. Am J Physiol Lung Cell Mol Physiol. 2016;311:389–99.
Komissarov AA, Florova G, Schaefer C, Rahman NM, Lee YCG, Idell S. Pleural Fluids Collected During The Second Multicenter Intrapleural Sepsis Trial (MIST-2) demonstrate highly variable fibrinolytic potential prior to the treatment and endogenous fibrinolytic activity depletion during intrapleural fibrinolytic therapy. In: Am J Respir Crit Care Med. Pennsylvania Convention Center; 2013.
Lung Therapeutics, Inc. A phase 2, randomized, placebo-controlled, double-blind, dose-ranging study evaluating LTI-01 (single-chain urokinase plasminogen activator, scuPA) in patients with infected, non-draining pleural effusions [Internet]. clinicaltrials.gov; 2020 Jun [cited 2020 Jun 29]. Report No.: NCT04159831. https://clinicaltrials.gov/ct2/show/NCT04159831.
Florova G, Azghani AO, Karandashova S, Schaefer C, Yarovoi SV, Declerck PJ, et al. Targeting plasminogen activator inhibitor-1 in tetracycline-induced pleural injury in rabbits. Am J Physiol Lung Cell Mol Physiol. 2018;314(1):L54–68.
Beckert L, Brockway B, Simpson G, Southcott AM, Lee YCG, Rahman N, et al. Phase I trial of the single-chain urokinase intrapleural LTI-01 in complicated parapneumonic effusions or empyema. JCI Insight. 2019;4(10):e127470.
Lee K-L, Chen W-L, Chen R-J, Lai KS, Chung C-L. Lipoteichoic acid upregulates plasminogen activator inhibitor-1 expression in parapneumonic effusions: LTA upregulates PAI-1 expression in PPE. Respirology. 2018;23(1):89–95.
Scarci M, Abah U, Solli P, Page A, Waller D, van Schil P, et al. EACTS expert consensus statement for surgical management of pleural empyema. Eur J Cardiothorac Surg. 2015;48(5):642–53.
Muhammad MIA. Management of complicated parapneumonic effusion and empyema using different treatment modalities. Asian Cardiovasc Thorac Ann. 2012;20(2):177–81.
Bilgin M, Akcali Y, Oguzkaya F. Benefits of early aggressive management of empyema thoracis. ANZ J Surg. 2006;76(3):120–2.
Marks DJB, Fisk MD, Koo CY, Pavlou M, Peck L, Lee SF, et al. Thoracic empyema: a 12-year study from a UK Tertiary Cardiothoracic Referral Centre. PLoS ONE. 2012;7(1):e30074.
Belcher E, Edwards JG. The role of surgery. In: In: Maskell NA, Laursen CB, Lee YCG, et al, editors Pleural Disease (ERS Monograph) [Internet]. Sheffield: European Respiratory Society; 2020 [cited 2020 May 6]. p. 276–94. http://public.eblib.com/choice/PublicFullRecord.aspx?p=6181621.
Nayak R, Brogly SB, Lajkosz K, Lougheed MD, Petsikas D. Outcomes of operative and nonoperative treatment of thoracic empyema: a population-based study. Ann Thorac Surg. 2019;108(5):1456–63.
Farjah F, Symons RG, Krishnadasan B, Wood DE, Flum DR. Management of pleural space infections: a population-based analysis. J Thorac Cardiovasc Surg. 2007;133(2):346–51.
Wozniak CJ, Paull DE, Moezzi JE, Scott RP, Anstadt MP, York VV, et al. Choice of first intervention is related to outcomes in the management of empyema. Ann Thorac Surg. 2009;87(5):1525–31.
Redden MD, Chin TY, van Driel ML. Surgical versus non-surgical management for pleural empyema. Cochrane Acute Respiratory Infections Group, editor. Cochrane Database Syst Rev [Internet]. 2017 Mar 17 [cited 2020 Jul 2]. https://doi.org/10.1002/14651858.CD010651.pub2.
Rahman NM, Kahan BC, Miller RF, Gleeson FV, Nunn AJ, Maskell NA. A Clinical Score (RAPID) to identify those at risk for poor outcome at presentation in patients with pleural infection. Chest. 2014;145(4):848–55.
Corcoran JP, Psallidas I, Gerry S, Piccolo F, Koegelenberg CF, Saba T, et al. Prospective validation of the RAPID clinical risk prediction score in adult patients with pleural infection: the PILOT study. Eur Respir J. 2020;16:2000130.
Molnar TF. Current surgical treatment of thoracic empyema in adults. Eur J Cardiothorac Surg. 2007;32(3):422–30.
Chambers A, Routledge T, Dunning J, Scarci M. Is video-assisted thoracoscopic surgical decortication superior to open surgery in the management of adults with primary empyema? Interact Cardiovasc Thorac Surg. 2010;11(2):171–7.
Terra R, Waisberg D, Almeida J, Devido M, Pego-Fernandes P, Jatene F. Does videothoracoscopy improve clinical outcomes when implemented as part of a pleural empyema treatment algorithm? Clinics. 2012;67(6):557–63.
Subotic D, Lardinois D, Hojski A. Minimally invasive thoracic surgery for empyema. Breathe. 2018;14(4):302–10.
Lardinois D, Gock M, Pezzetta E, Buchli C, Rousson V, Furrer M, et al. Delayed referral and Gram-Negative organisms increase the conversion thoracotomy rate in patients undergoing video-assisted thoracoscopic surgery for empyema. Ann Thorac Surg. 2005;79(6):1851–6.
Waller DA, Rengarajan A. Thoracoscopic decortication: a role for video-assisted surgery in chronic postpneumonic pleural empyema. Ann Thorac Surg. 2001;71(6):1813–6.
Cassina PC, Hauser M, Hillejan L, Greschuchna D, Stamatis G. Video-assisted thoracoscopy in the treatment of pleural empyema: stage-based management and outcome. J Thorac Cardiovasc Surg. 1999;117(2):234–8.
Roberts JR. Minimally invasive surgery in the treatment of empyema: intraoperative decision making. Ann Thorac Surg. 2003;76(1):225–30.
Stefani A, Aramini B, della Casa G, Ligabue G, Kaleci S, Casali C, et al. Preoperative predictors of successful surgical treatment in the management of parapneumonic empyema. Ann Thorac Surg. 2013;96(5):1812–9.
Jagelavicius Z, Jovaisas V, Mataciunas M, Samalavicius NE, Janilionis R. Preoperative predictors of conversion in thoracoscopic surgery for pleural empyema. Eur J Cardiothorac Surg. 2017;52(1):70–5.
Chung JH, Lee SH, Kim KT, Jung JS, Son HS, Sun K. Optimal timing of thoracoscopic drainage and decortication for empyema. Ann Thorac Surg. 2014;97(1):224–9.
Bedawi EO, Hassan M, Rahman NM. Recent developments in the management of pleural infection: a comprehensive review. Clin Respir J. 2018;12(8):2309–20.
Bedawi EO. A randomised controlled trial of the feasibility of early administration of clot-busting medication through a chest tube versus early surgery in pleural infection [Internet]. ISRCTN registry; 2019 Jul [cited 2020 Jul 3]. Report No.: ISRCTN18192121. http://www.isrctn.com/ISRCTN18192121.
Rahman NM, Ali N, Brown G, Chapman S, Davies RJO, Gleeson FV, et al. Local anaesthetic thoracoscopy: British Thoracic Society pleural disease guideline 2010. In: BTS Pleural Disease Guideline 2010. II. Thorax; 2010. p. 254–60.
Bhatnagar R. A trial to investigate whether pleuroscopy can be used to treat pleural infection [Internet]. ISRCTN registry; 2017 Jun. Report No.: ISRCTN98460319. https://www.isrctn.com/ISRCTN98460319?q=&filters=conditionCategory:Respiratory&sort=&offset=3&totalResults=708&page=1&pageSize=10&searchType=basic-search.
Davies HE, Rahman NM, Parker RJ, Davies RJO. Use of indwelling pleural catheters for chronic pleural infection. Chest. 2008;133(2):546–9.
Chao YK, Lee C-H, Liu K-S, Wang Y-C, Wang C-W, Liu S-J. Sustained release of bactericidal concentrations of penicillin in the pleural space via an antibiotic-eluting pigtail catheter coated with electrospun nanofibers: results from in vivo and in vitro studies. Int J Nanomedicine. 2015;10:3329–3326.
Meijvis SC, Hardeman H, Remmelts HH, Heijligenberg R, Rijkers GT, van Velzen-Blad H, et al. Dexamethasone and length of hospital stay in patients with community-acquired pneumonia: a randomised, double-blind, placebo-controlled trial. Lancet. 2011;377(9782):2023–30.
Blum CA, Nigro N, Briel M, Schuetz P, Ullmer E, Suter-Widmer I, et al. Adjunct prednisone therapy for patients with community-acquired pneumonia: a multicentre, double-blind, randomised, placebo-controlled trial. Lancet. 2015;385(9977):1511–8.
Fitzgerald DB, Waterer GW, Read CA, Fysh ET, Shrestha R, Stanley C, et al. Steroid therapy and outcome of parapneumonic pleural effusions (STOPPE): study protocol for a multicenter, double-blinded, placebo-controlled randomized clinical trial. Medicine (Baltimore). 2019;98(43):e17397.
Acknowledgements
Funding
No funding or sponsorship was received for this study or publication of this article.
Authorship
All named authors meet the International Committee of Medical Journal Editors (ICMJE) criteria for authorship for this article, take responsibility for the integrity of the work as a whole, and have given their approval for this version to be published.
Disclosures
Anand Sundaralingam, Radhika Banka and Najib M. Rahman have nothing to disclose.
Compliance with Ethics Guidelines
This article is based on previously conducted studies and does not contain any new studies with human participants or animals performed by any of the authors.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-Non-Commercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Sundaralingam, A., Banka, R. & Rahman, N.M. Management of Pleural Infection. Pulm Ther 7, 59–74 (2021). https://doi.org/10.1007/s41030-020-00140-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s41030-020-00140-7