Abstract
Background
People with major neurocognitive disorder might be susceptible to drug-induced QT interval prolongation due to the presence of a number of concomitant risk factors.
Objective
The aim of this study was to investigate the prevalence of QT-prolonging drugs and QT-prolonging drug–drug interactions and associated factors among older people with major neurocognitive disorder.
Methods
In this register-based study, we obtained information regarding QT-prolonging drug use in a large population of older people with major neurocognitive disorder, through record linkage between the Swedish registry for cognitive/dementia disorders, and the Swedish Prescribed Drug Register. QT-prolonging drugs were identified according to the CredibleMeds online database and interactions using the Janusmed interaction database. Drug use was defined as one or more filled prescriptions during a 6-month timeframe, July 01 to December 31, 2017. Associations between people with a QT-prolonging drug and the factors of age and gender were analysed through multiple logistic regression.
Results
Of 35,212 people included in the study, 41.6% had one or more QT-prolonging drug prescribed. The most commonly prescribed drug was donepezil, with a prevalence of 25.0%, followed by citalopram and escitalopram, representing 14.5% and 3.9% of prescriptions in the study population, respectively. Significant associations were found between QT-prolonging drug use and the factors of younger age and female gender. The most prevalent interaction was between citalopram and donepezil (2.7%), followed by the combination of escitalopram and donepezil (0.7%).
Conclusions
In this population of older people with major neurocognitive disorder, QT-prolonging drugs and interactions that increase the risk of torsade de pointes were prevalent. Due to the presence of many risk factors in this population, it is important to continuously evaluate current QT-prolonging drugs and concomitant drug treatment in each individual.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
QT-prolonging drugs were common among older people with major neurocognitive disorder. |
Due to the presence of potential risk factors among this population of older individuals with major neurocognitive disorder, the prevalence of QT-prolonging drugs and relevant interactions warrants concern. |
1 Introduction
Long QT syndrome (LQTS) refers to a condition in which there is a prolongation of the corrected QT (QTc) interval on the electrocardiogram. Many commonly used drugs exhibit QT-prolonging effects, which increase the risk of ventricular tachycardia of the type torsade de pointes (TdP). These QT-prolonging drugs include, for example, antiarrhythmic drugs, certain antidepressant and antipsychotic drugs, and drugs within the groups antibiotics, antihistamines and antimalarial drugs [1]. In addition to use of QT-prolonging drugs, people with drug-induced TdP most often have other concomitant risk factors present, for example older age, female gender, heart disease, renal or hepatic dysfunction, and electrolyte disorders [2, 3]. Further, concomitant prescription of more than one TdP-classified agent has been associated with an increased risk of QTc prolongation, and also interactions between drugs that increase the concentration of the QT-prolonging drug [2].
The prevalence of QT-prolonging drugs among older people seems common. In a large geriatric German population, more than half of the population (58.7%) were prescribed at least one QT-prolonging drug and 22.1% were prescribed at least two of these drugs [4]. Another study among older people admitted to hospital found that 89.7% were prescribed at least one QT-prolonging drug, and more than 30% were prescribed drugs with a known risk of TdP [5].
People with major neurocognitive disorder (NCD) might be susceptible to drug-induced QT interval prolongation due to the presence of a number of concomitant risk factors such as comorbidities, old age (≥65 years), and use of multiple medications. In addition, another risk factor for drug-induced QT interval prolongation is bradycardia, a side effect associated with acetylcholinesterase inhibitors (AChEIs) [2, 6]. Furthermore, other drugs with QT-prolonging effect such as antidepressants are often prescribed to people with major NCD [7]. Despite the potentially high risk of drug-induced QT prolongation among people with major NCD, there are few scientific studies published on this topic. One smaller study from 2019 included 432 patients with major NCD, suspected of syncope or unexplained fall during the previous 3 months. A high prevalence of prolonged QTc that was associated with diuretics but not with psychoactive medications was found among these patients [8]. One recent study using drug data from the Norwegian Prescription Database (NorPD) found that among people using AChEIs, 44% were prescribed drugs that might cause bradycardia and prolonged QT interval. In this study, no diagnoses were available, including the diagnosis of major NCD. Also, the NorPD only includes drug data from people living at home, not those living in nursing homes [9]. Considering that major NCD is a common condition, with multiple risk factors for drug-induced QT interval prolongation as described above, the aim of this study was therefore to describe the use of QT-prolonging drugs in a large population of people diagnosed with major NCD. More specifically, the aim was to investigate the prevalence of QT-prolonging drugs, and QT prolonging drug–drug interactions and associated factors, among older people with major NCD. Through record-linkage between the Swedish registry for cognitive/dementia disorders (SveDem) and the Swedish Prescribed Drug Register (SPDR), we obtained information regarding QT-prolonging drug use in a large population of people with major NCD.
2 Methods
In this cross-sectional study, SveDem [10], SPDR [11] and the Swedish Cause of Death Register [12] were linked through personal identity numbers to obtain information regarding pharmacy refill data among older people with major NCD, and in order to select people who were alive during the chosen time period. Data from a previous study investigating psychotropic drugs in the same population during the same time period as the present study are referred to in the discussion. Results from that study were published previously [7].
2.1 The Swedish Registry for Cognitive/Dementia Disorders
SveDem is a national quality registry for patients with major neurocognitive disorders. The register was started in 2007 and the number of registrations is growing continuously; in April 2022, 107,099 patients were registered. Patients are registered by the date when major NCD diagnosis is established by the physician, in primary care or at a specialised care unit. The patients are followed-up yearly in specialised care units, primary care centres or in nursing homes. Information about age, gender, demographic data, and type of major NCD diagnosis (ICD-10) are some examples of data that are registered [10].
2.2 The Swedish Prescribed Drug Register
SPDR provides data on all prescribed drugs that are dispensed at all Swedish pharmacies. The register was started in 2005 and is complete for all residents in Sweden and contains data with unique patient identifiers for all dispensed prescriptions. The information is restricted to prescribed drugs, over-the counter drugs are not included. Also, drugs dispensed within other parts of health care (e.g. at hospitals) are not included. The register contains data such as age, gender and the dates of medications prescribed and dispensed. Information about how many days of prescribed medications were supplied is not available. All drugs are classified according to the Anatomical Therapeutic Chemical (ATC) classification system [11].
2.3 CredibleMeds
CredibleMeds is an online resource that maintains lists of drugs that have risk of QT prolongation and cardiac arrhythmias. To evaluate and update evaluations, information from published studies, labels, reports and adverse effects are used. The QT-prolonging drugs are then placed into one of four categories: ‘known risk of TdP’, ‘possible risk of TdP’, ‘conditional risk of TdP’, and ‘drugs to avoid in congenital LQTS’. The category ‘known risk of TdP’ includes drugs that prolong the QT interval and are clearly associated with a known risk of TdP, even when taken as recommended. The category ‘possible risk of TdP’ includes drugs that can cause QT prolongation but currently lack evidence for a risk of TdP when taken as recommended, while the category ‘conditional risk of TdP’ includes drugs that are associated with an increased risk of TdP, but only in special circumstances, for example, in the event of overdose or in interaction with other drugs [1].
2.4 Janusmed Interaction Database
In Janusmed interaction database, information about interactions based on pairwise combinations of drug substances are provided. Drug interactions are classified into four different categories (A–D) depending on clinical relevance, and the level of documentation is recorded as 0–4. Type C and D interactions are considered to be clinically relevant; type C refers to interactions that may require dose adjustments, and type D refers to interactions that should be avoided [13].
2.5 Study Population
This study includes people aged ≥65 years and registered in SveDem, with diagnosis date (i.e. the date when the major NCD diagnosis was established according to SveDem) no later than 30 June 2017, and who were alive on December 31, 2017 (n = 35,212). The Swedish Cause of Death Register that includes dates of deaths was used to select people who were alive during the time period. Data regarding filled prescriptions for QT-prolonging drugs was collected for the period July 01 to December 31, 2017.
2.6 Definitions
One or more filled prescriptions during a 6-month timeframe (July 01–December 31, 2017) defined drug use during the period, and dispensing date was used to identify drug use. QT-prolonging drugs classified as ‘known risk of TdP’ (referred to as ‘known risk’ in this study) according to the CredibleMeds online database (with date of 5 December 2021) were included. The drugs were classified pursuant to the ATC classification system. Of the substances in the known-risk category, 34 substances were authorised for the Swedish market at study start (see Appendix in the electronic supplementary material [ESM]). Excluded from these 34 substances in this specific study were antifungal and antibiotic drugs, as well as antiparasitic products, insecticides and repellents, as these drugs often are prescribed as shorter courses of treatment. Furthermore, anesthetic drugs and antineoplastic agents were excluded, leaving 17 substances to be analysed.
Interactions were identified using the Janusmed interaction database. All 17 substances included in this study were investigated pairwise and potentially clinically relevant interactions type C and type D according to Janusmed interaction database were identified.
2.7 Data Analysis
Descriptive statistics were used to summarise the data. Frequencies were calculated for dichotomous variables, and continuous variables were presented as mean values with standard deviation (SD). People who did and did not have a QT-prolonging drug were compared using the Pearson chi-square test and t-test for dichotomous and continuous variables, respectively. Simple and multiple logistic regression analyses were conducted to investigate the association between people with a QT-prolonging drug and the factors of age and gender. The factors age and gender were included in both the simple and the multiple regression models.
IBM SPSS Statistics version 26, and SAS Enterprise Guide 7.1 were used for all processing, calculations and analyses of data. We considered p values <0.05 significant for all statistical tests, and odds ratios (ORs) were calculated with 95% confidence intervals (CIs).
3 Results
Among the study population, 61.8% were women, and 38.2% were men (Table 1). Mean age was 82.7 years. Furthermore, 12,252 (34.8%) people had Alzheimer’s disease (early and late onset), and 6325 (18.0%) had vascular dementia. Of the 35,212 people included in the study, 14,664 (41.6%) had one or more QT-prolonging drug prescribed. There were significant differences between people with and without a QT-prolonging drug regarding gender, age and type of major NCD.
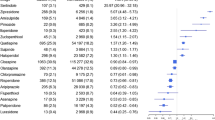
Of the 14,664 persons with one or more QT-prolonging drug prescribed, 13,275 (37.7%) had one, 1365 (3.9%) had two, and 24 (0.1%) had three of these drugs on concomitant prescription during the selected period. The proportion of individuals who filled at least one prescription for QT-prolonging drugs are presented in Table 2. The most commonly prescribed drug was donepezil, with a prevalence of 25.0%. The selective serotonin reuptake inhibitors (SSRIs), citalopram and escitalopram, were prescribed among 14.5% and 3.9%, respectively, of the study population, and 533 people (1.5%) were prescribed haloperidol.
The regression model revealed a significant association between QT-prolonging drug use and female gender (adjusted OR [aOR] 1.22; 95% CI 1.16–1.27) (Table 3). An association was also found between QT-prolonging drug use and younger age; the age categories 85–94 years and 95–104 years had a lower OR in the multiple regression model compared with the age category 65–74 years (aOR 0.90; 95% CI 0.84–0.96 and aOR 0.57; 95% CI 0.49–0.66, respectively). There was no significant association between the age category 75–84 years and the age category 65–74 years (aOR 1.01; 95% CI 0.95–1.08).
When investigating combinations of the 17 substances in the category ‘known risk’, 1352 of the included 35,212 persons (3.8%) had at least one potentially clinically relevant interaction. Table 4 presents the distribution of interactions found between the substances included in this category. The most prevalent interaction was between citalopram and donepezil (2.7%), followed by the combination of escitalopram and donepezil (0.7%). All interactions found were pharmacodynamic, with an additive prolongation effect on QT interval.
4 Discussion
In this study, we found that the prevalence of QT-prolonging drugs among people with major NCD was 42%, and 3.8% of the study population had at least one potentially clinically relevant interaction. The most commonly prescribed drug was donepezil, followed by citalopram, escitalopram and haloperidol. The most prevalent interaction was between citalopram and donepezil followed by the combination of escitalopram and donepezil.
The prevalence of QT-prolonging drugs is obviously dependent on the study population investigated, as well as the definitions used. In Sweden in 2015, 17% of all people aged 65 years or older were prescribed a QT-prolonging drug from the known risk and possible risk categories [3]. As previously mentioned, in a study among older hospitalised people, with a mean age of 79.7 years, 89.7% were prescribed at least one QT-prolonging drug and more than 30% were prescribed drugs with a known risk of TdP [5]. Multi-morbidity among older people is common, which increases the risk of being exposed to polypharmacy, and polypharmacy is one contributing factor to prolonged QT interval [14, 15]. People with major NCD have more comorbidities and a higher drug burden than people without this disorder [16, 17]. In addition, people with major NCD commonly use QT-prolonging drugs such as AChEIs and antidepressants in the treatment of major NCD and behavioural and psychological symptoms of dementia (BPSD), which partly explains the high prevalence seen in this study. Indeed, in our study investigating only drugs in the known risk category, the most commonly prescribed QT-prolonging drug was donepezil—one of three AChEIs used in the treatment of AD and related major NCDs. In this specific study population, donepezil was the most commonly prescribed AChEI, 3–4 times more used than rivastigmine and galantamine [7]. Donepezil was added to the known risk category in 2015, while galantamine is on the conditional risk list, and rivastigmine is not listed in any of the categories [1, 18]. No specific AChEI is recommended in guidelines [19].
Citalopram was the second most commonly used QT-prolonging drug in this study, followed by escitalopram. Guidelines from the Swedish Medical Products Agency and the National Board of Health and Welfare recommend SSRIs as the first pharmacological alternative for depression amongst the elderly, and also as a treatment option with regard to BPSD such as irritability, agitation and aggressive behaviour in people with major NCD [20, 21]. Citalopram was the most commonly used SSRI in this study population, as described in a previous study [7]. However, in some recommendations regarding BPSD, sertraline is recommended ahead of citalopram/escitalopram [19]. Reasons for this could be the potential drug–drug interactions associated with citalopram, for example, citalopram in combination with omeprazole, and the interaction between citalopram and donepezil, both highly relevant examples of combinations that increase the risk of TdP [13]. Also, sertraline, unlike citalopram, is not listed in the known risk category by CredibleMeds. This drug is instead categorised as a conditional risk drug. In a register-based study including all individuals aged 18 years or older in Sweden, citalopram was associated with a higher incidence of TdP compared with mirtazapine and sertraline [22]. Of note, in 2011 there was a recommendation regarding restriction to a maximal dose of 20 mg citalopram among the elderly due to the risk of QT prolongation [23]. Considering the relatively weak evidence regarding the effects of antidepressants amongst the elderly, and amongst the elderly with major NCD, it is important to carefully follow-up the individual response to treatment, and regularly reconsider the indication. Nevertheless, it is important to emphasise that many older people also benefit from the treatment [24,25,26,27].
Haloperidol was prescribed to 1.5% of the study population, a relatively low prevalence. The negative effects with using antipsychotics among people with major NCD are well known, with risk of extrapyramidal symptoms, stroke and increased mortality even with short-term use [28,29,30,31,32]. Antipsychotic drugs should therefore be used with caution, and the effect and possible side effects should be evaluated shortly after prescribing. Today, risperidone is the antipsychotic drug recommended in the treatment of BPSD [20]. Risperidone was also found in the majority of people prescribed antipsychotics in the investigated population [7]. Risperidone is categorised as conditional risk for TdP while haloperidol is listed on the known risk list [1].
There were 1365 people using more than one drug from the known risk list. As previously stated, the use of more than one QT-prolonging drug increases the risk of TdP [2]. The most prevalent interaction found in this study—citalopram in combination with donepezil—is an example of a pharmacodynamic interaction with this additive effect. This also applies to the interaction between citalopram/escitalopram and haloperidol. However, also of importance are pharmacokinetic interactions with drugs, which do not in themselves increase the risk of QT prolongation, but that increase the concentration of the QT-prolonging drug. These interactions were not found in this study, but a relevant example is the interaction mentioned above between omeprazole and citalopram, which increases plasma levels of citalopram and thereby increases the risk for QT prolongation. This interaction was among the most common interactions found in a previous study conducted amongst people with major NCD [33].
In the adjusted regression analysis, filled prescriptions for QT-prolonging drugs were significantly more common among women, and for those who were 65–74 years compared with the two oldest age groups. However, the difference in age between those with and without a QT-prolonging drug was only 0.5 year, and all included participants were older than 65 years. As previously described, female gender and advanced age are risk factors for TdP with the use of QT-prolonging drugs, and major NCD is more prevalent in individuals with older age and female gender [34]. This also indicates that individuals with major NCD are particularly vulnerable to the effects and side effects of drugs. However, the regression analysis in this study only covers age and gender, and cannot give a full picture of potentially associated factors. In addition, some previously mentioned risk factors can change over time, and thereby increase the risk of TdP, for example, electrolyte disturbances due to treatment with diuretics. In an observational study amongst people with major NCD, and with at least one episode of suspected syncope or unexplained fall, prolonged corrected QT was found in 25% of individuals [8].
The main limitation of this study is that we had no clinical data information, such as concomitant comorbidities or characteristics that might increase the risk for QTc prolongation. Consequently, we had no information about prolonged QT time or arrhythmias among the participants. We also did not include different types of major NCD in the regression model because of uncertainties regarding the large proportion of diagnoses such as unspecified dementia. Altogether, this means that the regression analyses performed do not give a full picture of associated factors. Further, we did not perform any sub-analyses regarding, for example, concomitant prescription of QT-prolonging drugs or regarding specific drugs. This should also be considered when interpreting the results. There was also a lack of information regarding doses or indications for prescription. Nor is it known how the individuals used their medications, whether on a daily basis or as part of shorter courses of treatment. Furthermore, there was a lack of information regarding the total number of drugs among the participants, which would have been interesting. The strength of this study is that it was possible to investigate and describe QT-prolonging drug use amongst a large group of people with major NCD, through the use of registries. The use of SveDem registry ensures that all included individuals have a diagnosis of major NCD. However, some types of major NCD diagnosis are changed after registration, although less than 5% of all registrations during 2007–2020 had been changed during follow-up [35]. Still, since the regression analysis in the present study does not include different types of major NCD, we believe that this does not have any impact of the main results.
In summary, even if this study has limitations, it is important to pay attention to the use of QT-prolonging drugs in this population, considering the increased risk with older age and general use of multiple medications. An evaluation of current QT-prolonging drugs, the individual risk factors, and other concomitant drug treatment should be regularly assessed for each individual.
5 Conclusions
In this population of older people with major neurocognitive disorder, QT-prolonging drugs and interactions that increase the risk of torsade de pointes were prevalent. With regard to the presence of many risk factors in this population, it is important to continuously evaluate current QT-prolonging drugs and concomitant drug treatment in each individual.
References
Woosley RL, Heise CW , Gallo T, Tate J, Woosley D and Romero KA, www.CredibleMeds.org, QTdrugs List, AZCERT, Inc. 1457 E. Desert Garden Dr., Tucson, AZ 85718. Accessed 16 Dec 2021.
Drew BJ, Ackerman MJ, Funk M, Gibler WB, Kligfield P, Menon V, et al. Prevention of torsade de pointes in hospital settings: a scientific statement from the American Heart Association and the American College of Cardiology Foundation. Circulation (New York, NY). 2010;121:1047–60.
The National Board of Health and Welfare. Läkemedel som kan orsaka allvarliga rubbningar i hjärtats rytm. 2019 [Eng. Drugs that can cause severe disorders of the heart rhythm]. https://www.socialstyrelsen.se/globalassets/sharepoint-dokument/artikelkatalog/ovrigt/2019-4-2.pdf.
Schächtele S, Tümena T, Gaßmann K-G, Fromm MF, Maas R. Co-prescription of QT-interval prolonging drugs: an analysis in a large cohort of geriatric patients. PLoS ONE. 2016;11(5): e0155649.
Rossi M, Marzi F, Natale M, Porceddu A, Tuccori M, Lazzerini PE, et al. Drug-Associated QTc Prolongation in Geriatric Hospitalized Patients: a Cross-Sectional Study in Internal Medicine. Drugs Real World Outcomes. 2021;8(3):325–35.
Park-Wyllie LY, Mamdani MM, Li P, Gill SS, Laupacis A, Juurlink DN. Cholinesterase inhibitors and hospitalization for bradycardia: a population-based study. PLoS Med. 2009;6(9): e1000157.
Kindstedt J, Sjölander M, Lövheim H, Gustafsson M. Psychotropic drug use among older people with major neurocognitive disorder: a cross-sectional study based on Swedish national registries. Eur J Clin Pharmacol. 2022;78:477–87. https://doi.org/10.1007/s00228-021-03241-7.
Bo M, Ceccofiglio A, Mussi C, Bellelli G, Nicosia F, Riccio D, et al. Prevalence, predictors and clinical implications of prolonged corrected QT in elderly patients with dementia and suspected syncope. Eur J Intern Med. 2019;61:34–9.
Efjestad AS, Ihle-Hansen H, Hjellvik V, Engedal K, Blix HS. Use of drugs with risk of heart rate-related problems is common in Norwegian dementia patients treated with acetylcholinesterase inhibitors: a prevalence study based on the Norwegian prescription database. Front Pharmacol. 2022;12:791578–791578.
Swedish registry for cognitive/dementia disorders (SveDem). https://www.ucr.uu.se/svedem/
Wettermark B, Hammar N, Michaelfored C, Leimanis A, Otterblad Olausson P, Bergman U, et al. The new Swedish Prescribed Drug Register—opportunities for pharmacoepidemiological research and experience from the first six months. Pharmacoepidemiol Drug Saf. 2007;16(7):726–35.
The Swedish Board of Health and Welfare; The Cause of Death Register. Available from: https://www.socialstyrelsen.se/statistik-och-data/register/alla-register/dodsorsaksregistret/
Stockholm County Council, the Health and Medical Care Administration; Janusmed interactions. https://janusmed.sll.se/interaktioner. Accessed 16 Dec 2021.
Aubert CE, Streit S, Da Costa BR, Collet TH, Cornuz J, Gaspoz JM, et al. Polypharmacy and specific comorbidities in university primary care settings. Eur J Intern Med. 2016;35:35–42.
Swenson RS, Murphy-Ende K. Prolonged QT interval in patients receiving psychotropic medications. J Am Psychiatr Nurses Assoc. 2020;26(4):344–53.
Lai SW, Lin CH, Liao KF, Su LT, Sung FC, Lin CC. Association between polypharmacy and dementia in older people: a population-based case-control study in Taiwan. Geriatr Gerontol Int. 2012;12(3):491–8.
Park HY, Park JW, Song HJ, Sohn HS, Kwon JW. The association between polypharmacy and dementia: a nested case-control study based on a 12-year longitudinal cohort database in South Korea. PLoS ONE. 2017;12(1):e0169463–e0169463.
Woosley R, Heise C, Romero K. Changes Made to CredibleMeds® Lists. https://crediblemeds.org/blog/changes-made-crediblemedsr-lists
Västerbotten County Council. Terapirekommendationer 2021 [Eng. Therapy recommendations]. https://regionvasterbotten.se/for-vardgivare/behandlingsstod-och-vardriktlinjer/lakemedel/behandlingsrekommendationer/terapirekommendationer.
Swedish Medical Products Agency. Läkemedelsbehandling och bemötande vid Beteendemässiga och Psykiska Symptom vid Demenssjukdom—BPSD. 2008 [Eng. Pharmacological treatment and management of behavioural and psychological symptoms of dementia—BPSD]. https://www.lakemedelsverket.se/490322/globalassets/dokument/behandling-och-forskrivning/behandlingsrekommendationer/bakgrundsdokument/bakgrundsdokumentation-bpsd.pdf
The National Board of Health and Welfare. Indikatorer för god läkemedelsterapi hos äldre. 2017 [Eng. Indicators for evaluating the quality of older people’s drug therapy]. https://www.socialstyrelsen.se/globalassets/sharepoint-dokument/artikelkatalog/ovrigt/2017-6-7.pdf
Danielsson B, Collin J, Nyman A, Bergendal A, Borg N, State M, et al. (Drug use and torsades de pointes cardiac arrhythmias in Sweden: a nationwide register-based cohort study. BMJ Open. 2020;10(3):e034560-e.
Swedish medical products agency. 2011. https://www.mynewsdesk.com/se/lakemedelsverket/pressreleases/citalopram-saenkt-maxdos-rekommenderas-698966
Swedish agency for health technology assessment and assessment of social services. 2015 Behandling av depression hos äldre [Eng. Treatment of depression in the elderly]. https://www.sbu.se/sv/publikationer/SBU-utvarderar/behandling-av-depression-hos-aldre-/
Seitz DP, Adunuri N, Gill SS, Gruneir A, Herrmann N, Rochon P. Antidepressants for agitation and psychosis in dementia. Cochrane Database Syst Rev. 2011. https://doi.org/10.1002/14651858.CD008191.pub2.
Masopust J, Protopopová D, Vališ M, Pavelek Z, Klímová B. Treatment of behavioral and psychological symptoms of dementias with psychopharmaceuticals: a review. Neuropsychiatr Dis Treat. 2018;14:1211–20.
Bains J, Birks J, Dening T. Antidepressants for treating depression in dementia. Cochrane Database Syst Rev. 2002. https://doi.org/10.1002/14651858.CD003944.
Gill SS, Bronskill SE, Normand SL, Anderson GM, Sykora K, Lam K, et al. Antipsychotic drug use and mortality in older adults with dementia. Ann Intern Med. 2007;146(11):775–86.
Rochon PA, Normand SL, Gomes T, Gill SS, Anderson GM, Melo M, et al. Antipsychotic therapy and short-term serious events in older adults with dementia. Arch Intern Med Res. 2008;168(10):1090–6.
Langballe EM, Engdahl B, Nordeng H, Ballard C, Aarsland D, Selbaek G. Short- and long-term mortality risk associated with the use of antipsychotics among 26,940 dementia outpatients: a population-based study. Am J Geriatr Psychiatry. 2014;22(4):321–31.
Schwertner E, Secnik J, Garcia-Ptacek S, Johansson B, Nagga K, Eriksdotter M, et al. Antipsychotic treatment associated with increased mortality risk in patients with dementia. A registry-based observational cohort study. J Am Med Dir Assoc. 2019;20(3):323-9.e2.
Gill SS, Rochon PA, Herrmann N, Lee PE, Sykora K, Gunraj N, et al. Atypical antipsychotic drugs and risk of ischaemic stroke: population based retrospective cohort study. BMJ. 2005;330(7489):445–8.
Sönnerstam E, Sjölander M, Lövheim H, Gustafsson M. Clinically relevant drug–drug interactions among elderly people with dementia. Eur J Clin Pharmacol. 2018;74(10):1351–60.
Swedish agency for health technology assessment and assessment of social services. Dementia—Etiology and Epidemiology. 2008. https://www.sbu.se/contentassets/2c12ea9230ef419a84a0078c5fa48ae7/dementia_vol12.pdf
Swedish registry for cognitive/dementia disorders (SveDem). Annual report 2020. https://www.ucr.uu.se/svedem/om-svedem/arsrapporter. Accessed 30 Jul 2021
Acknowledgements
The Swedish registry for cognitive/dementia disorders, SveDem, www.ucr.uu.se/svedem, provided data on people with major neurocognitive disorders.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
This study received financial support from the Swedish Dementia Association. The funders had no role in the study design, data collection and analysis, decision to publish or preparation of the manuscript.
Conflicts of interest
M.G, M.A and M.S declare that they have no potential conflicts of interest that might be relevant to the contents of this manuscript.
Availability of data and materials
The datasets generated during and/or analysed in the present study are available from the corresponding author on reasonable request.
Author contributions
MG and MS contributed to the study conception, design and subject acquisition. Material preparation, data collection and analysis were performed by MG, MA and MS. The first draft of the manuscript was written by MA and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Competing interests
The authors declare no competing interests.
Ethics approval
The study was approved by the Regional Ethical Review Board in Umeå, Sweden (registration number 2017-256-31M).
Consent to participate
Not applicable.
Consent for publication
Not applicable.
Code availability (software application or custom code)
Not applicable.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Gustafsson, M., Altufaili, M. & Sjölander, M. Prevalence of Drugs and Drug Combinations that Increase Risk of Prolonged QT Time Among People with Major Neurocognitive Disorder Living in Sweden: A Cross-Sectional Registry Study. Drugs - Real World Outcomes 10, 61–68 (2023). https://doi.org/10.1007/s40801-022-00341-3
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40801-022-00341-3