Opinion statement
The past 30 years have seen broad changes in the diagnosis and management of vesicoureteral reflux (VUR). Recently, a clinical debate has generated an open discussion in academic circles. New evidence has shifted treatment patterns away from widespread surgical management and recently brought into question some pharmacologic treatments. VUR is usually not hazardous by itself but is a significant risk factor for urinary tract infection (UTI) and less commonly, renal scarring and insufficiency. Given the costs and morbidity of UTI as well as the potential for significant renal injury, our approach remains conservative. Careful follow-up, parental education about pathophysiology and management of VUR and UTI, and management of bowel and bladder dysfunction (BBD), when present, are the foundations of treatment. Additionally, though we recognize the limitation of continuous antibiotic prophylaxis (CAP), we believe that the benefits outweigh the risks and costs for many patients. Careful observation can be considered in patients with a single medical home, parental understanding of what UTI signs and symptoms are, low grade VUR, no history of complicated UTIs, and close follow-up. Surgical management remains a relevant option for select patients who fail conservative measures with breakthrough UTIs or failure to resolve. Minimally invasive surgical options are available with acceptable outcomes though open ureteroneocystostomy still carries the highest success rate.
Similar content being viewed by others
Introduction
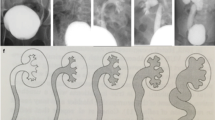
Vesicoureteral reflux (VUR) is the retrograde flow of urine from urinary bladder to upper urinary tract. VUR is graded I–V depending on the degree of dilatation and renal collecting system morphology [1]. VUR is the most common congenital urological abnormality of urinary tract occurring in 1 % of newborns [2]. For children with antenatal hydronephrosis on prenatal ultrasound, up to 20 % may be diagnosed with VUR [3, 4]. Like other congenital anomalies of the kidney and urinary tract, VUR has a strong genetic component. VUR occurs in 27.4 % of siblings of affected children and in 35.7 % of the children of affected parents [5]. Thirty to forty percent of children investigated for UTI have VUR [6]. With recurrent UTI, children with VUR are at risk for renal scarring that ultimately can result in chronic or end-stage renal disease. In 2006, in the USA alone, costs exceeded $100 million for hospitalizations related to VUR [7].
VUR came into focus after the advent of voiding cystourethrography (VCUG) in 1950. Hodson and Edward showed the relationship of VUR with chronic pyelonephritis [8]. Historically, VUR was treated almost exclusively by open surgical reimplantation of the ureter also known as ureteroneocystostomy (UNC). With the recognition that VUR often resolves spontaneously with time, the concept of continuous antibiotic prophylaxis (CAP) was introduced to prevent UTI while waiting for VUR resolution. The identification of bowel and bladder dysfunction (BBD) as a related risk factor for UTI and VUR outcomes has prompted a greater focus on co-managing these functional disorders. Additionally, advances in technology have improved minimally invasive surgical approaches for treating VUR.
Currently, a large academic discussion has focused on the utility of antibiotic prophylaxis in children with VUR. The 2011 AAP technical report reviewed eight clinical trials in a meta-analysis and questioned the utility of CAP. This report found no difference in placebo group and antibiotic prophylaxis group in the rate of recurrent pyelonephritis, regardless of reflux grade and age [9]. However, a significant difference in the rate of UTI in prophylactic group was noted when all forms of UTI were included.
Recently, two large randomized studies were published that demonstrated the benefit of CAP in preventing UTIs in children with VUR. The Randomized Intervention for Children with Vesicoureteral Reflux (RIVUR) study, a large multicenter, randomized placebo-controlled trial, involving 607 children between the ages of 2 to 71 months with grade I to grade IV reflux, showed that prophylaxis reduced the risk of recurrence of UTI by almost 50 % (95 % CI, 0.34 to 0.74) [10••]. Another large, multicenter clinical trial in Sweden that involved 203 children aged 1 to younger than 2 years with grade III to IV reflux also showed a reduction in recurrent UTIs in girls on CAP [11••]. Both studies indicate a role for CAP, especially in young girls, in preventing UTI occurrence.
Another global academic debate has focused on when to screen for VUR. Depending on the context and availability of imaging modalities, a clear, evidenced-based consensus cannot be reached on when to screen children for VUR. Furthermore, similar ambiguity exists with when to screen children of parents with VUR and siblings of children with VUR [5]. The discussion of the approach to the patient with possible VUR is outside the scope of this review.
Education
Parents of children with VUR often have misconceptions about the nature of VUR and UTIs [12]. Parents should be educated about the pathophysiology of VUR, signs and symptoms of UTI, and the indications and methods for collecting urine for culture. This time spent educating families may aid appropriate detection and treatment of UTIs and decrease chronic untreated UTIs and false diagnoses. Many symptoms may be falsely attributed to VUR or UTI and consequently may lead to detection bias. For example, bacteriuria is often noted in inappropriately collected urine samples (such as bagged urine) and labeled by parents and practitioners as a “UTI.” Confirming the diagnosis of a UTI requires both symptoms and a positive urine culture. Typical symptoms of UTI include dysuria, urinary frequency, urgency, or hematuria. Atypical symptoms may include fever, malaise, abdominal or flank pain, diarrhea, vomiting, and weight loss. Malodorous urine is often cited by parents as a symptom of UTI when in fact the association is weak [13]. Unexplained fever in the child with VUR should prompt a workup for a urinary source if no other cause is readily apparent. Proper urine collection for culture often requires catheterization in young children who are unable to cooperate adequately for clean catch collection. Screening via urinalysis of bagged urine sample may be appropriate only when followed by confirmatory catheterized sample collection and culture.
Pharmacologic treatment
Pharmacological treatment of VUR aims at prevention of recurrent UTI. Current evidence suggests that CAP reduces the rate of recurrent UTI until the reflux resolves. The majority of lower grade VUR spontaneously resolves as the child grows [14]. CAP consists of prescribing daily antibiotics at one quarter to one half the normal therapeutic dose. Trimethoprim-sulfamethoxazole (TMP-SMX), amoxicillin, and nitrofurantoin are the most commonly used CAP agents. The significant drawback to CAP is antibiotic resistance. The RIVUR trial demonstrated a significant amount of resistance to TMP-SMX in patients on prophylaxis with breakthrough UTI compared to patients on placebo [10••].
Trimethoprim-sulfamethoxazole
Mechanism of action: TMP-SMX combination acts to inhibit the formation of bacterial tetrahydrofolate which is required for protein synthesis. Sulfonamides are structurally similar to para-aminobenzoic acid (PABA) used by bacteria for synthesis of folic acid [15]. Sulfamethoxazole (sulfonamide) inhibits the enzyme dihydropteroate synthetase and the formation of dihydropteroic acid, which converts to dihydrofolic acid. Trimethoprim inhibits the enzyme dihydrofolate reductase which is required for conversion of dihydrofolate to tetrahydrofolic acid [16].
Standard dosage: Standard prophylactic dose of TMP-SMX is based on TMP dose of 2 mg/kg/day in children ≥2 months. The maximum single dose was 160 mg TMP/dose. Dose adjustment is required for patients with chronic kidney disease.
Contraindications: TMP-SMX is contraindicated in neonates/infants younger than 2 months and patients with a history of hypersensitivity to any component of TMP-SMX, Steven-Johnson syndrome, G6PD and pyruvate kinase deficiencies, liver disease, pregnancy, prolonged QT interval, and porphyria [17].
Main drug interactions: Warfarin, cyclosporine, phenytoin sodium, cyclosporine, angiotensin-converting enzyme inhibitors and receptor blockers, and hypoglycemic urticarial agents.
Main side effects: Nausea, vomiting, loss of appetite, rash, pruritus, and urticaria. Skin-related side effects are more common with TMP-SMX combination compared to sulfonamides alone (5.9 vs. 1.7). Serious, but rare, side effects include Steven-Johnson syndrome, toxic epidermal necrolysis, and agranulocytosis ∼0.1 % for sulfonamides) [16].
Special points: Patients with G6PD deficiency may develop hemolysis.
Cost/cost effectiveness: TMP-SMX is an inexpensive medicine.
Amoxicillin
Mechanism of action: Amoxicillin is a broad-spectrum, second-generation, beta-lactam penicillin. Like other penicillins, amoxicillin inhibits the enzymes involved in bacterial cell wall synthesis, inhibiting the formation of peptidoglycan linkages, with activity against Gram-negative organisms [18]. Enzymes involved in bacterial cell wall synthesis are detected by radioactively labeled penicillins and are called penicillin-binding proteins. Amoxicillin penetrates the porin channels of Gram-negative bacteria but is still susceptible to beta-lactamase enzyme. Recently, the role of murein hydrolase enzyme activity is also shown to play the role in mechanism of action of penicillins [19].
Standard dosage: Amoxicillin is given orally at 10–15 mg/kg/dose (preferably in the evening) for prophylaxis of VUR in infants ≤2 months. Maximum single dose, 500 mg.
Contraindications: Hypersensitivity to amoxicillin, penicillins or other beta-lactams.
Main drug interactions: Penicillins increase the anticoagulant effect of vitamin K antagonist, increase the serum levels of methotrexate, and interfere with typhoid vaccine.
Main side effects: Rash (>1 %) and diarrhea (>1 %) are the most common side effects. Rarely, dental discoloration and candidiasis can occur. Serious side effects such as anaphylactoid reactions are rare (0.004–0.04 %) [20].
Special points: Patients with infectious mononucleosis can develop rash while taking amoxicillin.
Cost/cost-effectiveness: Amoxicillin is an inexpensive medicine.
Nitrofurantoin
Mechanism of action: Nitrofurantoin is converted by bacterial nitroreductase (flavoproteins) into active intermediates that inactivate bacterial ribosomal proteins and halt protein synthesis in bacteria including DNA and RNA [21]. Nitrofurantoin is bactericidal at therapeutic doses.
Standard dosage for UTI prophylaxis: 1–2 mg/kg as a single daily dose; maximum dose, 100 mg/day.
Contraindications: Nitrofurantoin is contraindicated in patients with GFR less than 60 ml/h, anuria, oliguria, history of cholestatic jaundice, hypersensitivity to drug and its components, and children less than 1 month of age.
Main drug interactions: Nitrofurantoin interacts with norfloxacin, nitric oxide, spironolactone, and magnesium trisilicate.
Main side effects: Gastrointestinal side effects (4.4 %) such as abdominal discomfort, nausea, and vomiting are most common. Skin rashes and urticaria are also common (3.2 %). Pulmonary complications (0.7 %) such as chest pain or interstitial pneumonitis may also rarely occur. Serious side effects like hepatotoxicity, neurotoxicity, and hematological reactions are extremely rare [22].
Special points: Nitrofurantoin is not indicated for the treatment of pyelonephritis. Drug absorption is better if taken with meal and can cause brown discoloration of urine.
Cost/cost effectiveness: Nitrofurantoin is an inexpensive medicine.
Surgery
The aim of surgical management is to prevent VUR by elongating the intramural tunnel of the ureter or altering the shape or angle of the ureteral orifice to allow coaptation during bladder filling. Open surgical ureteroneocystostomy (UNC) continues to be the gold standard for correction of VUR. Hutch was the first to report surgical correction in seven out of nine paraplegic patients with VUR in 1952 [23]. Over the past 60 years, multiple surgical techniques, including endoscopic and laparoscopic techniques, have been described.
Open ureteroneocystostomy
Open ureteroneocystostomy (UNC) is considered the gold standard in treatment due to its high surgical success rate and low complication rate. Long-term success of open UNC to correct VUR is 98 % [24•]. The surgery is classified by its approach to the ureter as intravesical, extravesical, or combined. Well-established surgical principles to ensure a good clinical outcome include the following: recognition, treatment and resolution of secondary causes of VUR, adequate mobilization of the ureter without tension or damage to its blood supply, creation of a submucosal tunnel that has at least a 5:1 ratio of length to ureteral lumen, and good detrusor muscle backing within the tunnel to create an antireflux mechanism via compression of the ureter during bladder filling and emptying. Recent studies have concentrated on reducing morbidity by improving preoperative and postoperative care, refinement of postoperative analgesia, reducing the size of the incision, and minimizing catheter usage [25]. Complication rates for UNC remain low, and the most commonly reported complications include urinary tract infection, persistent VUR, contralateral de novo VUR, and obstruction. Contralateral VUR after unilateral UNC is reported to be 5.6–18 % with a trend towards development of contralateral VUR in patients with high-grade (grade 4–5) ipsilateral VUR [26, 27]. Prophylactic bilateral UNC for unilateral VUR is not universally recommended due to high spontaneous resolution rates of the de novo contralateral VUR [28].
Minimally invasive ureteroneocystostomy
Recently, both laparoscopic and robotic assisted laparoscopic ureteroneocystostomy (LUNC/RALUNC) have been introduced as viable surgical treatment options for VUR. Both intravesical and extravesical techniques have been described which follow the same surgical principles of open surgery. Reported success and complication rates are similar to that of open UNC, 89–97.6 % [29, 30]. In a recent retrospective study comparing open UNC (39 patients) and RALUNC (39 patients), no significant difference was found in pain but significantly longer operative times for both intravesical and extravesical RALUNC. The study also noted shorter hospital course and transurethral catheter duration associated with intravesical RALUNC compared to open UNC. Both clinical and radiologic success rates were found to be similar [31].
Endoscopic injection
Matouschek described the first endoscopic injection (EI) for treatment of VUR in 1981, using polytetrafluoroethylene (PTFE) paste injected into the subepithelium at the ureteral orifice. Since then, O’Donnell and Puri (1986) popularized the technique and their initial results had a reported success rate of 75 % after one subureteric injection of Teflon. This procedure became popular in many countries but never achieved widespread use in the USA. The US Food and Drug Administration (FDA) did not approve Teflon for this indication over concerns regarding the potential migration of Teflon particles. Polydimethylsiloxane, cattle collagen, calcium hydroxylapatite, polyacrylate-polyalcohol copolymer, and dextranomer/hyaluronic acid have also been used for EI. In 2001, the FDA approved the use of dextranomer/hyaluronic acid (Dx/HA) (Deflux, Oceana Therapeutics, Inc., Edison, NJ) as the first FDA-approved subepithelial injectable treatment for VUR in the USA. EI is a less invasive procedure with minimal morbidity that can be performed as an outpatient procedure. Two key challenges with endoscopic treatment of reflux are reproducibility and durability of the results. A recent meta-analysis of subureteric injection for VUR in 8101 renal units in a total of 5527 patients showed a primary success rate of 78.5 % in grade I and II VUR, 72 % for grade III, 63 % for grade IV, and 51 % for grade V VUR. The subsequent success rate of second and third injections was 68 and 34 %, respectively [24•]. The success rate was also found to be lower in duplicated systems compared to single systems (50 vs. 73 %) and neuropathic bladder patients compared to patients with a normal bladder (62 vs. 74 %). The Swedish reflux trial also calls into question the long-term efficacy of EI in high grade VUR (grades III–V). The authors found a 20 % recurrence rate of VUR after EI in children who had previously been treated with a high success rate (86 %). The same study also noted that UTI rates were similar in patients who received EI or prophylactic antibiotics (23 vs. 19 %). The rates of infection and renal scaring were also similar in patients who received Dx/HA vs. patients who had not received any treatment [32•].
Another key challenge with EI treatment is reproducibility of the results. Several techniques have been described to help improve surgical outcomes. In the original subureteric Teflon injection method (STING), the injection needle is inserted 2–3 mm distal to the ureteral orifice and advanced 4–5 mm submucosally prior to injection. The goal is to form a crest in the distal submucosal tunnel leading to coaptation of the ureter. Within the last decade, recent EI modifications have improved clinical outcomes. The hydrodistention-implantation technique (HIT) and double HIT methods have demonstrated a significant improvement in resolution rate after 1 year of follow-up [33, 34]. Multiple retrospective review articles have noted that despite the introduction of endoscopic Dx/HA injection for VUR, the rate of UNC has remained stable. Since 2002, the average number of EI antireflux surgeries performed per institution has decreased likely secondary to concerns over the long-term efficacy and cost-effectiveness of EI as a viable treatment option [35, 36].
Bowel and bladder dysfunction
Bowel and bladder dysfunction (BBD) is a relatively new term which replaces the previously used dysfunction elimination syndrome (DES) [37]. BBD is an umbrella term which encompasses functional disorders of bowel and lower urinary tract (LUT), the full taxonomy of which are out of the scope of this article. Briefly, BBD is divided into bowel dysfunction (e.g., constipation, encopresis, etc.) and LUT dysfunction (e.g., urgency, frequency, enuresis, etc.).
Association between vesicoureteral reflux and BBD
Bowel and bladder dysfunction is clearly associated with VUR, UTIs, and the outcomes of treatment for VUR. The largest analysis of VUR and BBD was performed by the American Urological Association (AUA) guideline committee and was published in 2010 [38••]. Pooled meta-analysis of 16 study arms of 2039 children with VUR showed that 32 % had concurrent BBD. In the meta-analysis of patients on CAP, including patients with high and low grade reflux, BBD was associated with 31 % rate of spontaneous VUR resolution. In comparison, 61 % of patients without BBD had resolution of reflux. Additionally, breakthrough UTIs in children on CAP occurred in 44 % of children with BBD as compared to only 13 % of patients without BBD.
Febrile or symptomatic UTI can occur even after surgical treatment of VUR and is increased in patients with BBD. In the AUA meta-analysis, 22.6 % of children who had surgery for VUR had a subsequent UTI if they had BBD [38••]. UTI incidence was only 4.8 % after successful surgery in children without BBD. Failure of EI for VUR has been classically associated with BBD; however, recent reports have shown that patients with active BBD who are undergoing active treatment (urotherapy) can have satisfactory outcomes equivalent to those without BBD [39, 40]. Persistence of VUR after UNC is rare. In a retrospective review of 400 patients who underwent UNC at our institution, all 11 children with persistent VUR after surgery had significant BBD [41].
Evaluation of BBD
Evaluation of children with VUR and suspected BBD should start with a careful and detailed history to document symptoms including incontinence (frequency, timing, and volume), voiding frequency, voiding urgency, voided volumes, fluid intake, and frequency and quality of bowel movements. Details about maladaptive behaviors and signs should also be collected, such as voiding postponement, posture during voiding, wiping patterns for female patients, post-void dribbling, straining with defecation, etc. History of specific behaviors should be elicited such as the “potty dance” or “Vincent curtsy” wherein a female child will squat and press the heel of the foot against the perineum. This sign is classically associated with BBD, specifically voiding postponement and overactive bladder. The use of bowel/bladder diaries and validated questionnaires such as the dysfunctional voiding symptom score (DVSS) have been shown to increase specificity in diagnosing BBD and can be used to document improvement after intervention [42]. The Bristol stool chart is another simple metric which can improve accuracy of parent reported stool quality. Noninvasive uroflowmetry, post-void residual (PVR) measurement, and pelvic floor electromyography (EMG) are useful adjuncts typically performed in the urologist’s office and can help distinguish between the various subcategories of LUT dysfunction. Invasive testing such as urodynamics is rarely indicated in the workup of BBD in neurologically intact children.
Urotherapy
Behavioral modification is the frontline treatment for BBD and is often termed “urotherapy.” This consists of five domains including the following:
-
Education of parents and children about normal and abnormal LUT function
-
Individualized instruction regarding timed voiding, proper posture and pelvic floor relaxation with voiding, proper wiping technique for females, avoidance of holding maneuvers, etc.
-
Lifestyle advice regarding fluid intake, avoidance of bladder irritants, fiber intake, etc.
-
Registration of symptoms using bladder diaries and/or frequency/volume charts
-
Support and encouragement via regular follow-up and reinforcement
Recent studies have shown the effectiveness of adjunct strategies to improve compliance and outcomes with urotherapy. Use of a programmable watch which gives an audible or vibrating reminder to facilitate timed voiding has been shown to increase compliance with urotherapy as well as decrease incontinence episodes though it was only studied on children older than 5 years of age [43]. A recent pilot study was also published about the efficacy of group visits for urotherapy which have been proposed to improve compliance and decrease the costs of care. The study was focused on older children (>5 years of age) with BBD and showed significant improvement in LUT symptoms in children receiving either individual or group therapy sessions [44].
Pelvic floor biofeedback
In addition to standard urotherapy, many practitioners have reported success from an additional regimen of pelvic floor muscle (PFM) physical therapy using biofeedback. Protocols vary but typically consist of a series of visits in which the child is instructed on PFM contraction and relaxation. This is often facilitated by a visual/animated computer program that gives feedback using EMG signals from leads placed on the perineum. Some studies have documented benefits from biofeedback in uroflowmetry patterns, post-void residuals, and in rates of UTI [45, 46]. However, the largest meta-analysis of biofeedback for LUT dysfunction was published recently and found no significant difference in rates of UTI, resolution of incontinence, or maximum urinary flow rate as compared to standard urotherapy [47].
Bowel management
Bowel dysfunction and bladder dysfunction are clearly linked with multiple proposed mechanisms explaining the relationship [48•]. Parents often focus on urinary symptoms and may not notice or report bowel symptoms without prompting. The first step in treatment is to educate parents and children about proper bowel habits and function. Constipation is very common and may require disimpaction followed by prevention through dietary modification and/or daily osmotic stool softeners such as polyethylene glycol [48•]. Some have advocated treating all children with LUT dysfunction for constipation based on the very high rate of coincident constipation among these patients, the unreliability of parent reporting of bowel symptoms, and the low cost and risk associated with this treatment [49]. However, a recent randomized trial comparing polyethylene glycol versus placebo for patients with isolated bladder urgency symptoms found no difference in resolution of bladder symptoms between the two groups [50]. Bowel dysfunction should be identified, quantified using objective metrics, and treated appropriately. However, all patients with VUR and LUT dysfunction may not benefit from blanket treatment.
Emerging therapies
With rising concerns of antimicrobial resistance and almost zero new antibiotics in the development pipeline, new therapies and approaches to patients with VUR are desperately needed. No longer can we take a “one size fits all” approach to children with VUR. Studies to elucidate the genetic and host factors that lead to recurrent UTI and renal scarring risks are desperately needed. In the modern day world of precision medicine, each patient will need a UTI recurrence/scarring risk score to establish what therapy (CAP, UNC, observation, EI, etc.) conveys the most benefit with the least amount of risk.
Conclusion
Vesicoureteral reflux continues to be a significant source of pediatric morbidity. Though not all patients with VUR will develop UTIs and most will not suffer renal injury, it is difficult to predict outcomes in advance for each patient. BBD is clearly associated with outcomes of VUR and should be managed appropriately. Surgical and pharmacologic management remain important approaches to reduce the morbidity and expense of UTIs as well as potentially decrease risk of renal injury and insufficiency. Future research may allow individual risk stratification and allow targeted intervention for patients at the highest risk.
References and Recommended Reading
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Lebowitz RL, Olbing H, Parkkulainen KV, Smellie JM, Tamminen-Mobius TE. International system of radiographic grading of vesicoureteric reflux. International Reflux Study in Children. Pediatr Radiol. 1985;15(2):105–9.
Hiraoka M, Hori C, Tsukahara H, Kasuga K, Ishihara Y, Kotsuji F, et al. Vesicoureteral reflux in male and female neonates as detected by voiding ultrasonography. Kidney Int. 1999;55(4):1486–90.
Farhat W, McLorie G, Geary D, Capolicchio G, Bagli D, Merguerian P, et al. The natural history of neonatal vesicoureteral reflux associated with antenatal hydronephrosis. J Urol. 2000;164(3 Pt 2):1057–60.
Jaswon MS, Dibble L, Puri S, Davis J, Young J, Dave R, et al. Prospective study of outcome in antenatally diagnosed renal pelvis dilatation. Arch Dis Child Fetal Neonatal Ed. 1999;80(2):F135–138.
Skoog SJ, Peters CA, Arant BS, Copp HL, Elder JS, Hudson RG, et al. Pediatric Vesicoureteral Reflux Guidelines Panel Summary Report: Clinical Practice Guidelines for Screening Siblings of Children With Vesicoureteral Reflux and Neonates/Infants With Prenatal Hydronephrosis. J Urol. 2010;184(3):1145–51.
Hoberman A, Charron M, Hickey RW, Baskin M, Kearney DH, Wald ER. Imaging studies after a first febrile urinary tract infection in young children. N Engl J Med. 2003;348(3):195–202.
Spencer JD, Schwaderer A, McHugh K, Vanderbrink B, Becknell B, Hains DS. The demographics and costs of inpatient vesicoureteral reflux management in the USA. Pediatr Nephrol. 2011;26(11):1995–2001.
Hodson CJ, Edwards D. Chronic pyelonephritis and vesico-ureteric reflex. Clin Radiol. 1960;11:219–31.
Finnell SM, Carroll AE, Downs SM. Subcommittee on Urinary Tract I: Technical report-Diagnosis and management of an initial UTI in febrile infants and young children. Pediatrics. 2011;128(3):e749–770.
Hoberman A, Greenfield SP, Mattoo TK, Keren R, Mathews R, Pohl HG, et al. Antimicrobial prophylaxis for children with vesicoureteral reflux. N Engl J Med. 2014;370(25):2367–76. This multicenter prospective randomized clinical trial enrolled 607 children and showed clearly the advantage of continuous antibiotic prophylaxis on rate of recurrence of UTI on children aged 2–71 with grade I –IV VUR; however it did not show difference in degree of scarring in subjects on prophylaxis.
Brandström P, Esbjörner E, Herthelius M, Swerkersson S, Jodal U, Hansson S. The Swedish reflux trial in children: III. Urinary tract infection pattern. J Urol. 2010;184(1):286–91. This multicenter clinical trial enrolled 203 children (128 girls and 75 boys), 1 to less than 2 years of age, with grade III and IV vesicoureteral reflux. The study showed the benefit of prophylactic therapy in girls with VUR on febrile UTI recurrence. However this trial did not include children younger than 1 year and those with low grade VUR.
Harmsen M, Wensing M, van der Wouden JC, Grol RP. Parents' awareness of and knowledge about young children's urinary tract infections. Patient Educ Couns. 2007;66(2):250–5.
Gauthier M, Gouin S, Phan V, Gravel J. Association of malodorous urine with urinary tract infection in children aged 1 to 36 months. Pediatrics. 2012;129(5):885–90.
Estrada Jr CR, Passerotti CC, Graham DA, Peters CA, Bauer SB, Diamond DA, et al. Nomograms for predicting annual resolution rate of primary vesicoureteral reflux: results from 2,462 children. J Urol. 2009;182(4):1535–41.
Gleckman R, Blagg N, Joubert DW. Trimethoprim: mechanisms of action, antimicrobial activity, bacterial resistance, pharmacokinetics, adverse reactions, and therapeutic indications. Pharmacotherapy. 1981;1(1):14–20.
Petri WJ, Knollmann BC. Sulfonamides, Trimethoprim-Sulfamethoxazole, Quinolones, and Agents for Urinary Tract Infections. In: Brunton LLCB, editor. Goodman and Gillman’s the pharmacological basis of therapeutics. New York: NY: McGraw-Hill; 2011.
Product Information: BACTRIMTM oral tablets oral double strength tablets, sulfamethoxazole trimethoprim oral tablets and oral double strenth tablets. In. Philadelphia, PA: AR Scitntific, Inc. (Per FDA); 2013.
Petri WJ. Penicillins, cephalosporins, and other beta-lactam antibiotics. In: Brunton LLCB, Knollmann BC, editors. Goodman and Gillman’s the pharmacological basis of therapeutics. New York: NY: McGraw-Hill; 2011.
Bayles KW. The bactericidal action of penicillin: new clues to an unsolved mystery. Trends Microbiol. 2000;8(6):274–8.
Product Information: amoxicillin oral capsules, oral tablets, oral powder for suspension, amoxicillin oral capsules, oral tablets, oral powder for suspension. Sandoz Inc, (per DailyMed), Princeton, NC. In.; 2013.
Tu Y, McCalla DR. Effect of activated nitrofurans on DNA. Biochim Biophys Acta. 1975;402(2):142–9.
Karpman E, Kurzrock EA. Adverse reactions of nitrofurantoin, trimethoprim and sulfamethoxazole in children. J Urol. 2004;172(2):448–53.
Hutch JA. Vesico-ureteral reflux in the paraplegic: cause and correction. J Urol 2002. 1952;167(3):1410–4. discussion 1422.
Elder JS, Diaz M, Caldamone AA, Cendron M, Greenfield S, Hurwitz R, et al. Endoscopic therapy for vesicoureteral reflux: a meta-analysis. I. Reflux resolution and urinary tract infection. J Urol. 2006;175(2):716–22. This meta-analysis evaluated the success of endoscopic treatment of vesicoureteral reflux pooled from multiple studies and included subgroup analysis. Endoscopic treatment outcomes were shown to be favorable though not as good as open surgical treatment.
Celik O, Ipekci T, Aydogdu O, Yucel S. Current medical diagnosis and management of vesicoureteral reflux in children. Nephrourol Mon. 2014;6(1), e13534.
Diamond DA, Rabinowitz R, Hoenig D, Caldamone AA. The mechanism of new onset contralateral reflux following unilateral ureteroneocystostomy. J Urol. 1996;156(2 Pt 2):665–7.
Minevich E, Wacksman J, Lewis AG, Sheldon CA. Incidence of contralateral vesicoureteral reflux following unilateral extravesical detrusorrhaphy (ureteroneocystostomy). J Urol. 1998;159(6):2126–8.
Burno DK, Glazier DB, Zaontz MR. Lessons learned about contralateral reflux after unilateral extravesical ureteral advancement in children. J Urol. 1998;160(3 Pt 2):995–7. discussion 1038.
Peters CA. Robotically assisted surgery in pediatric urology. Urol Clin N Am. 2004;31(4):743–52.
Casale P, Patel RP, Kolon TF. Nerve sparing robotic extravesical ureteral reimplantation. J Urol. 2008;179(5):1987–9. discussion 1990.
Marchini GS, Hong YK, Minnillo BJ, Diamond DA, Houck CS, Meier PM, et al. Robotic assisted laparoscopic ureteral reimplantation in children: case matched comparative study with open surgical approach. J Urol. 2011;185(5):1870–5.
Brandström P, Nevéus T, Sixt R, Stokland E, Jodal U, Hansson S. The Swedish reflux trial in children: IV. Renal damage. J Urol. 2010;184(1):292–7. The renal scarring outcomes from the Swedish reflux trial (reference 11 above) were reviewed in this paper. New renal scars were highly associated with febrile UTIs in female children. The highest rate of new scarring was observed in girls in the surveillance arm (not on antibiotic prophylaxis).
Kirsch AJ, Perez-Brayfield M, Smith EA, Scherz HC. The modified sting procedure to correct vesicoureteral reflux: improved results with submucosal implantation within the intramural ureter. J Urol. 2004;171(6 Pt 1):2413–6.
Yucel S, Gupta A, Snodgrass W. Multivariate analysis of factors predicting success with dextranomer/hyaluronic acid injection for vesicoureteral reflux. J Urol. 2007;177(4):1505–9.
Herbst KW, Corbett ST, Lendvay TS, Caldamone AA. Recent trends in the surgical management of primary vesicoureteral reflux in the era of dextranomer/hyaluronic acid. J Urol. 2014;191(5 Suppl):1628–33.
Lendvay TS, Sorensen M, Cowan CA, Joyner BD, Mitchell MM, Grady RW. The evolution of vesicoureteral reflux management in the era of dextranomer/hyaluronic acid copolymer: a pediatric health information system database study. J Urol. 2006;176(4 Pt 2):1864–7.
Austin PF, Bauer SB, Bower W, Chase J, Franco I, Hoebeke P, Rittig S, Walle JV, von Gontard A, Wright A, et al. The standardization of terminology of lower urinary tract function in children and adolescents: Update report from the standardization committee of the International Children's Continence Society. Neurourol Urodyn 2015.
Peters CA, Skoog SJ, Arant BS, Copp HL, Elder JS, Hudson RG, et al. Summary of the AUA guideline on management of primary vesicoureteral reflux in children. J Urol. 2010;184(3):1134–44. This is the latest AUA guideline on VUR management. The article includes the results from a large meta-analysis of VUR with respect to multiple variables and clinical outcomes including the association between BBD and VUR resolution.
Van Batavia JP, Nees SN, Fast AM, Combs AJ, Glassberg KI. Outcomes of vesicoureteral reflux in children with non-neurogenic lower urinary tract dysfunction treated with dextranomer/hyaluronic acid copolymer (Deflux). J Pediatr Urol. 2014;10(3):482–7.
Arlen AM, Scherz HC, Filimon E, Leong T, Kirsch AJ. Is routine voiding cystourethrogram necessary following double hit for primary vesicoureteral reflux? J Pediatr Urol. 2015;11(1):40.e41-45.
Noe HN. The role of dysfunctional voiding in failure or complication of ureteral reimplantation for primary reflux. J Urol. 1985;134(6):1172–5.
Farhat W, Bägli DJ, Capolicchio G, O'Reilly S, Merguerian PA, Khoury A, et al. The dysfunctional voiding scoring system: quantitative standardization of dysfunctional voiding symptoms in children. J Urol. 2000;164(3 Pt 2):1011–5.
Hagstroem S, Rittig S, Kamperis K, Djurhuus JC. Timer watch assisted urotherapy in children: a randomized controlled trial. J Urol. 2010;184(4):1482–8.
Brownrigg N, Pemberton J, Jegatheeswaran K, DeMaria J, Braga LH. A pilot randomized controlled trial evaluating the effectiveness of group vs individual urotherapy in decreasing symptoms associated with bladder-bowel dysfunction. J Urol. 2015;193(4):1347–52.
Ladi-Seyedian S, Kajbafzadeh AM, Sharifi-Rad L, Shadgan B, Fan E. Management of non-neuropathic underactive bladder in children with voiding dysfunction by animated biofeedback: a randomized clinical trial. Urology. 2015;85(1):205–10.
Tugtepe H, Thomas DT, Ergun R, Abdullayev T, Kastarli C, Kaynak A, et al. Comparison of biofeedback therapy in children with treatment-refractory dysfunctional voiding and overactive bladder. Urology. 2015;85(4):900–4.
Fazeli MS, Lin Y, Nikoo N, Jaggumantri S, Collet JP, Afshar K. Biofeedback for nonneuropathic daytime voiding disorders in children: a systematic review and meta-analysis of randomized controlled trials. J Urol. 2015;193(1):274–9.
Burgers RE, Mugie SM, Chase J, Cooper CS, von Gontard A, Rittig CS, et al. Management of functional constipation in children with lower urinary tract symptoms: report from the Standardization Committee of the International Children’s Continence Society. J Urol. 2013;190(1):29–36. This paper reports a consensus view on the clinical implications and management of bowel dysfunction co-incident to lower urinary tract symptoms. Though not a systematic review, it is evidence-based and includes several useful clinical tools and treatments for pediatric constipation.
Champeau A, Baskin L. Editorial comment. J Urol. 2013;190(1):36.
Bush NC, Shah A, Barber T, Yang M, Bernstein I, Snodgrass W. Randomized, double-blind, placebo-controlled trial of polyethylene glycol (MiraLAX®) for urinary urge symptoms. J Pediatr Urol. 2013;9(5):597–604.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Derrick L. Johnston, Aslam H. Qureshi, Rhys W. Irvine, Dana W. Giel, and David S. Hains declare that they have no conflict of interest
Human and animal rights and informed consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
This article is part of the Topical Collection on Pediatric Nephrology
Derrick L. Johnston, Aslam H. Qureshi and Rhys W. Irvine contributed equally to this work.
Rights and permissions
About this article
Cite this article
Johnston, D.L., Qureshi, A.H., Irvine, R.W. et al. Contemporary Management of Vesicoureteral Reflux. Curr Treat Options Peds 2, 82–93 (2016). https://doi.org/10.1007/s40746-016-0045-9
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40746-016-0045-9