Abstract
Introduction
Kidney failure negatively affects opportunities for work participation. Little is known about work functioning of employed CKD patients. This study investigates work-related outcomes, and examines associations between patient characteristics and employment status.
Methods
We performed a cross-sectional survey study in nine nephrology outpatient clinics in the Netherlands among working age (18–67 years) CKD Stage G3b-G5, dialysis and transplant patients (n = 634; mean age 53.4 years (SD 10); 53% male; 47% Stage G3b-G5, 9% dialysis, 44% transplantation). We assessed employment status, work disability, work-related characteristics (i.e., work situation, working hours, job demands), work functioning (i.e., perceived ability to work, productivity loss, limitations in work), work environment (i.e., work accommodations, psychosocial work environment), as well as health status and fatigue.
Results
Sixty-five percent were employed reporting moderate work ability. Of those, 21% received supplementary work disability benefits, 37% were severely fatigued, 7% expected to drop out of the workforce, and 49% experienced CKD-related work limitations. Work accommodations included reduced working hours, working at a slower pace, adjustment of work tasks or work schedule, and working from home. Multivariable analysis of sustained employment showed associations with younger age, male gender, higher level of education, better general and physical health and pre-emptive transplantation. Transplant patients had the highest work ability and highest expectation to maintain work. Dialysis patients had the highest productivity loss and perceived the most limitations regarding functioning in work. Stage G3b-G5 patients reported the lowest social support from colleagues and highest conflict in work and private life.
Conclusions
Employed CKD patients experience difficulties regarding functioning in work requiring adjustment of work or partial work disability. In addition to dialysis patients, stage G3b-G5 patients are vulnerable concerning sustained employment and work functioning.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Loss of kidney function negatively affects opportunities for work participation. Kidney replacement therapy, such as dialysis, is often associated with loss of work [1, 2]. Transplantation offers recipients the potential to return to a productive working life, but a substantial proportion of patients remain unemployed [3]. Besides medical treatment, kidney failure in itself is disabling and causes changes in employment, as even late-stage CKD patients may stop working [4].
Previous studies on work participation in CKD patients focused mainly on employment rates. Little is known about how patients perceive their work functioning, their work ability, work productivity and work relationships [5]. Regarding work limitations, a Dutch survey study [6] showed that 85% of employed CKD patients experienced work limitations, in the literature also known as presenteeism, or attending work while ill [7]. Moreover, 40% needed work accommodations, usually a reduction in working hours [5]. Work accommodations and job control may thus facilitate sustained employment [8].
From the patients’ perspective, participation in paid work is highly valued, as it enhances quality of life, provides a sense of identity, and provides financial security [9]. Participation in work was among the ten highest-ranked outcomes prioritized by CKD patients [10]. Nephrology care may have the potential to help CKD patients remain employed, however, currently, work-related issues may not be adequately addressed in the nephrology care [11]. Greater insight into the working life of CKD patients and potential risk groups may help identify effective interventions, may inform targeting of these interventions and as such may enhance the development of a supportive infrastructure enabling patients to remain employed in order to improve their quality of life [11, 12].
To address this knowledge gap, we designed a study that investigates sustained employment, work disability, work functioning, and work environment in CKD patients. In addition, we assess differences between employed and non-employed patients and examine associated patient characteristics of sustained employment, as well as differences between stage G3b-G5, dialysis, and transplant patients concerning work-related outcomes.
Methods
Study design and population
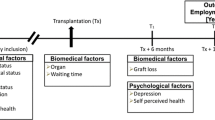
For this cross-sectional survey study (May–September 2019), nine nephrology, dialysis and transplantation departments in the Netherlands invited CKD Stage G3b-G5 patients of working age (18–67 years) to participate. Patients on kidney replacement therapy (dialysis or transplantation) were included if they had started dialysis or received their transplantation 6 months to 5 years prior to the start of the study. Patients were excluded if they were unable to understand Dutch. To increase the homogeneity of the study population, patients with advanced cancer or heart failure were excluded, as were patients with a life expectancy of less than 1 year as determined by the nephrologist or specialized nurse. Eligible patients were invited by a letter from their nephrologist and consented to participate by completing an online, or if they preferred, a paper questionnaire. Non-responders received a reminder within 3 weeks. Figure 1 presents a flow diagram of the inclusion. For every 50 respondents, a gift voucher of 100 euro was raffled among the respondents.
The study adhered to the Declaration of Helsinki and was approved by the Medical Ethics Review Board of the University Medical Center Groningen (M15.169470).
Socio-demographic, clinical and health status characteristics
Socio-demographic characteristics assessed were: age, gender, highest attained level of education, ethnicity and financial situation. Clinical characteristics included primary kidney disease, type of dialysis or transplantation, and retransplantation. Comorbidity was assessed with a list of conditions selected by nephrologists (i.e., heart, cerebrovascular, lung or rheumatic disease, diabetes, amputation, epilepsy, migraine, osteoarthritis, permanent injury impairment, depression, other), and the number was categorized as: no comorbidities, 1, and ≥ 2.
We measured general health (1 item), physical functioning (2 items) and mental functioning (3 items) using subscales from the Kidney Disease Quality of Life-Short Form (KDQoL) [13]. Raw scale scores were transformed (0–100 scale). Higher scores indicate better health, physical and mental functioning.
Fatigue was assessed using the fatigue severity subscale (8 items) of the Checklist Individual Strength (CIS) [14]. Items were scored on a 7-point Likert scale (1–7). Higher scores indicate more severe fatigue; a cutoff score > 35 indicates severe fatigue.
Employment and work disability status, and work-related characteristics
Employment was defined as working for at least one hour per week in a paid position [15]. Full-time students, unpaid caregivers, and those who retired early were considered as non-employed. Work disability was defined as receiving either full or partial work disability benefits administered under Dutch Work Incapacity Acts. After a sickness absence of two years, employees can apply for a disability benefit. Accredited insurance physicians assess the legitimacy of work disability, which can be either full or partial disability, and granted temporarily or permanently [16].
Work-related characteristics included work situation (working according to contract; supplementary work disability benefits; sick leave), and working hours (minor job, < 12 h/week; part-time job, 12–29 h/week; full-time job, ≥ 30 h/week). Job demands were assessed using a self-constructed question (‘What kind of tasks do you perform in your current job?’) with three response options (‘mainly physically demanding tasks’, ‘mainly mentally demanding tasks’, ‘both physically and mentally demanding tasks’).
Work functioning
We assessed different dimensions of work functioning: work ability, productivity loss, limitations in work performance, and expectation to work in the future [17].
The first item of the Work Ability Index (WAI) asks patients to estimate their current work ability compared with their lifetime best (0 = ‘unable to work’ to 10 = ‘lifetime best’) [18]. This score is classified into: ‘poor’ (0–5), ‘moderate’ (6–7), ‘good’ (8–9) and ‘excellent’ (10) [19].
Productivity loss at work was measured using the quantity item of the Quantity and Quality (QQ) questionnaire [20]. Respondents indicated how much work they actually performed during regular hours on their last regular working day, compared to an average working day before they experienced CKD-related limitations. Response options scaled from 1 (‘practically nothing’) to 10 (‘normal quantity’). Productivity loss based on a regular 8-h working day, was calculated by the formula [(10 – quantity score)/10] × 8 h [20].
Limitations in work performance due to CKD were assessed using a self-constructed question (‘Does the CKD restrict you from performing your job?’) with six response options (1 = ‘no limitations’, 6 = ‘not able to work at all’), and by assessing the type of limitation (e.g., working slower or working fewer hours). In addition, we assessed the expectation to work at 6 months (yes/maybe/no).
Work environment
We measured various aspects of the work environment: adjustment of work (yes/no), type of provided work accommodations, interpersonal relations, and reactions to the work situation.
Adjustment of work (yes/no) was assessed with a self-constructed question: ‘Have any adjustments been made to your work on your initiative or your employer’s initiative?’ If ‘yes’, respondents could indicate which type of work accommodations were made.
Interpersonal relations (social support by colleagues and by management; recognition) and reactions to the work situation (meaning at work; overall assessment of the psychosocial work environment; job satisfaction; conflict between work-life and private life) were assessed with subscales of the Danish Psychosocial Work Environment Questionnaire (DPQ) [21]. Most items had a 5-points response option (1 = ‘to a very small extent’, 5 = ‘to a very large extent’), whereas the subscales job satisfaction and psychosocial work environment were scored on a scale from 0 (‘lowest possible level’) to 10 (‘highest possible level’). We calculated subscale scores by averaging the transformed (0–100 scale) item scores. Higher scores indicate higher levels of the measured dimension.
Statistical analysis
Descriptive characteristics were stratified for CKD stage (i.e., Stage G3b-G5, dialysis, transplantation) and for employment status. We performed descriptive analyses, analyzed differences between employed and non-employed patients, and differences in work-related variables between CKD stages, using chi-squared tests and Fisher’s Exact tests (nominal or ordinal variables), and using t-tests, one-way ANOVAs, or nonparametric Kruskall-Wallis tests (continuous variables). Because we performed multiple comparisons, the level of statistical significance was set at P < 0.01.
Associations between socio-demographic, clinical and health characteristics, and the outcome ‘sustained employment’ (employed vs. non-employed), were examined by logistic regression analysis. After examination of the univariable associations, characteristics with an association of P < 0.10 were entered into the multivariable model. Sequentially deleting the characteristic with the weakest association resulted in a final model containing only variables related to the outcome (P < 0.05). Presence of multicollinearity was tested by calculating variance-inflated factors. In case of missing data, we followed the questionnaire instructions to calculate (sub)scale scores [13, 14, 18,19,20,21]. For self-constructed items, missing data were not imputed. We analyzed data using SPSS, version 26 (SPPS, Inc,. Chicago).
Results
Study population
We invited a total of 1907 patients to participate. Questionnaires were completed by 634 patients, consisting of 298 Stage G3b-G5 patients, 56 dialysis patients, and 280 patients with functioning kidney transplants. Of the dialysis patients, 43 (77%) were receiving hemodialysis and 13 (23%) peritoneal dialysis (Table 1). For the majority of transplant patients, it was their primary kidney transplantation (n = 249, 90%). Almost half of the transplant patients had received a pre-emptive transplantation (n = 128; 46%). Twenty-two percent reported polycystic kidney disease as their primary kidney disease and 64% had one or more comorbidities. Participants’ mean age was 53 years (range 19–67); 53% were men, 34% had only primary education.
Employment and work disability status
Sixty-five percent were employed and 35% were work disabled (Table 1). Of the dialysis patients, 52% had a paid job, compared to 68% of the CKD3b-G5 patients and 64% of the transplant patients. Of the non-employed, 61% were work disabled, 13% were looking for a job, 13% had retired early, and 11% never had a job (data not shown).
Differences between employed and non-employed patients
Table 2 reports socio-demographic, clinical, and health status characteristics for employed and non-employed patients. Employed patients were younger, were more often male, more often had a higher educational level, were less often receiving work disability benefits, and less often had a shortage of money. Employed patients also had fewer comorbidities, better health status, and less fatigue (37% vs. 53%).
Regarding kidney replacement therapy, compared to non-employed transplant patients, employed transplant patients more often received a pre-emptive transplantation and less often a deceased transplantation with prior dialysis. Although among employed dialysis patients the rate of peritoneal dialysis was higher, it was not statistically significant.
Associations of sustained employment with socio-demographic, clinical and health characteristics
Univariable regression analysis (Table 3) showed significant associations of sustained employment with age, gender, education, dialysis, deceased donor transplantation, renal vascular disease/diabetes, comorbid conditions, health status and fatigue.
Due to a significant correlation between comorbidity and health status (Spearman’s Rho: − 0.40; p < 0.001), we built two multivariable models: one with health status and one with comorbidity. Both final models showed significant associations with employment status for advanced age (55–64 yr, OR 0.14; 95% confidence interval (CI) 0.30–0.64 and OR 0.12; CI 0.03–0.53), being female (OR 0.51; CI 0.33–0.78 and OR 0.49; CI 0.32–0.75), and higher education (tertiary education, OR 2.62; CI 1.53–4.49 and OR 2.75; CI 1.63–4.62). Compared to stage G3b-G5 patients, transplant patients had lower odds of being employed (OR 0.40; CI 0.25–0.64 and OR 0.48; CI 0.3–0.76). In the model including comorbidity, dialysis patients had lower odds of being employed compared to stage G3b-G5 patients (OR 0.48; CI 0.24–0.97) as well. In the model including health status, better general (OR 1.03; CI 1.02–1.05) and better physical health (OR 1.02; CI 1.01–1.02) indicated higher odds of being employed. Comorbidity was deleted in the last step of this final model because of the weakest and non-significant association (1 comorbid condition OR 0.77; CI 0.43–1.37; 2 comorbid conditions, OR 0.52; CI 0.29–0.94; P 0.08). However, in the model without health status, having two or more comorbid conditions and fatigue indicated lower odds of being employed (OR 0.33; CI 0.19–0.57 and OR 0.96; CI 0.95–0.98, respectively).
Work-related characteristics, work functioning and work environment of employed patients
Table 4 shows that of the employed patients, 71% worked according to contract, whereas 21% received supplementary work disability benefits and 8% were on sick leave. The majority had a full-time job and predominantly mentally demanding tasks.
Regarding work functioning, patients had moderate work ability (mean WAI 7.8) and reported a mean productivity loss of 2.0 h/day. Forty-nine percent experienced CKD-related limitations in their work and 7% expected to drop out of the workforce within the following 6 months.
Twenty-six percent of the patients had made some adjustments in their work. Frequently provided accommodations were: working fewer hours (51%), working at a slower pace (42%), adjustment of work tasks (31%) or work schedule (24%), working from home (19%), and change of position (17%). Patients scored relatively high on meaning at work, psychosocial environment and job satisfaction (mean ranges 79.1–81.4).
Differences between CKD stages in work characteristics, work functioning and work environment
Comparison between employed Stage G3b-G5, dialysis, and transplant patients showed that dialysis patients were more often partially work disabled (55%) and on sick leave (21%), and more often had minor or part-time jobs (Table 4).
Regarding work functioning, transplant patients reported the highest level of work ability (mean 8.2; ‘good’), experienced the least limitations in work performance (41%), and 91% expected to maintain work in 6 months. Dialysis patients had ‘poor’ work ability (mean 5.4), the highest productivity loss and highest proportion of patients (90%) experiencing limitations, as well as the highest proportion that expected to drop out of the workforce (22%).
Results on work environment showed the greater need for work adjustment among dialysis patients (54%). Compared to dialysis and transplant patients, stage G3b-G5 patients reported less social support from colleagues (mean 63.1) and these patients perceived more conflict between work and private life (mean 31.1).
In order to check for potential confounding of age, gender and educational level, we built adjusted models for continuous variables (see Supplementary File), which showed that all statistically significant associations listed in Table 4 remained significant.
Discussion
This study investigated sustained employment in Stage G3b-G5, dialysis, and transplant patients. Two thirds of the study group had a paid job (60% full-time). However, 21% of these working patients received supplementary work disability benefits, and in total, one third of the study group was (partially) work disabled. Employed patients had better health although one third reported severe fatigue. Half of employed patients experienced CKD-related limitations at work and one in four patients needed some work adjustments. Non-employed patients experienced financial hardship, underlining the importance of employment for maintaining an income. Multivariable regression analysis showed associations of younger age, male gender, higher education, better health status, and early/late-stage CKD (CKD G3b-G5) with being employed. Dialysis patients reported the greatest limitations and work adjustments. Stage G3b-G5 patients experienced the lowest level of support from colleagues and felt more conflict in their work- and private life. Regarding transplantation, pre-emptive transplant patients had the highest employment rate.
Compared to the 69% employment rate in the general Dutch population [22], Sage G3b-G5 patients have a similar employment rate (68%), whereas transplantation patients (64%) and dialysis patients (52%) have lower rates. Although comparison is difficult because of variability in measurement of employment and in characteristics of the study participants across studies and countries, available literature shows high variability in employment rates of CKD patients (range 18–82%) [3, 23, 24] as is the case in patients with other chronic conditions (range 14–75%) [6, 25]. Compared to the 6% work disability rate in the general population [25], we found relatively high disability rates among patients (i.e., stage G3b-G5 29%; dialysis 66%; transplantation 36%), which is in line with previous studies [1, 4, 26,27,28].
In addition to employment and work disability status, our study focused on how employed CKD patients function at work. We found slightly lower work ability levels (mean WAI 7.8, SD 4.1) than those reported in previous studies among general working populations (mean 8.2, 95% CI 8.2–8.4 [27]; mean 7.95 ± 1.2 to 8.48 ± 1.4 [28]). However, of the employed patients in our study, half reported limitations at work due to CKD, a lower percentage than in a previous Dutch study among CKD patients (85%)[6].
The present study showed multiple associations between patient characteristics and sustained employment. Concerning transplantation, pre-emptive transplantation is positively associated with employment, potentially explained by avoidance of the harmful effects of dialysis on general health [29], and its subsequent risk of job loss. The multivariable models indicated social and gender inequalities; more poorly educated patients and women were at higher risk of unemployment. Moreover, poor health increased the risk of unemployment. With regard to CKD stage, transplant patients have lower odds of being employed compared to stage G3b-G4 patients. This indicates that concerning work participation, transplant patients are at a disadvantage compared to patients before the start of kidney replacement therapy. We found that 23% of transplant patients still depended on work disability benefits. This indicates decreased work ability and persistent functional limitations in transplant patients, also found in previous studies [4].
A remarkable result was that 50% of the employed Stage G3b-G5 patients experienced work performance limitations and 24% adopted work accommodations such as reducing working hours, working at a slower pace, and adjusting work tasks. Seven percent expected to drop out of the workforce, and another 8% were uncertain about maintaining their work in six months. Moreover, patients experienced the lowest level of support from colleagues. In its early stages, CKD is often an invisible condition that may be poorly understood by others [30]. At the workplace, patients often avoid or postpone disclosure of their CKD out of fear of stigmatization and prejudice, and worries about job loss [31]. Interestingly, stage G3b-G5 patients more often perceived conflict between work- and private life compared to dialysis and transplant patients; their private life suffered under the amount of energy and time they spent at work. Clearly, these patients struggle to find an acceptable work-life balance. Early employment-related counseling may support patients [12, 32].
Dialysis patients appeared particularly vulnerable concerning employment and work functioning [1]. Compared to Stage G3b-G5 and transplant patients they reported low work ability, more sickness absence and supplementary work disability benefits, more productivity loss, as well as greater need for work adjustments. Autonomy and job control (i.e., the possibility to plan and pace work tasks [8]), work accommodations [33], and dialysis scheduling around work [8] can support patients in remaining productive workers.
Our study expands the knowledge on the impact of CKD on the work life of patients, which is an innovative research topic in nephrology. The comprehensive assessment of work functioning informs clinicians on work situations and limitations in work performance. The range of identified work accommodations shows the patients’ opportunities of handling work-related limitations. Another strength of this study is the inclusion of patients in CKD stage G3b-G5, a group often neglected in studies concerning the impact of kidney failure on patients’ lives.
A study limitation is the convenience sampling in nine nephrology, dialysis, and transplantation departments; this did not allow for a central tracking system with an overview of eligible patients and characteristics in all participating centers. Consequently, reasons for non-participation were not registered and may be a source of bias. Moreover, as we lacked information about CKD patients who were not willing to participate we were unable to compare responders with non-responders. As a consequence, it is not possible to conclude that our study sample is representative of all CKD patients and might overestimate the employment rates of the overall CKD patient population. As some previous studies in the Netherlands [1] showed lower employment rates among CKD patients, and others showed similar rates [4, 6], our study may overestimate employment status and underestimate limitations in work functioning and work disability. In addition, our sample tends to be better educated which generally is associated with higher employment rates. Furthermore, the large proportion of pre-emptive and living donor transplant patients, and patients with polycystic kidney disease, as well as the relatively low proportion of diabetes as primary disease that is common for the Netherlands, may limit generalizability of findings to other countries with different patient characteristic distributions. The relatively small sample size of dialysis patients, with a small proportion of peritoneal dialysis, restricted statistical testing of some variables. In addition, we did not collect data on occupational type or occupational position. Possibly, patients from more socially disadvantaged positions may experience greater socioeconomic impact of CKD. Future research must show whether work impact varies across occupational positions.
In conclusion, although work participation is feasible for many CKD patients, they often experience substantial limitations in work functioning that require adjustment of work or partial work disability, combined with a part-time job. Patients with early/late-stage CKD struggle with their work-life balance and support at work, and in transplant patients work functioning is not completely restored. Therefore, clinicians should communicate about their patients’ work situation, potential problems and support needs, and refer them for occupational counseling where needed. Furthermore, person-centered nephrology care, integrating CKD treatment and work, and individual tailoring of workplace accommodations may facilitate work functioning. Lastly, vocational rehabilitation programs or interventions should be developed to enable sustainable employment of CKD patients.
Data availability
The dataset generated and analyzed during the current study are available from the corresponding author on reasonable request.
References
Van Manen JG, Korevaar JC, Dekker FW, Reuselaars MC, Boeschoten EW, Krediet RT (2001) Changes in employment status in end-stage renal disease patients during their first year of dialysis. Perit Dial Int 21(6):595–601
Tappe K, Turkelson C, Doggett D, Coates V (2001) Disability under Social Security for patients with ESRD: an evidence-based review. Disabil Rehabil 23(5):177–185. https://doi.org/10.1080/09638280151080522
D’Egidio V, Mannocci A, Ciaccio D, Sestili C, Cocchiara RA, Del Cimmuto A, La Torre G (2019) Return to work after kidney transplant: a systematic review. Occup Med 69(6):412–418. https://doi.org/10.1093/occmed/kqz095
Van der Mei SF, Kuiper D, Groothoff JW, van den Heuvel WJ, van Son WJ, Brouwer S (2011) Long-term health and work outcomes of renal transplantation and patterns of work status during the end-stage renal disease trajectory. J Occup Rehabil 21(3):325–334. https://doi.org/10.1007/s10926-011-9317-1
Neri L, Gallieni M, Cozzolino M, Rocca-Rey L, Brambilla G, Colombi A, Foà V, Brancaccio D (2005) Work ability and health status in dialysis patients. Int J Artif Organs 28(6):554–556. https://doi.org/10.1177/039139880502800603
Klabbers C, Rooijackers B, Goertz B, De Rijk A (2014) Powerful and vulnerable: a study on work and social participation of people with chronic diseases and disabilities [Krachtig en kwetsbaar: onderzoek naar de ervaringen met arbeidsparticipatie en sociale participatie van mensen met chronische ziekten en beperkingen]. Maastricht University, Maastricht
Miraglia M, Johns G (2016) Going to work ill: a meta-analysis of the correlates of presenteeism and a dual-path model. J Occup Health Psychol 21(3):261–283. https://doi.org/10.1037/ocp0000015
Van der Mei SF, Alma MA, de Rijk AE, Brouwer S, Gansevoort RT, Franssen CFM, Bakker SJL, Hemmelder MH, Westerhuis R, van Buren M, Visser A (2021) Barriers to and facilitators of sustained employment: a qualitative study of experiences in Dutch patients with Chronic Kidney Disease (CKD). Am J Kidney Dis 78(6):780–792. https://doi.org/10.1053/j.ajkd.2021.04.008
Rajkunmar R, Baumgart A, Martin A et al (2022) Perspectives on ability to work from patients’ receiving dialysis and caregivers: analysis of data from the global SONG initiative. J Nephrol 35(1):255–266. https://doi.org/10.1007/s40620-021-01105-y
Carter SA, Gutman T, Logeman C, Cattran D, Lightstone L, Bagga A, Barbour SJ, Barratt J, Boletis J, Caster D, Coppo R, Fervenza FC, Floege J, Hladunewich M, Hogan JJ, Kitching AR, Lafayette RA, Malvar A, Radhakrishnan J, Rovin BH, Scholes-Robertson N, Trimarchi H, Zhang H, Azukaitis K, Cho Y, Viecelli AK, Dunn L, Harris D, Johnson DW, Kerr PG, Laboi P, Ryan J, Shen JI, Ruiz L, Wang AY, Lee AHK, Fung S, Tong MK, Teixeira-Pinto A, Wilkie M, Alexander SI, Craig JC, Tong A (2020) Identifying outcomes important to patients with glomerular disease and their caregivers. Clin J Am Soc Nephrol 15(5):673–684. https://doi.org/10.2215/CJN.13101019
Awan AA, Zhao B, Anumudu SJ, Winkelmayer WC, Ho V, Erickson KF (2020) Pre-ESKD nephrology care and employment at the start of dialysis. Kidney Int Rep 5(6):821–830. https://doi.org/10.1016/j.ekir.2020.03.004
Feder J, Nadel MV, Krishnan M (2016) A matter of choice: opportunities and obstacles facing people with ESRD. Clin J Am Soc Nephrol 11(3):536–538. https://doi.org/10.2215/CJN.0447041
Hays RD, Kallich JD, Mapes DL, Coons SJ, Carter WB (1994) Development of the kidney disease quality of life (KDQOL) instrument. Qual Life Res 3(5):329–338. https://doi.org/10.1007/BF00451725
Worm-Smeitink M, Gielissen M, Bloot L, van Laarhoven HWM, van Engelen BGM, van Riel P, Bleijenberg G, Nikolaus S, Knoop H (2017) The assessment of fatigue: psychometric qualities and norms for the Checklist individual strength. J Psychosom Res 98:40–46. https://doi.org/10.1016/j.jpsychores.2017.05.007
Statistics Netherlands. Accessed August 20, 2021. https://www.cbs.nl/nl-nl/onze-diensten/methoden/begrippen/werkzame-beroepsbevolking.
De Rijk A (2019) Work disability prevention the Netherlands: a key role for employers. In: MacEachen E (ed) The science and politics of work disability prevention. New York, Routledge, pp 223–241
Sandqvist JL, Henriksson CM (2004) Work functioning: a conceptual framework. Work 23(2):147–157
Tuomi K, Ilmarinen J, Jahkola A, Katajarinne L, Tulkki A (1998) Work ability index, 2nd edn. Finnish Institute of Occupational Health, Helsinki
Gould R, Koskinen S, Seitsamo J, Tuomi K, Polvinen A, Sainio P (2008) Data and methods. In: Gould R, Ilmarinen J, Järvisalo J, Koskinen S (eds) Dimensions of work ability results of the health 2000 survey. Finnish Centre for Pensions, Helsinki
Brouwer WB, Koopmanschap MA, Rutten FF (1999) Productivity losses without absence: measurement validation and empirical evidence. Health Policy 48(1):13–27. https://doi.org/10.1016/s0168-8510(99)00028-7
Clausen T, Madsen IE, Christensen KB, Bjorner JB, Poulsen OM, Maltesen T, Borg V, Rugulies R (2019) The Danish Psychosocial Work Environment Questionnaire (DPQ): development, content, reliability and validity. Scand J Work Environ Health 45(4):356–369. https://doi.org/10.5271/sjweh.3793
Statistics Netherlands: CBS Statline. Accessed August 20, 2021. https://opendata.cbs.nl/statline/#/CBS/nl/dataset/80590ned/table?dl=56E34.
Van der Mei SF, Krol B, Van Son WJ, De Jong PE, Groothoff JW, Van den Heuvel WJ (2006) Social participation and employment status after kidney transplantation: a systematic review. Qual Life Res 15(6):979–994. https://doi.org/10.1007/s11136-006-0045-5
Erickson KF, Zhao B, Ho V, Winkelmayer WC (2018) Employment among patients starting dialysis in the United States. Clin J Am Soc Nephrol 13(2):265–273. https://doi.org/10.2215/CJN.06470617
Maurits E, Rijken M, Friele R: Knowledge synthesis Chronic illness and work. Work participation of people with a chronic illness or physical disability [Kennissynthese Chronisch ziek en werk. Arbeidsparticipatie door mensen met een chronische ziekte of lichamelijke beperking]. 2013, Nivel: Utrecht
Volksgezondheidenzorg.info: Arbeidsongeschiktheid. Accessed August 20,2021. https://www.volksgezondheidenzorg.info/onderwerp/arbeidsongeschiktheid/cijfers-context/huidige-situatie#!node-prevalentie-arbeidsongeschiktheid-naar-geslacht.
Lundin A, Leijon O, Vaez M, Hallgren M, Torgén M (2017) Predictive validity of the Work Ability Index and its individual items in the general population. Scand J Public Health 45(4):350–356. https://doi.org/10.1177/1403494817702759
Schouten LS, Bültmann U, Heymans MW, Joling CI, Twisk JW, Roelen CA (2016) Shortened version of the work ability index to identify workers at risk of long-term sickness absence. Eur J Public Health 26(2):301–305. https://doi.org/10.1093/eurpub/ckv198
Canaud B, Kooman JP, Selby NM, Taal MW, Francis S, Maierhofer A, Kopperschmidt P, Collins A, Kotanko P (2020) Dialysis-induced cardiovascular and Multiorgan morbidity. Kidney Int Rep 5(11):1856–1869. https://doi.org/10.1016/j.ekir.2020.08.031
Tong A, Sainsbury P, Chadban S, Walker RG, Harris DC, Carter SM, Hall B, Hawley C, Craig JC (2009) Patients’ experiences and perspectives of living with CKD. Am J Kidney Dis 53(4):689–700. https://doi.org/10.1053/j.ajkd.2008.10.050
Schipper K, van der Borg WE, de Jong-Camerik J, Abma TA (2016) Living with moderate to severe renal failure from the perspective of patients. BMC Nephrol 17(1):48. https://doi.org/10.1186/s12882-016-0263-1
Hansen MS, Tesfaye W, Sewlal B, Mehta B, Sud K, Kairaitis L, Tarafdar S, Chau K, Zaidi ST, Castelino RL (2022) Psychosocial factors affecting patients with end-stage kidney disease and the impact of the social worker. J Nephrol 35(1):43–58. https://doi.org/10.1007/s40620-021-01098-8
Nevala N, Pehkonen I, Koskela I, Ruusuvuori J, Anttila H (2015) Workplace accommodation among persons with disabilities: a systematic review of its effectiveness and barriers or facilitators. J Occup Rehabil 25:432–448. https://doi.org/10.1007/s10926-014-9548-z
Acknowledgements
The authors gratefully thank all patients who participated in this study by completing the questionnaire. We thank the nephrology staff of the Dutch hospitals that contributed to the inclusion of patients (the University Medical Center Groningen, Dialysis Center Groningen, Medical Center Leeuwarden, Isala Hospital Zwolle, Radboud University Medical Center, Leiden University Medical Center, Catharina Hospital Eindhoven, Academic Medical Center Amsterdam, and HagaHospital The Hague). In addition, we gratefully acknowledge Louwine Bierma (Nurse Practitioner Medical Centre Leeuwarden) for assistance in recruitment of study participants, and Wim Sipma of the Dutch Kidney Patients Association for his cooperation in this study.
Funding
This study was supported by a grant from the Dutch Kidney Foundation (Social Kolff Grant, SWO14.01). The funding organization had no role in the study design, data collection, analysis, interpretation of data, writing of the report or the decision to submit the report for publication.
Author information
Authors and Affiliations
Contributions
Conceptuatlizon: SFM, SB, RTG, AV; Methodology: SFM, SB, RTG, AV; Investigation: MAA, SFM, AV; Formal analysis and investigation: MAA, SFM, AV; Writing—original draft preparation: MAA, SFM; Writing—review and editing: MAA, SFM, SB, LBH, PJMB, HU, FW, MH, RTG, AV; Funding acquisition: SFM, SB, RTG, AV; Resources: LBH, PJMB, HU, FW, MH, RTG; Supervision: SB, AV.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no relevant financial interests.
Ethical disclosure
This study was performed in line with the principles of the Declaration of Helsinki. Approval was granted by the Ethics Committee of the University Medical Center Groningen (M15.169470).
Informed consent
Informed consent was obtained from all individual participants included in the study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Alma, M.A., van der Mei, S.F., Brouwer, S. et al. Sustained employment, work disability and work functioning in CKD patients: a cross-sectional survey study. J Nephrol 36, 731–743 (2023). https://doi.org/10.1007/s40620-022-01476-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40620-022-01476-w