Abstract
Background
Gut-derived uremic toxins have been associated with adverse outcomes in chronic kidney disease (CKD). Alterations in bowel habits, including constipation, seem to play an additional role in uremic toxicity. The aim of this study is to investigate the association of bowel habits with gut-derived uremic toxins and intestinal permeability in patients on automated peritoneal dialysis (APD).
Methods
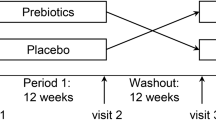
This cross-sectional study enrolled 58 APD patients (age 52.5 ± 15.1 years; dialysis vintage 14.1 (6.0–36.5) months). Constipation was defined according to the Rome IV criteria. Bowel habits were assessed by the Bristol Stool Scale (BSS < 3 characterized by hard consistency of stools and/or low frequency of evacuation, a surrogate of slow intestinal transit time, and BSS ≥ 3, defining regular bowel habit). The total and free serum concentration of p-cresyl sulfate (PCS), indoxyl sulfate (IS) and indole-3-acetic acid (IAA) were dosed by high-performance liquid chromatography. Lipopolysaccharide (LPS) and zonulin were assessed by ELISA and d(–)-lactate by colorimetric method. Dietary intake was assessed by the 3-day food records.
Results
No differences were observed in clinical, demographic, and dietary characteristics between constipated (n = 30) and non-constipated (n = 28) groups. A trend for higher total PCS (p = 0.07) and free PCS (p = 0.06) was found in constipated patients. Patients with BSS < 3 (n = 11) exhibited significantly higher levels of total and free PCS (p < 0.01) and total IAA (p = 0.04). Conversely, No difference was found in IS levels. Except for a lower serum level of d(–)-lactate in patients with BSS < 3 (p = 0.01), zonulin and LPS levels were not different.
Conclusions
Disturbed bowel habits, mainly characterized by slow transit time, may play a role in the accumulation of uremic toxins, particularly PCS, in patients on automatized peritoneal dialysis.

Similar content being viewed by others
References
Shirazian S, Radhakrishnan J (2010) Gastrointestinal disorders and renal failure: exploring the connection. Nat Rev Nephrol 6:480–492
Zuvela J, Trimingham C, Le Leu R, Faull R, Clayton P, Jesudason S, Meade A (2018) Gastrointestinal symptoms in patients receiving dialysis: a systematic review. Nephrology 23:718–727
Drossman DA (2016) Functional gastrointestinal disorders: history, pathophysiology, clinical features, and Rome IV. Gastroenterology 150:1262–1279
Lewis SJ, Heaton KW (1997) Stool form scale as a useful guide to intestinal transit time. Scand J Gastroenterol 32:920–924
Dennison C, Prasad M, Lloyd A, Bhattacharyya SK, Dhawan R, Coyne K (2005) The health-related quality of life and economic burden of constipation. Pharmacoeconomics 23:461–476
Lee A (2011) Constipation in patients on peritoneal dialysis: a literature review. Ren Soc Australas J 7:122–129
Ramos CI, Armani RG, Canziani ME, Ribeiro Dolenga CJ, Nakao LS, Campbell KL, Cuppari L (2020) Bowel habits and the association with uremic toxins in non-dialysis-dependent chronic kidney disease patients. J Ren Nutr 30:31–35
Nakabayashi I, Nakamura M, Kawakami K, Ohta T, Kato I, Uchida K, Yoshida M (2011) Effects of synbiotic treatment on serum level of p-cresol in haemodialysis patients: a preliminary study. Nephrol Dial Transpl 26:1094–1098
Evenepoel P, Meijers BKI, Bammens BRM, Verbeke K (2009) Uremic toxins originating from colonic microbial metabolism. Kidney Int 76:S12–S19
Cosola C, Rocchetti MT, Sabatino A, Fiaccadori E, Di Iorio BR, Gesualdo L (2019) Microbiota issue in CKD: how promising are gut-targeted approaches? J Nephrol 32:27–37
Watanabe H, Miyamoto Y, Honda D et al (2013) p-Cresyl sulfate causes renal tubular cell damage by inducing oxidative stress by activation of NADPH oxidase. Kidney Int 83:582–592
Jones JD, Burnett PC (1974) Creatinine metabolism in humans with decreased renal function: creatinine deficit. Clin Chem 20:1204–1212
Miyazaki T, Ise M, Seo H, Niwa T (1997) Indoxyl sulfate increases the gene expressions of TGF-beta 1, TIMP-1 and pro-alpha 1(I) collagen in uremic rat kidneys. Kidney Int Suppl 62:S15–S22
Adijiang A, Higuchi Y, Nishijima F, Shimizu H, Niwa T (2010) Indoxyl sulfate, a uremic toxin, promotes cell senescence in aorta of hypertensive rats. Biochem Biophys Res Commun 399:637–641
Bammens B, Evenepoel P, Keuleers H, Verbeke K, Vanrenterghem Y (2006) Free serum concentrations of the protein-bound retention solute p-cresol predict mortality in hemodialysis patients. Kidney Int 69:1081–1087
Liabeuf S, Barreto DV, Barreto FC, Meert N, Glorieux G, Schepers E, Temmar M, Choukroun G, Vanholder R, Massy ZA (2009) Free p-cresylsulphate is a predictor of mortality in patients at different stages of chronic kidney disease. Nephrol Dial Transpl 25:1183–1191
Vaziri ND, Zhao YY, Pahl MV (2016) Altered intestinal microbial flora and impaired epithelial barrier structure and function in CKD: the nature, mechanisms, consequences and potential treatment. Nephrol Dial Transpl 3:737–746
Fasano A (2011) Zonulin and its regulation of intestinal barrier function: the biological door to inflammation, autoimmunity, and cancer. Physiol Rev 91:151–175
Raetz CRH, Whitfield C (2002) Lipopolysaccharide endotoxins. Annu Rev Biochem 71:635–700
Ewaschuk JB, Naylor JM, Zello GA (2005) d-Lactate in human and ruminant metabolism. J Nutr 135:1619–1625
CANADA-USA, (CANUSA), Peritoneal, Dialysis Study Group (1996) Adequacy of dialysis and nutrition in continuous peritoneal dialysis: association with clinical outcomes. Canada-USA (CANUSA) Peritoneal Dialysis Study Group. J Am Soc Nephrol 7:198–207
Jennifer H, Ute N, Jean-Luc V, Arnold D, Marga O, Ulrich Harttig (2011) Estimating usual food intake distributions by using the multiple source method in the EPIC-potsdam calibration study. J Nutr 141:914–920
Willett WC, Howe GR, Kushi LH (1997) Adjustment for total energy intake in epidemiologic studies. Am J Clin Nutr 65:1220S–1228S
Tudor-Locke C, Bassett DR (2004) How many steps/day are enough? Preliminary pedometer indices for public health. Sports Med 34:1–8
Daugirdas JT (1993) Second generation logarithmic estimates of single-pool variable volume Kt/V: an analysis of error. J Am Soc Nephrol 4:1205–1213
Rodrigues SD, Santos SS, Meireles T, Romero N, Glorieux G, Pecoits-Filho R, Zhang DD, Nakao LS (2020) Uremic toxins promote accumulation of oxidized protein and increased sensitivity to hydrogen peroxide in endothelial cells by impairing the autophagic flux. Biochem Biophys Res Commun 523:123–129
Cummings JH, Macfarlane GT (1991) The control and consequences of bacterial fermentation in the human colon. J Appl Bacteriol 70:443–459
Birkett A, Muir J, Phillips J, Jones G, O’Dea K (1996) Resistant starch lowers fecal concentrations of ammonia and phenols in humans. Am J Clin Nutr 63:766–772
Poesen R, Mutsaers HAM, Windey K et al (2015) The influence of dietary protein intake on mammalian tryptophan and phenolic metabolites. PLoS One 10:e0140820
Rossi M, Johnson DW, Xu H, Carrero JJ, Pascoe E, French C, Campbell KL (2015) Dietary protein-fiber ratio associates with circulating levels of indoxyl sulfate and p-cresyl sulfate in chronic kidney disease patients. Nutr Metab Cardiovasc Dis 25:860–865
Roager HM, Hansen LBS, Bahl MI et al (2016) Colonic transit time is related to bacterial metabolism and mucosal turnover in the gut. Nat Microbiol 1:16093
Lin C, Pan C, Chuang C, Liu H, Sun F, Wang T, Chen H, Wu C (2013) Gastrointestinal-related Uremic toxins in peritoneal dialysis: a pilot study with a 5-year follow-up. Arch Med Res 44:535–541
Smith EA, Macfarlane GT (1996) Enumeration of human colonie bacteria producing phenolic and indolic compounds: effects of pH, carbohydrate availability and retention time on dissimilatory aromatic amino acid metabolism. J Appl Bacteriol 81:288–302
Gerritsen J, Smidt H, Rijkers GT, De Vos WM (2011) Intestinal microbiota in human health and disease: the impact of probiotics. Genes Nutr 6:209–240
Kirgizov IV, Sukhorukov AM, Dudarev VA, Istomin AA (2001) Hemostasis in children with dysbacteriosis in chronic constipation. Clin Appl Thromb Hemost 7:335–338
Poveda J, Sanchez-Niño MD, Glorieux G, Sanz AB, Egido J, Vanholder R, Ortiz A (2014) p-Cresyl sulphate has pro-inflammatory and cytotoxic actions on human proximal tubular epithelial cells. Nephrol Dial Transpl 29:56–64
Claro LM, Moreno-Amaral AN, Gadotti AC et al (2018) The impact of uremic toxicity induced inflammatory response on the cardiovascular burden in chronic kidney disease. Toxins (Basel) 10:384
Acknowledgements
This study was supported by the Oswaldo Ramos Foundation and Fundação de Amparo à Pesquisa do Estado de São Paulo (FAPESP 2018/12122-7). We thank Danilo Takashi Aoike for the statistical assistance; the Coordenação de Aperfeiçoamento de Pessoal de Nível Superior (CAPES) who provided scholarship and especially all the renal nurses, for their assistance in data collection.
Funding
NBFP received a scholarship from Coordenação de Aperfeiçoamento de Pessoal de Nível Superior (CAPES). CIR was supported by the Coordenação de Aperfeiçoamento de Pessoal de Nível Superior—CAPES, Brazil (88887.352924/2019-00). LC receives a scholarship from the Conselho Nacional de Desenvolvimento Científico e Tecnológico (CNPq) (302765/2017-4). Support for this research was provided by the Fundação de Amparo à Pesquisa do Estado de São Paulo (FAPESP 2018/12122-7).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
On behalf of all authors, the corresponding author states that there is no conflict of interest.
Ethical approval
Approval was obtained from the ethics committee of the Universidade Federal de São Paulo. The procedures used in this study adhere to the tenets of the Declaration of Helsinki.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Pereira, N.B.F., Ramos, C.I., de Andrade, L.S. et al. Influence of bowel habits on gut-derived toxins in peritoneal dialysis patients. J Nephrol 33, 1049–1057 (2020). https://doi.org/10.1007/s40620-020-00819-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40620-020-00819-9