Abstract
Monoclonal gammopathy of renal significance (MGRS) encompasses a group of disorders in which a monoclonal immunoglobulin (M-protein) secreted by a B-cell or plasma cell clone causes renal disease. Proliferative glomerulonephritis with monoclonal immunoglobulin deposits (PGNMID) is a form of MGRS where M-protein is deposited in the glomerulus. Although evidence is limited, the current consensus is that therapy for PGNMID should be directed against the underlying clone. However, it is conceivable that there is heterogeneity in the renal prognosis of PGNMID and that not all patients have need for clone-directed therapy. Here, we report two cases of PGNMID with IgM-kappa gammopathy. In one case of a 53-year-old woman the glomerulonephritis resolved without clone-directed therapy. In the other case of a 34-year-old woman clone-directed therapy was discontinued due to adverse effects. Although no hematological response was achieved, the PGNMID resolved. In both cases there are no signs of a recurrent glomerulonephritis in over 3 years of follow-up. Here, we review the literature and suggest that some PGNMID patients have a favorable renal prognosis in whom clone-directed therapy can be withheld or postponed. Further research is warranted to yield predictors to identify these patients and to better understand the disease course of PGNMID.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The term monoclonal gammopathy of renal significance (MGRS) has been coined in 2012 to describe a group of renal disorders caused by a monoclonal immunoglobulin (M-protein) secreted by a nonmalignant plasma cell or B-cell clone [1,2,3]. Proliferative glomerulonephritis with monoclonal immunoglobulin deposits (PGNMID) is a form of MGRS affecting the glomerulus, often leading to chronic or end-stage kidney disease [4, 5]. Although evidence is limited, the current consensus is that therapy for PGNMID, similar as for other forms of MGRS, should be directed at the underlying clone with the goal to achieve deep hematological response and thereby improve the renal prognosis. However, it is conceivable that there is heterogeneity in the renal prognosis of PGNMID and that not all patients need to undergo this type of treatment. Here, we illustrate this by two cases of PGNMID and by summarizing the available literature.
Case 1
A 53-year-old woman visited our outpatient clinic because of a systemic lupus erythematosus (SLE)/Sjögren syndrome overlap. Her medication included low-dose prednisolone, hydroxychloroquine, and azathioprine. The latter was recently started as steroid-sparing approach. On a routine check-up 2 weeks after starting azathioprine, urinalysis showed 500 white blood cells (WBC), 300 red blood cells (RBCs)/μL, of which > 40% were dysmorphic, and 0.36 g protein/day. She had no clinical signs of a urinary tract infection and the urine culture was negative. Her serum creatinine level had gradually increased from 0.6 to 0.8 mg/dL in the previous 4 months. Repeat urinalysis 3 weeks later showed no WBCs, but the new onset glomerular hematuria persisted. Serum protein electrophoresis (SPE) and immunofixation revealed a non-quantifiable IgM-kappa M-protein. The serum free-light chain (FLC) ratio (kappa/lambda) was slightly elevated (2.04). Serum cryoglobulins were negative.
A kidney biopsy was indicative of a proliferative glomerulonephritis with monoclonal IgM-kappa deposits (Fig. 1a–d). Furthermore, a revision of a lip biopsy from a year before, which had confirmed the Sjögren syndrome diagnosis, showed 62% IgM positive plasma cells with predominance of kappa over lambda and PCR analysis using the IdentiClone IGH gene clonality assay (InVivoScribe Technologies) showed B-cell monoclonality. Bone marrow biopsy showed no infiltration of monoclonal B-cells or plasma cells, and the IdentiClone assay showed no B-cell clonality. Remarkably, 6 weeks after the kidney biopsy, the M-protein was no longer detectable on repeat measurements. Also, the urine sediment normalized and there was no further increase in the serum creatinine level. Hence, no clone-directed therapy was started. Her treatment regimen including azathioprine/prednisolone remained unchanged. Three years later, immunofixation again showed a non-quantifiable IgM-kappa M-protein. Immunofluorescence on a repeat kidney biopsy still showed mesangial IgM-deposits, but no more mesangial or endocapillary hypercellularity was seen (Fig. 1e–f). Up to the time of writing this report, the serum creatinine level remained stable and there was no hematuria or proteinuria.
Kidney biopsy and serum immunofixation electrophoresis of patient 1. a Biopsy at presentation: Light microscopy showed eight glomeruli of which one was globally and one subtotally sclerosed. The remaining glomeruli showed some mesangial proliferation (asterisk) and five glomeruli showed endocapillary hypercellularity (arrows). The extent of tubular atrophy and interstitial fibrosis was estimated at 10–20%. The arteries and arterioles showed no abnormalities. Congo red staining was negative. b Biopsy at presentation: Immunofluorescence showed granular staining in glomeruli for IgM (1+ to 2+) and C3c (2+), while IgG, IgA, kappa- and lambda-free light chains and C1q were negative (not shown). c Biopsy at presentation: Immunohistochemistry indicated more intense staining in glomeruli for kappa than for lambda. d Biopsy at presentation: Electron microscopy showed subtle deposits in the mesangium, and on the subendothelial and subepithelial side of the glomerular basement membrane (arrows). e Serum immunofixation electrophoresis shows IgM-kappa M-protein. f Biopsy after 3 years: light microscopy showed no more mesangial or endocapilary hypercellularity. g Biopsy after 3 years: Immunofluorescence still showed mesangial deposits of IgM and C3c
Case 2
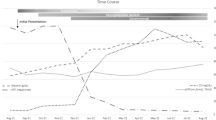
A 34-year-old woman presented with microscopic hematuria and proteinuria. Her medical history included a pharyngeal non-Hodgkin lymphoma at the age of 12 and immune thrombocytopenia purpura for which she had a splenectomy. Two years before, an IgM-kappa M-protein of 7 g/L was detected. Although she had thrombocytopenia, low complement levels and positivity for anti phospholipid antibodies, she did not meet the criteria for SLE. At presentation urinalysis showed 150 RBCs/μL (> 40% dysmorphic), RBC casts and 1.02 g protein/day. Serum creatinine was 0.8 mg/dL and the IgM-kappa M-protein level remained stable at 7 g/L. Kidney biopsy showed a proliferative glomerulonephritis with monoclonal IgM-kappa deposits (Fig. 2a–c). About 5% infiltration of IgM-kappa positive lymphoplasmacytic cells was seen in a bone marrow biopsy, the IdentiClone assay showed B-cell clonality. Given the diagnosis of PGNMID treatment with bortezomib, rituximab, and dexamethasone was initiated. The rituximab was discontinued after the first cycle because of adverse events. After receiving five cycles of bortezomib and dexamethasone the treatment was stopped because of progressive polyneuropathy. The M-protein had decreased to 4 g/L. Although no complete hematological response was achieved, the hematuria and proteinuria had resolved and the serum creatinine remained stable. Soon after discontinuation of the treatment the IgM-kappa M-protein progressed to the initial level of 7 g/L (Fig. 2d). As the M-protein level remained stable thereafter a watchful-waiting approach was taken. At the time of writing this report, over 3 years after the kidney biopsy, there are no signs of a recurrent glomerulonephritis.
Kidney biopsy and serum immunofixation electrophoresis of patient 2. a Light microscopy showed 13 glomeruli of which none was globally sclerosed. All glomeruli showed mild mesangial proliferation without signs of endocapillary hypercellularity. The extent of tubular atrophy and interstitial fibrosis was less than 10%. b Immunofluorescence showed intense granular staining in glomeruli for IgM (3+), C3c (1+ to 2+) and kappa (2+), while lambda was negative. c Electron microscopy showed subtle deposits in the mesangium (arrows). d Serum immunofixation electrophoresis showed IgM-kappa M-protein
Discussion
In PGNMID M-protein is deposited in the glomerulus, mostly causing membranoproliferative lesions, occasionally only with mesangial proliferation, on light microscopy [2, 5]. Immunofluorescence generally shows a granular staining pattern in the glomeruli restricted to a single immunoglobulin heavy chain (mostly IgG) and light chain subtype, and non-organized mesangial and subendothelial deposits can be seen in electron microscopy. While there is limited evidence, there is consensus that treatment of MGRS should target the underlying clone, since complete hematological response is associated with the best renal outcomes [1, 6]. However, in contrast to other forms of MGRS, the detection rate of serum M-protein in PGNMID is only 32–37% and a pathologic clone is found in a bone marrow biopsy in only 25–42% of cases [6,7,8]. Nonetheless, empirical treatment prescribed to target a hypothesized underlying clone is associated with renal response in cases without a detectable clone [6].
In case 1, the bone marrow biopsy showed no pathologic clone, but possibly the detected M-protein could have been produced by a precursor of a mucosa-associated lymphoid tissue (MALT)-lymphoma, given the abundant IgM-kappa positive plasma cells and the finding of B-cell monoclonality in the lip biopsy. MALT-lymphomas frequently produce M-protein, particularly IgM-kappa [9]. Even though no clone-directed treatment was given, the M-protein and the glomerulonephritis resolved. Previous studies show that in some patients with monoclonal gammopathy of undetermined significance (MGUS) the M-protein disappears without apparent cause [10, 11]. The probability of M-protein persistence seems to depend on the quantity, as in patients with a quantifiable M-protein only 0.4% disappeared spontaneously [10], whereas in patients with an M-protein without quantifiable M-spike 16% disappeared without immunomodulating treatment [11]. The fact that in the present case the M-protein was detectable again after 2 years strongly suggests that the responsible clone did not completely disappear. The question remains whether the M-protein disappeared spontaneously or that the prednisolone or azathioprine attenuated the PGNMID in an early stage. Renal response on immunosuppressive therapy has been described in various cases of MGRS, but small retrospective studies suggest that clone-directed regimens result in higher renal response rates [6, 12, 13].
In the second case, the PGNMID resolved even though no complete or sustained hematological response was achieved. Two similar cases with complete renal response while the M-protein was still detectable after clone-directed therapy were described in a recent case series [6], indicating that renal response is not contingent on the resolution of the M-protein in PGNMID. The fact that the M-protein increased to the pretreatment level without any signs of recurrent glomerulonephritis suggests that a factor besides the M-protein presence or quantity is involved in the development of PGNMID. Possibly, specific characteristics of the M-protein and its interaction with the patient’s immune system play a role. The question remains whether the trigger for PGNMID disappeared due to the clone-directed therapy or that it would have also disappeared without therapy. Either way, it challenges the current assumption that deep hematological response should be pursued with clone-directed therapy in order to achieve the most favorable renal outcome. In fact, other cases of PGNMID with favorable renal outcomes without receiving clone-directed therapy have been described [4, 6, 8]. Among 65 patients from three case series together with our patients (summarized in Table 1), 73% of the patients who received clone-directed therapy had complete or partial renal response, but also 54% of the patients who received steroids, mycophenolate mofetil and/or cyclosporine, and 29% of the patients who received no treatment or renin-angiotensin system-blockade alone achieved complete or partial renal responses [4, 6, 8]. While PGNMID typically presents with overt proteinuria [4, 6, 8], our patients had relatively mild proteinuria, which might be a predictor of favorable renal prognosis. The International Kidney and Monoclonal Gammopathy Research Group recommends careful surveillance in patients with stages 1 and 2 chronic kidney disease (CKD) without evidence of progression and proteinuria < 1 g/day [14]. However, there are also patients with more severe proteinuria who have complete renal response without clone-directed therapy (Table 1). As expected, severe interstitial fibrosis and tubular atrophy is related to worse renal outcome. Among patients with a clone, all who received clone-directed therapy showed renal response, whereas those who received non-directed therapy had no or partial renal response. In contrast, all patients without a detectable clone who were treated with non-directed therapy had partial or complete renal response. Of course, the small sample size and risk for confounding by indication limit the conclusions that can be made from these observational studies.
Both our patients had IgM deposits, whereas the majority of PGNMID patients have IgG deposits, which is a similar distribution as in MGUS [10]. Although the clinicopathologic characteristics, clone and serum M-protein detection rates do not significantly differ between IgG and non-IgG PGNMID [7], it is yet to be determined whether the type of immunoglobulin heavy chain affects the renal prognosis in PGNMID.
It remains a challenge to predict which patients with PGNMID have a favorable renal outcome without the need for clone-directed therapy. Future research into the pathophysiology and predictors of renal prognosis in PGNMID might help to allocate the right treatment to the right patient. Meanwhile, treatment for MGRS should be patient-tailored, preferably by consulting a multidisciplinary team consisting of nephrologists, hematologists and pathologists [3].
References
Leung N, Bridoux F, Hutchison CA et al (2012) Monoclonal gammopathy of renal significance: when MGUS is no longer undetermined or insignificant. Blood 120(22):4292–4295. https://doi.org/10.1182/blood-2012-07-445304
Bridoux F, Leung N, Hutchison CA et al (2015) Diagnosis of monoclonal gammopathy of renal significance. Kidney Int 87(4):698–711. https://doi.org/10.1038/ki.2014.408
Amaador K, Peeters H, Minnema MC et al (2019) Monoclonal gammopathy of renal significance (mgrs): Histopathologic classification, diagnostic workup, and therapeutic options. Neth J Med 77(7):243–254
Nasr SH, Satoskar A, Markowitz GS et al (2009) Proliferative glomerulonephritis with monoclonal IgG deposits. J Am Soc Nephrol 20(9):2055–2064. https://doi.org/10.1681/ASN.2009010110
Lusco MA, Fogo AB, Najafian B, Alpers CE (2016) AJKD atlas of renal pathology: proliferative glomerulonephritis with monoclonal immunoglobulin deposits. Am J Kidney Dis 67(3):e13–e15. https://doi.org/10.1053/j.ajkd.2016.01.003
Gumber R, Cohen JB, Palmer MB et al (2018) A clone-directed approach may improve diagnosis and treatment of proliferative glomerulonephritis with monoclonal immunoglobulin deposits. Kidney Int 94(1):199–205. https://doi.org/10.1016/j.kint.2018.02.020
Bhutani G, Nasr SH, Said SM et al (2015) Hematologic characteristics of proliferative glomerulonephritides with nonorganized monoclonal immunoglobulin deposits. Mayo Clin Proc 90(5):587–596. https://doi.org/10.1016/j.mayocp.2015.01.024
Kousios A, Duncan N, Tam FWK et al (2019) Proliferative glomerulonephritis with monoclonal Ig deposits (PGNMID): diagnostic and treatment challenges for the nephrologist! Kidney Int 95(2):467–468. https://doi.org/10.1016/j.kint.2018.10.016
Wöhrer S, Streubel B, Bartsch R, Chott A, Raderer M (2004) Monoclonal immunoglobulin production is a frequent event in patients with mucosa-associated lymphoid tissue lymphoma. Clin Cancer Res 10(21):7179–7181. https://doi.org/10.1158/1078-0432.CCR-04-0803
Kyle RA, Therneau TM, Rajkumar SV et al (2002) A long-term study of prognosis in monoclonal gammopathy of undetermined significance. N Engl J Med 346(8):564–569. https://doi.org/10.1056/NEJMoa01133202
Murray DL, Seningen JL, Dispenzieri A et al (2012) Laboratory persistence and clinical progression of small monoclonal abnormalities. Am J Clin Pathol 138(4):609–613. https://doi.org/10.1309/AJCPT6OWWMHITA1Y
Kourelis TV, Nasr SH, Dispenzieri A et al (2016) Outcomes of patients with renal monoclonal immunoglobulin deposition disease. Am J Hematol 91(11):1123–1128. https://doi.org/10.1002/ajh.24528
Chauvet S, Frémeaux-Bacchi V, Petitprez F et al (2017) Treatment of B-cell disorder improves renal outcome of patients with monoclonal gammopathy-associated C3 glomerulopathy. Blood 129(11):1437–1447. https://doi.org/10.1182/blood-2016-08-737163
Fermand JP, Bridoux F, Kyle RA et al (2013) How I treat monoclonal gammopathy of renal significance (MGRS). Blood 122(22):3583–3590. https://doi.org/10.1182/blood-2013-05-495929
Funding
No support/funding was received for this work.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Research involving human participants and/or animals
This article does not contain any studies with human participants or animals performed by any of the authors.
Informed consent
The patients that are described in the case reports have given their consent for publication.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
van Kruijsdijk, R.C.M., Abrahams, A.C., Nguyen, T.Q. et al. Clone-directed therapy for proliferative glomerulonephritis with monoclonal immunoglobulin depositions: is it always necessary?. J Nephrol 33, 611–617 (2020). https://doi.org/10.1007/s40620-020-00723-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40620-020-00723-2