Abstract
Background
Elevated serum phosphorus level is a risk factor for progression of chronic kidney disease in non-dialysis patients. However, the association of serum phosphorus level with residual renal function (RRF) loss among incident continuous ambulatory peritoneal dialysis (CAPD) patients remains unclear.
Methods
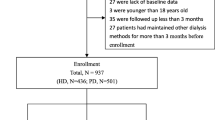
We performed a retrospective analysis of prospectively collected cohort of 1245 incident CAPD patients from January 2006 to December 2015 and followed up until December 2017. Patients were stratified into tertiles according to baseline serum phosphorus levels. RRF loss was defined as residual glomerular filtration rate (mL/min/1.73 m2) reaching zero or estimated urine output less than 200 mL/day on two successive clinic visits. Propensity-score matched Cox’s proportional hazards and competing risk models were performed to examine the association of serum phosphorus with RRF loss.
Results
A total of 421 (33.82%) patients had loss of RRF over a median follow-up of 26.23 months. In the entire cohort, elevated serum phosphorus was associated with increased risk for RRF loss after adjustment. In the propensity-score matched cohort, patients in the 3rd tertile of serum phosphorus had a 51% higher risk of RRF loss than those in the combination of the 1st and 2nd tertiles. Furthermore, the association of serum phosphorus level with RRF loss differed by sex (interaction P = 0.018). The adjusted HRs per 1 mg/dL increase in serum phosphorus level of RRF loss were 1.32 (95% CI 1.15–1.50, P < 0.001) for male and 1.03 (95% CI 0.87–1.21, P = 0.750) for female, respectively. These findings persisted in competing risk analysis.
Conclusion
Higher serum phosphorus levels independently predicts RRF loss in men treated with CAPD.




Similar content being viewed by others
References
Shafi T, Jaar BG, Plantinga LC, Fink NE, Sadler JH, Parekh RS, Powe NR, Coresh J (2010) Association of residual urine output with mortality, quality of life, and inflammation in incident hemodialysis patients: the Choices for Healthy Outcomes in Caring for End-Stage Renal Disease (CHOICE) Study. Am J Kidney Dis 56(2):348–358. https://doi.org/10.1053/j.ajkd.2010.03.020
Toth-Manikowski SM, Sirich TL, Meyer TW, Hostetter TH, Hwang S, Plummer NS, Hai X, Coresh J, Powe NR, Shafi T (2019) Contribution of ‘clinically negligible’ residual kidney function to clearance of uremic solutes. Nephrol Dial Transplant. https://doi.org/10.1093/ndt/gfz042
Mathew AT, Fishbane S, Obi Y, Kalantar-Zadeh K (2016) Preservation of residual kidney function in hemodialysis patients: reviving an old concept. Kidney Int 90(2):262–271. https://doi.org/10.1016/j.kint.2016.02.037
Obi Y, Rhee CM, Mathew AT, Shah G, Streja E, Brunelli SM, Kovesdy CP, Mehrotra R, Kalantar-Zadeh K (2016) Residual kidney function decline and mortality in incident hemodialysis patients. J Am Soc Nephrol 27(12):3758–3768. https://doi.org/10.1681/asn.2015101142
Krediet RT (2017) Preservation of residual kidney function and urine volume in patients on dialysis. Clin J Am Soc Nephrol 12(3):377–379. https://doi.org/10.2215/CJN.00330117
Wang AY, Lai KN (2006) The importance of residual renal function in dialysis patients. Kidney Int 69(10):1726–1732. https://doi.org/10.1038/sj.ki.5000382
Perl J, Bargman JM (2009) The importance of residual kidney function for patients on dialysis: a critical review. Am J Kidney Dis 53(6):1068–1081. https://doi.org/10.1053/j.ajkd.2009.02.012
Schwarz S, Trivedi BK, Kalantar-Zadeh K, Kovesdy CP (2006) Association of disorders in mineral metabolism with progression of chronic kidney disease. Clin J Am Soc Nephrol 1(4):825–831. https://doi.org/10.2215/CJN.02101205
O’Seaghdha CM, Hwang SJ, Muntner P, Melamed ML, Fox CS (2011) Serum phosphorus predicts incident chronic kidney disease and end-stage renal disease. Nephrol Dial Transplant 26(9):2885–2890. https://doi.org/10.1093/ndt/gfq808
De Nicola L, Conte G, Chiodini P, D’Angio P, Donnarumma G, Minutolo R (2014) Interaction between phosphorus and parathyroid hormone in non-dialysis CKD patients under nephrology care. J Nephrol 27(1):57–63. https://doi.org/10.1007/s40620-013-0001-8
Thongprayoon C, Cheungpasitporn W, Mao MA, Sakhuja A, Erickson SB (2018) Admission hyperphosphatemia increases the risk of acute kidney injury in hospitalized patients. J Nephrol 31(2):241–247. https://doi.org/10.1007/s40620-017-0442-6
Kasiske BL, Lakatua JD, Ma JZ, Louis TA (1998) A meta-analysis of the effects of dietary protein restriction on the rate of decline in renal function. Am J Kidney Dis 31(6):954–961. https://doi.org/10.1053/ajkd.1998.v31.pm9631839
Fouque D, Laville M (2009) Low protein diets for chronic kidney disease in non diabetic adults. Cochrane Database Systematic Rev. https://doi.org/10.1002/14651858.cd001892.pub3
Yoon CY, Park JT, Jhee JH, Noh J, Kee YK, Seo C, Lee M, Cha MU, Kim H, Park S, Yun HR, Jung SY, Han SH, Yoo TH, Kang SW (2017) High dietary phosphorus density is a risk factor for incident chronic kidney disease development in diabetic subjects: a community-based prospective cohort study. Am J Clin Nutr 106(1):311–321. https://doi.org/10.3945/ajcn.116.151654
Coladonato JA (2005) Control of hyperphosphatemia among patients with ESRD. J Am Soc Nephrol 16(Suppl 2):S107–S114. https://doi.org/10.1681/asn.2005060663
He L, Liu X, Li Z, Abreu Z, Malavade T, Lok CE, Bargman JM (2016) Rate of decline of residual kidney function before and after the start of peritoneal dialysis. Perit Dial Int 36(3):334–339. https://doi.org/10.3747/pdi.2016.00024
Noordzij M, Voormolen NM, Boeschoten EW, Dekker FW, Bos WJ, Krediet RT, Korevaar JC, Group Ns (2009) Disordered mineral metabolism is not a risk factor for loss of residual renal function in dialysis patients. Nephrol Dial Transplant 24(5):1580–1587. https://doi.org/10.1093/ndt/gfn768
Bai W, Li J, Liu J (2016) Serum phosphorus, cardiovascular and all-cause mortality in the general population: a meta-analysis. Clin Chim Acta 461:76–82. https://doi.org/10.1016/j.cca.2016.07.020
Moist LM, Port FK, Orzol SM, Young EW, Ostbye T, Wolfe RA, Hulbert-Shearon T, Jones CA, Bloembergen WE (2000) Predictors of loss of residual renal function among new dialysis patients. J Am Soc Nephrol 11(3):556–564
de Jager DJ, Halbesma N, Krediet RT, Boeschoten EW, le Cessie S, Dekker FW, Grootendorst DC (2013) Is the decline of renal function different before and after the start of dialysis? Nephrol Dial Transplant 28(3):698–705. https://doi.org/10.1093/ndt/gfs578
Noordzij M, Leffondre K, van Stralen KJ, Zoccali C, Dekker FW, Jager KJ (2013) When do we need competing risks methods for survival analysis in nephrology? Nephrol Dial Transplant 28(11):2670–2677. https://doi.org/10.1093/ndt/gft355
Sim JJ, Bhandari SK, Smith N, Chung J, Liu IL, Jacobsen SJ, Kalantar-Zadeh K (2013) Phosphorus and risk of renal failure in subjects with normal renal function. Am J Med 126(4):311–318. https://doi.org/10.1016/j.amjmed.2012.08.018
Bellasi A, Mandreoli M, Baldrati L, Corradini M, Di Nicolo P, Malmusi G, Santoro A (2011) Chronic kidney disease progression and outcome according to serum phosphorus in mild-to-moderate kidney dysfunction. Clin J Am Soc Nephrol 6(4):883–891. https://doi.org/10.2215/CJN.07810910
Voormolen N, Noordzij M, Grootendorst DC, Beetz I, Sijpkens YW, van Manen JG, Boeschoten EW, Huisman RM, Krediet RT, Dekker FW, Group Ps (2007) High plasma phosphate as a risk factor for decline in renal function and mortality in pre-dialysis patients. Nephrol Dial Transplant 22(10):2909–2916. https://doi.org/10.1093/ndt/gfm286
Smith DH, Johnson ES, Thorp ML, Petrik A, Yang X, Blough DK (2010) Outcomes predicted by phosphorous in chronic kidney disease: a retrospective CKD-inception cohort study. Nephrol Dial Transplant 25(1):166–174. https://doi.org/10.1093/ndt/gfp387
Chue CD, Edwards NC, Davis LJ, Steeds RP, Townend JN, Ferro CJ (2011) Serum phosphate but not pulse wave velocity predicts decline in renal function in patients with early chronic kidney disease. Nephrol Dial Transplant 26(8):2576–2582. https://doi.org/10.1093/ndt/gfq787
Cirillo M, Ciacci C, De Santo NG (2008) Age, renal tubular phosphate reabsorption, and serum phosphate levels in adults. N Engl J Med 359(8):864–866. https://doi.org/10.1056/NEJMc0800696
Ix JH, Chonchol M, Laughlin GA, Shlipak MG, Whooley MA (2011) Relation of sex and estrogen therapy to serum fibroblast growth factor 23, serum phosphorus, and urine phosphorus: the Heart and Soul Study. Am J Kidney Dis 58(5):737–745. https://doi.org/10.1053/j.ajkd.2011.06.011
Onufrak SJ, Bellasi A, Cardarelli F, Vaccarino V, Muntner P, Shaw LJ, Raggi P (2009) Investigation of gender heterogeneity in the associations of serum phosphorus with incident coronary artery disease and all-cause mortality. Am J Epidemiol 169(1):67–77. https://doi.org/10.1093/aje/kwn285
Yoo KD, Kang S, Choi Y, Yang SH, Heo NJ, Chin HJ, Oh KH, Joo KW, Kim YS, Lee H (2016) Sex, age, and the association of serum phosphorus with all-cause mortality in adults with normal kidney function. Am J Kidney Dis 67(1):79–88. https://doi.org/10.1053/j.ajkd.2015.06.027
Saab G, Whooley MA, Schiller NB, Ix JH (2010) Association of serum phosphorus with left ventricular mass in men and women with stable cardiovascular disease: data from the Heart and Soul Study. Am J Kidney Dis 56(3):496–505. https://doi.org/10.1053/j.ajkd.2010.03.030
Ibels LS, Alfrey AC, Haut L, Huffer WE (1978) Preservation of function in experimental renal disease by dietary restriction of phosphate. N Engl J Med 298(3):122–126. https://doi.org/10.1056/nejm197801192980302
Komaba H, Fukagawa M (2016) Phosphate-a poison for humans? Kidney Int 90(4):753–763. https://doi.org/10.1016/j.kint.2016.03.039
Razzaque MS (2011) Phosphate toxicity: new insights into an old problem. Clinical science (London, England: 1979) 120(3):91–97. https://doi.org/10.1042/cs20100377
Yamada S, Tokumoto M, Tatsumoto N, Taniguchi M, Noguchi H, Nakano T, Masutani K, Ooboshi H, Tsuruya K, Kitazono T (2014) Phosphate overload directly induces systemic inflammation and malnutrition as well as vascular calcification in uremia. Am J Physiol Renal Physiol 306(12):F1418–F1428. https://doi.org/10.1152/ajprenal.00633.2013
Funding
This work was supported by grants from the Guangzhou Committee of Science and Technology, China (2010U1-E00831), the PhD Start-up Fund of Natural Science Foundation of Guangdong Province, China (S2013040012953), Key Laboratory of Nephrology, Guangdong Province, Guangzhou, China (2002B60118), and Operational Grant of Guangdong Provincial Key Laboratory (2017B030314019).
Author information
Authors and Affiliations
Contributions
HPM, JNS and WL contributed to the study conception and design. JNS and WL performed analyses of data, interpretation of data and drafting manuscript. YTW, HYL, JLW, ZZ and YZK contributed to data collection and manuscript revision. HPM, XFH, and XQY provided overall supervision.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no competing interests.
Ethics approval and consent to participate
All participants provided written informed consents. The study was approved by the First Affiliated Hospital of Sun Yat-sen University Institutional Review Boards.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
40620_2019_670_MOESM1_ESM.docx
Supplementary material 1: Table S1. Clinical characteristics of PD Patients with different serum phosphorus levels before and after propensity score matching (DOCX 14 kb)
Rights and permissions
About this article
Cite this article
Shen, J., Li, W., Wang, Y. et al. Higher serum phosphorus predicts residual renal function loss in male but not female incident peritoneal dialysis patients. J Nephrol 33, 829–837 (2020). https://doi.org/10.1007/s40620-019-00670-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40620-019-00670-7