Abstract
Background
Acute kidney injury (AKI) after cardiac surgery is a common complication associated with increased mortality. However, the heterogeneity of the definitions used results in high variance of incidence rates in the literature. Data on the effect of diabetes mellitus on AKI incidence in this setting are scarce. We thus aimed to compare the incidence of AKI (defined by the AKIN, RIFLE and KDIGO criteria) in diabetic vs. non-diabetic patients undergoing cardiac surgery.
Methods
This is a nested case–control study from a cohort of patients undergoing cardiac surgery between 1/1/2013 and 30/6/2014 in a single center. Exclusion criteria were: type-1 diabetes, end-stage renal disease, death during surgery and AKI prior to surgery. We identified 199 type-2 diabetic patients and matched them for gender, age and estimated glomerular filtration rate (eGFR) to 199 non-diabetic individuals. The incidence of AKI between the two groups was compared in the total population and in subgroups according to preoperative eGFR. Univariate and multivariate logistic regression analysis were conducted to identify factors associated with AKI.
Results
The incidence of AKI was moderately high, but similar between the two study groups (AKIN and KDIGO: 24.1 vs. 23.1 %; p = 0.906, RIFLE: 25.1 vs. 25,1 %; p = 1.000, in diabetics and non-diabetics respectively). A trend towards increased incidence of AKI from eGFR subgroup 1 to subgroup 3a was noted in diabetic patients (p = 0.04). No significant differences were detected between the two study groups within any eGFR subgroup studied. At multivariate analysis, age [per year increase: odds ratio (OR) 1.034, 95 % confidence interval (CI) 1.001–1.068] and duration of cardiopulmonary bypass [per minute increase: OR 1.009 (1.003–1.015)] were associated with AKI. Diabetes was not related to AKI development in regression analysis [OR 1.057 (0.666–1.679)].
Conclusions
Incidence of AKI after cardiac surgery is high, but diabetes is not a risk factor for AKI. Baseline renal function in diabetics is related inversely to the incidence of AKI. Age and cardiopulmonary bypass duration are independent predictors of cardiac surgery-associated AKI.
Similar content being viewed by others
Introduction
Cardiac surgery, with or without the use of cardiopulmonary bypass, is commonly associated with the onset of acute kidney injury (AKI) [1, 2]. In the literature, a number of different definitions have been used for AKI, a fact resulting in highly variant estimations of postoperative AKI incidence [3]. In general, about 3–30 % of patients undergoing cardiac surgery are reported to experience an acute drop in renal function postoperatively, and 1–5 % require extracorporeal renal replacement therapy [4]. Renal function deterioration after such operations is considered a serious complication, as testified by a prospective cohort study of 2488 patients in which occurrence of AKI led to a 4 % increase in all-cause hospital mortality [5]. Notably, observational data from a prospective cohort of 4118 patients who underwent cardiac and thoracic aortic surgery suggested that even mild increases of serum creatinine (≥0.5 mg/dl) within 48 h postoperatively were associated with a 6 % increase in adverse outcomes with regard to 30-day mortality [6]. In patients with more severe cardiac surgery-related AKI, requiring renal replacement therapy postoperatively, 30-day mortality rate can be as high as 58 % [7].
In order to optimize clinical decision-making and implement preventive strategies in cardiac surgery, predictive models for high-risk patient identification have been developed. The most widely used system is perhaps the European System for Cardiac Operative Risk Evaluation (EuroSCORE) I and its more recent modified version EuroSCORE II [8, 9]. These morbidity scores correlate strongly both with mortality and incidence of AKI in several studies [1, 5, 6]. Moreover, since researchers tried to cope with different definitions for AKI and the consequent problems, in previous years three definition and classification systems for AKI were developed, with small differences between them. In 2002, the Acute Dialysis Quality Initiative (ADQI) group introduced the RIFLE (Risk, Injury, Failure, Loss and End-stage renal disease) criteria for diagnosis and staging of AKI based on serum creatinine, estimated glomerular filtration rate (eGFR) and urine output changes [10]. In 2007, the Acute Kidney Injury Network (AKIN) proposed a RIFLE modification known as the AKIN criteria and 5 years later the most recent definition was proposed, in the 2012 Kidney Disease: Improving Global Outcomes (KDIGO) clinical practice guideline for AKI [11, 12].
The pathophysiologic mechanisms leading to AKI after cardiovascular operations are multiple and complex. Intraoperative hypotension, nephrotoxic agents used in anesthesia, postoperative cardiac complications that impair renal perfusion, hemolysis and atheroembolism are some of the possible causes of AKI [13]. Further, a synergistic role of other injury pathways during and after surgery, such as neurohormonal activation, inflammation, oxidative stress activated by kidney ischemia and reperfusion and several endogenous toxins, has been proposed [14, 15]. In addition to the above, preoperative non-controllable risk factors that impair the kidney autoregulatory mechanisms, such as older age, advanced atherosclerotic vascular disease, hypertension and left ventricular ejection fraction (EF) decrease, have been associated with higher incidence of AKI [13, 16]. Presence of chronic kidney disease (CKD) per se is independently correlated with the post-surgery occurrence of AKI and need for renal replacement therapy [17]. The extent of renal dysfunction (higher serum creatinine, lower eGFR) and renal injury (higher proteinuria) before cardiac surgery is associated with AKI incidence [17–19].
Diabetes mellitus (DM) is present in about 20–25 % of patients undergoing cardiac surgery [1, 5] and has been associated with an increase in post-surgery cardiovascular events in some, but not all, studies [20, 21]. No study so far has focused mainly on the effect of DM on AKI incidence after cardiac surgery and current data are contradictory; some studies showed a similar prevalence of DM between patients with and without occurrence of AKI [5, 22], whereas others indicated that DM is an independent predictor of AKI, among several studied factors [1, 19]. Thus, the aim of this study was to compare the incidence of AKI (defined by the AKIN, RIFLE and KDIGO criteria) in matched patients with and without DM undergoing cardiac surgery and to directly examine the effect of DM on AKI development in these individuals.
Materials and methods
Study design and population
This is a nested case–control study with both cases and controls deriving from a prospectively assembled cohort of patients undergoing elective, urgent or emergency cardiac surgery (coronary artery bypass grafting [CABG], aortic or mitral valve replacement, thoracic aortic aneurysm repair, aortic dissection repair, atrial septal defect closure or a combination of these procedures) during an 18-month period (from 1/1/2013 to 30/6/2014) in the Department of Cardiothoracic Surgery, Papanikolaou Hospital in Thessaloniki, Greece. Exclusion criteria were: (a) type-1 DM; (b) stage 5 renal disease (eGFR <15 ml/min/1.73 m2); (c) death during surgery; (d) ongoing AKI of any cause before surgery; (e) patients with missing data for the parameters studied. A total of 199 type-2 diabetic patients were identified and represented the cases. After the case group was formed, one of the investigators, blinded to patient data apart from matching parameters, selected an equal number of non-diabetic patients as controls, matched for gender, age (±5 years) and pre-surgery kidney function (eGFR values ± 5 ml/min/1.73 m2).
Data collection and definitions
Upon admission, demographic and anthropometric parameters were recorded for each patient, as well as existing risk factors and comorbidities, e.g. hypertension, dyslipidemia, DM, coronary heart disease, stroke, peripheral vascular disease, chronic obstructive pulmonary disease, heart failure according to the New York Heart Association (NYHA) classification, as well as pre-surgery use of diuretics or renin-angiotensin-aldosterone system (RAAS) inhibitors. Additional preoperative risk factors included in the EuroSCORE I and II models were recorded. Pre-surgery cardiac function was evaluated by echocardiography. Intraoperative parameters such as type of intervention, duration of intubation (hours), duration of cardiopulmonary bypass use (minutes) and use of intra-aortic balloon pump, as well as factors related to intensive care unit (ICU) hospitalization were recorded. Possible postoperative complications were documented in all study participants; e.g. postoperative myocardial infarction, onset of atrial fibrillation, deep sternal wound infection, ventilator-associated pneumonia, stroke, requirement for re-intubation or renal replacement therapy, persistent hemodynamic instability, septicemia and multiple organ dysfunction syndrome.
Renal function was estimated on the basis of a series of serum creatinine measurements before surgery (baseline), when the operation was finalized, as well as exactly 24 and 48 h after the baseline blood samples were acquired. The eGFR was calculated using the Modification of Diet in Renal Disease (MDRD) equation, as described elsewhere [23]. Patient’s urinary excretion rate was monitored every 6 h on the day of surgery and on a daily basis thereafter. Diagnosis of AKI was made separately with the use of RIFLE, AKIN and KDIGO criteria [24], which are depicted in Fig. 1. The period of observation was restricted to 48 h post-surgery. The incidence of AKI and requirement for renal replacement therapy were compared between the diabetic and non-diabetic patients in the total population and in subgroups of renal function, according to their eGFR levels prior to surgery (Group 1: ≥90 ml/min/1.73 m2; Group 2a: ≥75 < 90 ml/min/1.73 m2; Group 2b: ≥60 <75 ml/min/1.73 m2; Group 3a: ≥45 <60 ml/min/1.73 m2; Group 3b: ≥30 < 45 ml/min/1.73 m2). Patients with stage 4 CKD were very few (n = 4) and, thus, were not analyzed separately. A further analysis to examine the effect of CKD severity on AKI incidence was performed.
Statistical analysis
The Shapiro–Wilk test was applied to examine the normality of distribution for quantitative variables. Continuous variables are described as mean ± 1 standard deviation (SD) or median and range according to the normality of distribution, while categorical variables are described as frequency and percentage (n, %). Incidence of AKI, existing comorbidities, medication use, surgery and procedure related data, occurrence of post-operative complications, as well as laboratory parameters were compared between the two study groups with the Chi-square test or Fisher’s exact test for qualitative variables, and with Student’s t test or the Mann–Whitney test and analysis of variance (ANOVA) or Kruskal–Wallis test by ranks for quantitative variables. Moreover, uni- and multivariate logistic regression analysis was performed to evaluate the correlation of various demographic, clinical and laboratory characteristics with occurrence of AKI defined by the KDIGO criteria. Variables were tested for interactions and included in the multivariate model if p was <0.20 at the univariate analysis. The adjusted odd ratios (OR) are reported with 95 % confidence intervals (CI) and values of p < 0.05 (two-tailed) were considered statistically significant. Statistical analysis was performed with the 21st version of the Statistical Package for Social Sciences (SPSS Inc., Chicago, IL, USA).
Results
Baseline demographic and clinical characteristics
A total of 398 patients were included in this study, allocated into two equal groups (n = 199) based on the diagnosis of DM prior to study entry. Mean age of patients was 67 years (diabetics: 66.4 ± 9.1, non-diabetics: 67.4 ± 8.3, p = 0.289) and each group consisted of 164 males and 35 females. Pre-operative renal function, in means of serum creatinine and eGFR, was similar in the two groups (creatinine: diabetics: 1.10 ± 0.2, non-diabetics: 1.09 ± 0.2, p = 0.817; eGFR: diabetics: 68.3 ± 28.5, non-diabetics: 67.5 ± 16.1, p = 0.724). The only parameters that were significantly more prevalent in diabetic patients were hypertension (54 vs. 46 %, p = 0.013) and dyslipidemia (58.7 vs. 41.3 %, p = 0.010). EuroSCORE I was higher in non-diabetics (4.9 ± 4.6 vs. 5.8 ± 5.9, p = 0.084), but the difference was of borderline significance and its newer modification EuroSCORE II was similar (1.9 ± 1.7 vs. 2.1 ± 2.1, p = 0.353) in the two groups. The pre-surgery use of diuretics and RAAS inhibitors was higher in the diabetic patient group, but did not reach significant levels (Table 1).
Surgery-related factors
As shown in Table 2, there were differences in the types of operation performed between the two groups. CABG was performed more often in diabetics, while combined surgery was more frequent in non-diabetics. Intra-aortic balloon pump was used more often in non-diabetic patients (3.5 vs. 10.6 %, p = 0.010). However, duration both of cardiopulmonary bypass and of intubation did not differ significantly between groups (cardiopulmonary bypass: 100.3 ± 36.8 min in diabetics vs. 107.1 ± 45.2 min in non-diabetics, p = 0.319; duration of intubation: 10.8 ± 13.8 h in diabetics vs. 13.4 ± 29.7 h in non-diabetics, p = 0.263). The most common complications were the onset of atrial fibrillation (140 cases in total) and hemodynamic instability (25 cases in total). No differences in incidence rates of any post-surgery complications were noted between the two groups (Table 2).
Renal outcomes
Baseline creatinine and eGFR levels were, respectively, 1.1 ± 0.2 mg/dl and 68.3 ± 28.5 ml/min/1.73 m2 in diabetic vs. 1.09 ± 0.2 mg/dl and 67.5 ± 16.1 ml/min/1.73 m2 in non-diabetic patients (p = 0.817, and p = 0.724, accordingly). Similarly, creatinine and eGFR levels at the end of surgery, as well as 24 h and 48 h after the first blood sample acquisition did not differ between the two groups (Table 3). Urine excretion during the first day post-surgery (diabetics: 3553 ± 887 ml vs. non-diabetics: 3766 ± 822, p = 0.053) and post-surgery day 2 (diabetics: 2998 ± 1083 ml vs. non-diabetics: 3296 ± 1111, p = 0.013) were significantly lower in the diabetic patient group. A similar analysis conducted within each renal function category, as defined above, showed no significant changes between groups (data not shown).
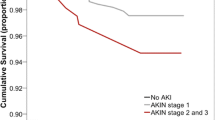
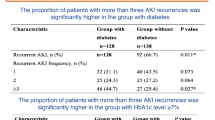
The incidence of AKI was moderately high, but also similar between the two study groups regardless of the set of criteria used. Defined by the AKIN criteria, incidence of AKI was 24.1 % (48 cases) in diabetic and 23.1 % (46 cases) in non-diabetic patients (p = 0.906) (Table 3). Using the RIFLE criteria, AKI was found in 25.1 % (50 cases) from each group (p = 1.000). With the KDIGO definition of AKI, the results were identical to those of the AKIN criteria (Table 3). Renal replacement therapy in the ICU was needed for 7 (3.5 %) diabetics and 3 (1.5 %) non-diabetics (p = 0.169). Notably, requirement for renal replacement therapy was significantly higher for diabetics in the renal function subgroup 2b (6.8 vs. 0 %, p = 0.022), but incidence rates and sample sizes in this comparison are relatively small. Moreover, there were no significant differences between diabetic and non-diabetic patients in AKI incidence with any definition used within each baseline renal function subgroup (Table 4).
We also analyzed the incidence of AKI and the need for renal replacement therapy in the ICU between baseline renal function categories in the study population as a whole and in the two study groups separately (Table 5). When AKIN or KDIGO criteria were used (identical results), a trend towards increased incidence of AKI from eGFR subgroup 1 to subgroup 3a was noted in the total study population; this trend was significant in diabetic patients, starting from 14.3 % in subgroup 1 and progressively increasing to 35.4 % in subgroup 3a (p = 0.04), but not in non-diabetic patients. With regard to renal replacement therapy, no particular trend was noted, apart from the fact that all non-diabetic patients in need of support were classified in subgroup 3a at baseline (p = 0.018).
Factors associated with AKI occurrence
The univariate and multivariate regression analysis in the total study population is shown in Table 5. Diabetes was clearly not correlated with the development of AKI in our study [OR 1.057 (95 % CI: 0.666–1.679)]. CKD severity defined by the aforementioned subgroups of renal function was associated with progressively increasing risk for AKI from group 1 to group 3a at univariate, but not multivariate analysis. Older age was independently associated with AKI occurrence both at univariate and multivariate [per year increase; OR 1.034 (1.001–1.068)] analysis. Another factor independently associated with elevated odds for AKI development was the duration of cardiopulmonary bypass use [per minute increase; OR 1.009 (1.003–1.015)]. EUROSCORE II score, total intubation time and occurrence of complications postoperatively displayed also significant ORs in the univariate analysis, but failed to reach statistical significance when adjusted for other factors.
Discussion
This study aimed to examine in comparison the incidence of AKI after cardiac surgery in matched diabetic and non-diabetic patients and to evaluate possible associations with factors that may contribute to its occurrence. The study included two groups of patients (diabetic and non-diabetic), carefully matched for age, gender and baseline renal function, that underwent cardiac surgery. As the sample size was relatively high, the two groups had almost no significant differences for a large set of demographic and clinical parameters studied, with the exception of hypertension and dyslipidemia, which cluster with type 2 diabetes within the setting of the metabolic syndrome [25]. Our main finding was that the prevalence of AKI as a whole was moderately high, but there were no differences between diabetic and non-diabetic patients with all three of the definitions used. This suggests that presence of DM is not a pre-disposing factor for AKI in individuals undergoing cardiac surgery.
Incidence of AKI after a cardiac operation in the population studied was 23.6 % based on the AKIN and the KDIGO criteria and 25.4 % based on the RIFLE criteria. In the literature, earlier studies, using definitions such as: (1) ≥25 % increase in serum creatinine by the third postoperative day or initiation of hemodialysis, or (2) postoperative decrease ≥10 % in creatinine clearance calculated with the Cockroft-Gault formula suggested incidence rates between 11 and 45 % [26–28]. With the development of new definitions, more reproducible data have become available. In a cohort study of about 25,000 patients undergoing cardiac surgery, over a period of 7 years, incidence rates of AKI were 30 % using the AKIN criteria and 31 % using the RIFLE criteria [29]. A study of 4836 individuals found a significantly higher incidence of AKI as defined by the AKIN criteria (26.3 %) than the RIFLE criteria (18.9 %) [30] while another study found an AKI incidence of 25.9 % with the AKIN and KDIGO criteria and of 24.9 % with RIFLE criteria [31]. Our findings are in general agreement with the above studies [3, 5, 29–31] and further support the significance of AKI as one of the most frequent postoperative complications in cardiac surgery, despite the development of predictive indices to identify high risk patients and the evolvement of a few protecting procedures, among various tried and showed to be ineffective [32].
The role of DM as a risk factor for AKI has not been conclusively determined. In non cardiac surgery settings, such as in 936 patients undergoing elective percutaneous coronary angioplasty, diabetes was a significant factor for AKI [33]. However, in a systematic review evaluating occurrence of AKI in patients undergoing transcatheter aortic valve implantation, DM was found as an independent predictor in 2 of the total 13 studies included [34]. Further, a meta-analysis including more than 1.2 million participants with general population characteristics and 80,000 CKD patients suggested that not the presence of DM per se but rather the presence of diabetic kidney injury (i.e. increased urine albumin excretion and particularly proteinuric diabetic nephropathy) were associated with increased occurrence of AKI [35]. The role of DM as a risk factor for renal function deterioration after cardiac surgery is much less studied. In a cohort study of 3219 patients who underwent cardiac surgery with cardiopulmonary bypass in a single center, DM was an independent predictor for AKI [OR 2.035 (1.172–3.534)], defined by the AKIN criteria [1]. Similarly, in a cohort of 995 patients DM was independently correlated with increased AKI incidence [OR 2.080 (1.080–4.040)] [3] defined as 50 % in eGFR. However, the use of suboptimal definitions for AKI may have affected these results. In contrast, in a retrospectively assembled cohort of 2488 patients, prevalence of diabetes was similar in patients with or without cardiac surgery-associated AKI defined by the RIFLE criteria and, thus, diabetes was not an independent predictor of AKI [5]. Similar were the findings in a multivariate analysis of a study in 267 patients undergoing aortic arch surgery [22]. Our study further clarifies this issue, as we found no significant differences between diabetic and non-diabetic patients, in the overall study population and when compared in subgroups based on preoperative renal function, in the incidence of AKI and need for renal replacement therapy in the ICU. Moreover, the uni- and multivariate logistic regression analysis performed did not indicate significant associations between DM and occurrence of AKI in the whole population studied.
Occurrence of post-surgery AKI and requirement of renal replacement therapy are considered established complications of CKD in the literature, possibly due to the impaired autoregulatory response of the kidneys [14]. Results from a cohort study including 964 patients with mean baseline eGFR 54 ml/min/1.73 m2 indicated an increasing risk for AKI and hemodialysis initiation with the progression of CKD from stage 1 towards stage 5; 7 % of the total population required renal replacement therapy and this rate was 75 % for patients at stage 5 [17]. Another observational study concluded that lower pre-operative eGFR values can independently predict the development of AKI defined by the AKIN and the RIFLE criteria [19]. In our study, progressive decline of renal function from CKD stage 1 to stage 3a was associated with higher post-surgery incidence of AKI with the AKIN and KDIGO definitions in both diabetic and non-diabetic patients. Regarding the results from the regression analysis, an interesting trend was noted with OR values gradually increasing from renal subgroup 1 towards 3a and slightly falling in subgroup 3b. With regard to other factors affecting incidence of AKI, an independent correlation with age was found, as noted in other observational studies [1, 5, 13]. Duration of cardiopulmonary bypass was also independently related to AKI development. Cardiopulmonary bypass during cardiac operations is believed to cause AKI through renal ischemia and reperfusion and it has been suggested that off-pump surgery, when indicated, may decrease this risk [15]. In most observational studies in the field, the mean time for cardiopulmonary bypass was significantly longer in those with AKI postoperatively [5, 30]. Results from a multicenter cohort study of 3500 patients indicated that for every 15-min increase of bypass time patients had an 11 % increased risk for AKI [14].
This study has strengths and limitations. Firstly, a direct comparison of carefully matched individuals was used to evaluate post cardiac surgery incidence of AKI in diabetic and non-diabetic patients with CKD. Secondly, as data from different studies are ambiguous, we examined AKI incidence using all three contemporary definitions of AKI. Lastly, our study included information on most of the possible factors affecting AKI incidence in the setting of cardiac surgery, following rigorous prospective recordings. However, this is still an observational study, and definite cause and effect associations cannot be established. The patients were not matched for type of surgery and this may have slightly affected the results, although almost all of many relevant factors (including target organ damage, EuroSCORE, cardiopulmonary bypass and intubation times) did not differ between groups. Lastly, the follow-up period was up to 48 h post-surgery, when all relevant data were routinely recorded for all patients.
In conclusion, this study shows that incidence of AKI after cardiac surgery remains relatively high, but diabetes mellitus does not constitute a separate risk factor for AKI development. This is in contrast to other settings, such as in patients undergoing percutaneous coronary angioplasty where DM increases the incidence of AKI significantly, possibly due to contrast-induced nephropathy. Among patients with DM, baseline renal function is the main parameter related inversely to the incidence of AKI. Age and cardiopulmonary bypass time are factors associated with AKI development in all patients. Thus, these are the factors that should be mainly considered when it comes to planning adequate measures for AKI prevention.
References
Parolari A, Pesce LL, Pacini D, Mazzanti V, Salis S, Sciacovelli C, Rossi F, Alamanni F (2012) Risk factors for perioperative acute kidney injury after adult cardiac surgery: role of perioperative management. Ann Thorac Surg 93(2):584–591
Sirvinskas E, Andrejaitiene J, Raliene L, Nasvytis L, Karbonskiene A, Pilvinis V, Sakalauskas J (2008) Cardiopulmonary bypass management and acute renal failure: risk factors and prognosis. Perfusion 23(6):323–327
Noyez L (2011) Influence of the definition of acute renal failure post-cardiac surgery on incidence, patient identification, and identification of risk factors. Eur J Cardiothorac Surg 39(3):e8–e12
Huen SC, Parikh CR (2012) Predicting acute kidney injury after cardiac surgery: a systematic review. Ann Thorac Surg 93(1):337–347
D’Onofrio A, Cruz D, Bolgan I, Auriemma S, Cresce GD, Fabbri A, Ronco C (2010) RIFLE criteria for cardiac surgery-associated acute kidney injury: risk factors and outcomes. Congest Heart Fail 16(Suppl 1):S32–S36
Lassnigg A, Schmidlin D, Mouhieddine M, Bachmann LM, Druml W, Bauer P, Hiesmayr M (2004) Minimal changes of serum creatinine predict prognosis in patients after cardiothoracic surgery: a prospective cohort study. J Am Soc Nephrol 15(6):1597–1605
Pistolesi V, Di Napoli A, Fiaccadori E, Zeppilli L, Polistena F, Sacco MI, Regolisti G, Tritapepe L, Pierucci A, Morabito S (2015) Severe acute kidney injury following cardiac surgery: short-term outcomes in patients undergoing continuous renal replacement therapy (CRRT). J Nephrol
Roques F, Nashef SA, Michel P, Gauducheau E, de Vincentiis C, Baudet E, Cortina J, David M, Faichney A, Gabrielle F, Gams E, Harjula A, Jones MT, Pintor PP, Salamon R, Thulin L (1999) Risk factors and outcome in European cardiac surgery: analysis of the EuroSCORE multinational database of 19030 patients. Eur J Cardiothorac Surg 15(6):816–822 (discussion 822-813)
Kuwaki K, Inaba H, Yamamoto T, Dohi S, Matsumura T, Morita T, Amano A (2015) Performance of the EuroSCORE II and the Society of Thoracic Surgeons Score in patients undergoing aortic valve replacement for aortic stenosis. J Cardiovasc Surg (Torino) 56(3):455–462
Bellomo R, Ronco C, Kellum JA, Mehta RL, Palevsky P (2004) Acute renal failure—definition, outcome measures, animal models, fluid therapy and information technology needs: the Second International Consensus Conference of the Acute Dialysis Quality Initiative (ADQI) Group. Crit Care 8(4):R204–R212
Mehta RL, Kellum JA, Shah SV, Molitoris BA, Ronco C, Warnock DG, Levin A (2007) Acute Kidney Injury Network: report of an initiative to improve outcomes in acute kidney injury. Crit Care 11(2):R31
Palevsky PM, Liu KD, Brophy PD, Chawla LS, Parikh CR, Thakar CV, Tolwani AJ, Waikar SS, Weisbord SD (2013) KDOQI US commentary on the 2012 KDIGO clinical practice guideline for acute kidney injury. Am J Kidney Dis 61(5):649–672
Rosner MH, Portilla D, Okusa MD (2008) Cardiac surgery as a cause of acute kidney injury: pathogenesis and potential therapies. J Intensive Care Med 23(1):3–18
Karkouti K, Wijeysundera DN, Yau TM, Callum JL, Cheng DC, Crowther M, Dupuis JY, Fremes SE, Kent B, Laflamme C, Lamy A, Legare JF, Mazer CD, McCluskey SA, Rubens FD, Sawchuk C, Beattie WS (2009) Acute kidney injury after cardiac surgery: focus on modifiable risk factors. Circulation 119(4):495–502
Bellomo R, Auriemma S, Fabbri A, D’Onofrio A, Katz N, McCullough PA, Ricci Z, Shaw A, Ronco C (2008) The pathophysiology of cardiac surgery-associated acute kidney injury (CSA-AKI). Int J Artif Organs 31(2):166–178
Chertow GM, Lazarus JM, Christiansen CL, Cook EF, Hammermeister KE, Grover F, Daley J (1997) Preoperative renal risk stratification. Circulation 95(4):878–884
Li SY, Chen JY, Yang WC, Chuang CL (2011) Acute kidney injury network classification predicts in-hospital and long-term mortality in patients undergoing elective coronary artery bypass grafting surgery. Eur J Cardiothorac Surg 39(3):323–328
Li SY, Chuang CL, Yang WC, Lin SJ (2015) Proteinuria predicts postcardiotomy acute kidney injury in patients with preserved glomerular filtration rate. J Thorac Cardiovasc Surg 149(3):894–899
Ko B, Garcia S, Mithani S, Tholakanahalli V, Adabag S (2012) Risk of acute kidney injury in patients who undergo coronary angiography and cardiac surgery in close succession. Eur Heart J 33(16):2065–2070
Conrotto F, D’Ascenzo F, Giordana F, Salizzoni S, Tamburino C, Tarantini G, Presbitero P, Barbanti M, Gasparetto V, Mennuni M, Napodano M, Rossi ML, La Torre M, Ferraro G, Omede P, Scacciatella P, Marra WG, Colaci C, Biondi-Zoccai G, Moretti C, D’Amico M, Rinaldi M, Gaita F, Marra S (2014) Impact of diabetes mellitus on early and midterm outcomes after transcatheter aortic valve implantation (from a multicenter registry). Am J Cardiol 113(3):529–534
Berkovitch A, Segev A, Barbash I, Grossman Y, Maor E, Erez A, Regev E, Fink N, Mazin I, Hamdan A, Goldenberg I, Hay I, Spiegelstien D, Guetta V, Fefer P (2015) Clinical impact of diabetes mellitus in patients undergoing transcatheter aortic valve replacement. Cardiovasc Diabetol 14(1):131
Arnaoutakis GJ, Bihorac A, Martin TD, Hess PJ, Jr., Klodell CT, Ejaz AA, Garvan C, Tribble CG, Beaver TM (2007) RIFLE criteria for acute kidney injury in aortic arch surgery. J Thorac Cardiovasc Surg 134(6):1554–1560 (discussion 1560–1551)
Levey AS, Bosch JP, Lewis JB, Greene T, Rogers N, Roth D (1999) A more accurate method to estimate glomerular filtration rate from serum creatinine: a new prediction equation. Modification of Diet in Renal Disease Study Group. Ann Intern Med 130(6):461–470
Fujii T, Uchino S, Takinami M, Bellomo R (2014) Validation of the Kidney Disease Improving Global Outcomes criteria for AKI and comparison of three criteria in hospitalized patients. Clin J Am Soc Nephrol 9(5):848–854
Alberti KG, Zimmet P, Shaw J (2006) Metabolic syndrome–a new world-wide definition. A Consensus Statement from the International Diabetes Federation. Diabet Med 23(5):469–480
Del Duca D, Iqbal S, Rahme E, Goldberg P, de Varennes B (2007) Renal failure after cardiac surgery: timing of cardiac catheterization and other perioperative risk factors. Ann Thorac Surg 84(4):1264–1271
van Straten AH, Hamad MA, van Zundert AA, Martens EJ, Schonberger JP, de Wolf AM (2010) Risk factors for deterioration of renal function after coronary artery bypass grafting. Eur J Cardiothorac Surg 37(1):106–111
Ronco C, Kellum JA, Bellomo R (2008) Cardiac surgery-associated acute kidney injury. Int J Artif Organs 31(2):156–157
Robert AM, Kramer RS, Dacey LJ, Charlesworth DC, Leavitt BJ, Helm RE, Hernandez F, Sardella GL, Frumiento C, Likosky DS, Brown JR (2010) Cardiac surgery-associated acute kidney injury: a comparison of two consensus criteria. Ann Thorac Surg 90(6):1939–1943
Englberger L, Suri RM, Li Z, Casey ET, Daly RC, Dearani JA, Schaff HV (2011) Clinical accuracy of RIFLE and Acute Kidney Injury Network (AKIN) criteria for acute kidney injury in patients undergoing cardiac surgery. Crit Care 15(1):R16
Bastin AJ, Ostermann M, Slack AJ, Diller GP, Finney SJ, Evans TW (2013) Acute kidney injury after cardiac surgery according to Risk/Injury/Failure/Loss/End-stage, Acute Kidney Injury Network, and Kidney Disease: improving Global Outcomes classifications. J Crit Care 28(4):389–396
Golestaneh L, Lindsey K, Malhotra P, Kargoli F, Farkas E, Barner H, Qazi R, Schmidt A, Rauchman M, Al-Aly Z, Johnson R, Martin K, Dagher P, Friedman A, El-Achkar TM (2015) Acute kidney injury after cardiac surgery: is minocycline protective? J Nephrol 28(2):193–199
Chen SL, Zhang J, Yei F, Zhu Z, Liu Z, Lin S, Chu J, Yan J, Zhang R, Kwan TW (2008) Clinical outcomes of contrast-induced nephropathy in patients undergoing percutaneous coronary intervention: a prospective, multicenter, randomized study to analyze the effect of hydration and acetylcysteine. Int J Cardiol 126(3):407–413
Elhmidi Y, Bleiziffer S, Deutsch MA, Krane M, Mazzitelli D, Lange R, Piazza N (2014) Acute kidney injury after transcatheter aortic valve implantation: incidence, predictors and impact on mortality. Arch Cardiovasc Dis 107(2):133–139
James MT, Grams ME, Woodward M, Elley CR, Green JA, Wheeler DC, de Jong P, Gansevoort RT, Levey AS, Warnock DG, Sarnak MJ (2015) A Meta-analysis of the Association of Estimated GFR, Albuminuria, Diabetes Mellitus, and Hypertension With Acute Kidney Injury. Am J Kidney Dis 66(4):602–612
Sources of support
This paper was not supported by any source and represents an original effort of the authors.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
All authors disclose that they do not have any conflict of interest.
Ethical approval
This is a retrospective study of patients’ routinely recorded data, approved by the Institutional Ethical Committee.
Informed consent
All study participants provided an informed consent for the use of their personal medical records.
Rights and permissions
About this article
Cite this article
Moschopoulou, M., Ampatzidou, F.C., Loutradis, C. et al. Diabetes mellitus does not affect the incidence of acute kidney injury after cardiac surgery; a nested case–control study. J Nephrol 29, 835–845 (2016). https://doi.org/10.1007/s40620-016-0281-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40620-016-0281-x