Abstract
Background
The novel iron-based phosphate binder sucroferric oxyhydroxide is being investigated for the treatment of hyperphosphatemia. Patients with chronic kidney disease often have multiple comorbidities that may necessitate the daily use of several types of medication. Therefore, the potential pharmacokinetic drug–drug interactions between sucroferric oxyhydroxide and selected drugs commonly taken by dialysis patients were investigated.
Methods
Five Phase I, single-center, open-label, randomized, three-period crossover studies in healthy volunteers investigated the effect of a single dose of sucroferric oxyhydroxide 1 g (based on iron content) on the pharmacokinetics of losartan 100 mg, furosemide 40 mg, omeprazole 40 mg, digoxin 0.5 mg and warfarin 10 mg. Pharmacokinetic parameters [including area under the plasma concentration–time curve (AUC) from time 0 extrapolated to infinite time (AUC0–∞) and from 0 to 24 h (AUC0–24)] for these drugs were determined: alone in the presence of food; with sucroferric oxyhydroxide in the presence of food; 2 h after food and sucroferric oxyhydroxide administration.
Results
Systemic exposure based on AUC0–∞ for all drugs, and AUC0–24 for all drugs except omeprazole (for which AUC 0–8 h was measured), was unaffected to a clinically significant extent by the presence of sucroferric oxyhydroxide, irrespective of whether sucroferric oxyhydroxide was administered with the drug or 2 h earlier.
Conclusions
There is a low risk of drug–drug interactions between sucroferric oxyhydroxide and losartan, furosemide, digoxin and warfarin. There is also a low risk of drug–drug interaction with omeprazole (based on AUC0–∞ values). Therefore, sucroferric oxyhydroxide may be administered concomitantly without the need to adjust the dosage regimens of these drugs.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
One of the serious and common clinical consequences of chronic kidney disease (CKD) is hyperphosphatemia, which is associated with CKD-mineral bone disorder [1], and increased risk of cardiovascular events [2] and mortality [3–6]. As a result, patients on dialysis often require phosphate binding agents to control serum phosphorus concentrations.
The novel polynuclear iron (III)-oxyhydroxide phosphate binder sucroferric oxyhydroxide is being investigated for the treatment of hyperphosphatemia. It is formulated as a chewable tablet that may be taken without water. In Phase I clinical studies, sucroferric oxyhydroxide was shown to be associated with minimal iron absorption through the gastrointestinal (GI) tract, and to be well tolerated [7, 8]. A Phase II dose-finding study demonstrated that sucroferric oxyhydroxide doses of 1.0–2.5 g/day (based on iron content) significantly lowered serum phosphorus concentrations [9]. A Phase III study in patients with hyperphosphatemia undergoing hemo- or peritoneal dialysis was recently undertaken [10]. In this study, patients (n = 1,059) were randomized to receive sucroferric oxyhydroxide 1.0–3.0 g/day or sevelamer 4.8–14.4 g/day. It was shown that sucroferric oxyhydroxide was non-inferior to sevelamer in terms of serum phosphorus control over the first 12 weeks of treatment, maintained its phosphorus-lowering effect over 52 weeks with a lesser pill burden than sevelamer, and was associated with reduced non-adherence to treatment [10, 11].
Patients with CKD often have multiple comorbidities, including cardiovascular disease, hypertension and diabetes, which may necessitate the use of several different types of daily medications [12, 13]. In vitro studies have identified a few potential interactions between sucroferric oxyhydroxide and some common medications (unpublished data) prescribed to patients with CKD. Therefore, a program of human in vivo pharmacokinetic (PK) drug–drug interaction (DDI) studies between sucroferric oxyhydroxide and several common medications was undertaken. Here we report data from five separate Phase I clinical DDI studies undertaken in healthy adults of sucroferric oxyhydroxide administered with medications selected based on adsorption of these medications onto sucroferric oxyhydroxide from in vitro investigations. Digoxin and warfarin did not show interactions in the in vitro investigations, but were chosen due to their narrow therapeutic window. The primary objective of these studies was to assess whether there was any effect of sucroferric oxyhydroxide on medication exposure [area under the plasma concentration–time curve from time 0–24 h (AUC0–24); AUC from time 0 extrapolated to infinite time (AUC0–∞); peak serum concentration (Cmax); time to Cmax (Tmax) and terminal half-life (t1/2)]. Adverse event profiles and routine biochemical/hematological laboratory tests were also assessed.
Subjects and methods
Study design and interventions
Five Phase I, single-center, open-label, randomized, three-period crossover studies investigated the PK effect of sucroferric oxyhydroxide (single dose of 1 g, based on iron content) on the following medications: losartan potassium (Cozaar® 100 mg), furosemide (Lasix® 40 mg), omeprazole (Prilosec® 40 mg), digoxin (Lanoxin® 0.5 mg) and warfarin (Coumadin® 10 mg). The doses of these drugs are based on the approved doses and those that are commonly used in clinical practice and/or have been used in PK interaction studies. The dose of sucroferric oxyhydroxide is the maximum single dose proposed for clinical use. Each study comprised a screening visit, 12 safety and PK visits, two washout periods (7 days each) and one follow-up visit 2 weeks after the last administration of study medication.
Subjects were randomized (1:1:1) to one of three treatment groups by sequentially following a randomization code list. Treatment Group 1 began with ‘Schedule 1’ dosing, Treatment Group 2 began with ‘Schedule 2’ dosing, and Treatment Group 3 began with ‘Schedule 3’ dosing (Table 1). After a 7-day washout period, subjects from Treatment Group 1 crossed over to receive ‘Schedule 2’ dosing, Treatment Group 2 crossed over to receive ‘Schedule 3’ dosing, and Treatment Group 3 crossed over to receive ‘Schedule 1’ dosing. After a further 7-day washout period, subjects from Treatment Group 1 crossed over to receive ‘Schedule 3’ dosing, Treatment Group 2 crossed over to receive ‘Schedule 1’ dosing, and Treatment Group 3 crossed over to receive ‘Schedule 2’ dosing.
Participants
Subjects eligible for these studies were healthy male or female volunteers aged 20–50 years, and with a body mass index of 18–32 kg/m2. The subjects had to provide written informed consent before the commencement of any study-specific procedures. All protocols were approved by an independent Review Board. Subjects were ineligible for the studies if they had participated in a clinical trial with an investigational drug or device ≤3 months before screening, if they had a history of clinically significant disorders or drug hypersensitivity, had a history of recurrent infectious diseases or major illness ≤30 days before screening, used nicotine ≤30 days before Study Day −1, presented with clinically significant abnormal findings on any screening assessments, took any medication ≤2 weeks before Study Day −1, had a clinically relevant history of drug or alcohol misuse, suffered any significant blood loss or blood donation ≤3 months before Study Day −1, or if they were pregnant or did not use adequate contraceptive precautions. No non-study medications, nicotine, alcohol or drugs of abuse were permitted during the study.
Outcomes
The primary endpoints of the studies were AUC0–24, AUC0–∞, Cmax, Tmax, and t1/2 for each of the study medications. These endpoints were analyzed for the two active enantiomers of warfarin (R- and S-forms) and also for the active metabolite of losartan (EXP 3174). Safety endpoints included adverse events and routine biochemical/hematological laboratory tests.
Sample sizes
For the studies involving losartan and furosemide, 36 and 42 subjects, respectively, were considered to be adequate in terms of demonstrating bioequivalence for the primary analysis of AUC0–24, and the sample sizes were not based on statistical assumptions.
For the omeprazole and digoxin studies, a total of 36 evaluable subjects each was judged to be sufficient to demonstrate the equivalence in a crossover design with a power of 84 %, considering a standard deviation (SD) of the difference of 0.43 (in the log scale), a 1-sided α of 0.05, an expected ratio of 1, and the bioequivalence limits of 80–125 %.
For the warfarin study, at least 36 evaluable subjects were considered sufficient to demonstrate the bioequivalence in a crossover design with a power of more than 95 %, considering a SD of the difference of 0.35 (in the log scale), a 1-sided α of 0.05, an expected ratio of 1, and the bioequivalence limits of 80–125 %.
Statistical methods
PK parameters were calculated using non-compartmental methods with WinNonlin® Professional Version 5.1.1 or higher (Pharsight Corp., Mountain View, CA, USA). PK computations were performed in SAS® Version 9.1 or higher. The plasma PK parameters were estimated from the concentration–time profiles for all PK population subjects. In estimating the PK parameters, values that were below the lower limit of quantification (LLOQ) at the beginning of the profile were set to 0. Lower limit of quantification values that occurred after the first quantifiable point were considered missing. Values that were embedded between LLOQs, or quantifiable values occurring after two or more LLOQs, were set to missing at the discretion of the pharmacokineticist. Descriptive statistics were used to summarize the calculated PK parameters by treatment. Missing PK parameter data were not imputed. Tmax and t1/2 were analyzed using the nonparametric Wilcoxon signed-rank test. To assess the effect of sucroferric oxyhydroxide on the PK of test medications (or the active metabolite), an analysis of variance (ANOVA) with fixed treatment, period, sequence, and subject within sequence was applied to natural logarithm-transformed AUC0–24, AUC0–∞, and Cmax. For omeprazole, analysis of AUC0–24 was planned but drug levels were below the limit of quantitation in all subjects by 8–12 h. Therefore, AUC 0–8 h (AUC0–8) was calculated instead of AUC0–24.
Bioequivalence criteria for log-transformed parameters were defined as 80–125 %. No clinically significant differences were concluded when 90 % confidence intervals (CIs) for exposure ratios fell within these bioequivalence criteria.
Results
Subject demographics and disposition
In total, 213 subjects were randomized across the five studies, of whom 210 received study medication and were included in the safety population. Overall, 200 subjects received treatment in at least two of the three dosing schedules and were eligible for PK analysis (n = 36 for losartan, n = 41 for furosemide, n = 39 for omeprazole, n = 42 for digoxin, and n = 42 for warfarin).
In total, 193 subjects completed the studies and 17 withdrew. Of the subjects who withdrew before randomization, nine did so by their own decision, six were found to have taken drugs/alcohol; following randomization, one subject was withdrawn as a result of an adverse event (rhabdomyolysis), and a second subject was withdrawn as the result of an administrative decision.
Patient demographics at baseline were similar between the treatment groups (Table 2).
Pharmacokinetic results
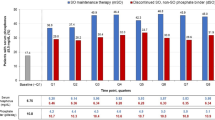
AUC0–24 and AUC0–∞
The systemic exposure of all test medications was unaffected to a clinically significant extent by the presence of sucroferric oxyhydroxide (i.e., 90 % CIs were within the bioequivalence range), based on AUC0–∞ (Table 3). Moreover, the systemic exposure of medications was unaffected irrespective of whether sucroferric oxyhydroxide was administered with the medication or 2 h earlier.
The systemic exposure, based on AUC0–24, for all drugs except omeprazole (for which AUC0–8 was measured) was also largely unaffected by the presence of sucroferric oxyhydroxide, irrespective of whether sucroferric oxyhydroxide was administered with the medication or 2 h earlier.
The AUC0–8 value of omeprazole was increased when sucroferric oxyhydroxide was administered 2 h before the medication, as the upper bound 90 % CI was outside the bioequivalence range, relative to that obtained in the absence of sucroferric oxyhydroxide.
The extent of formation of the active metabolite of losartan, EXP 3174, was also unaffected by sucroferric oxyhydroxide, with AUC parameters being within the bioequivalence range.
Cmax
Sucroferric oxyhydroxide had no clinically significant effect on the Cmax of R-warfarin, S-warfarin or EXP 3174 (i.e., 90 % CIs were within the bioequivalence range) (Table 3). However, the Cmax values of losartan, furosemide and omeprazole were decreased (lower bound 90 % CIs were outside the bioequivalence range) relative to those in the absence of sucroferric oxyhydroxide.
Furthermore, when sucroferric oxyhydroxide (and food) was administered 2 h before each of the medications, the Cmax values of losartan, furosemide, omeprazole and digoxin were increased (upper bound 90 % CIs were outside the bioequivalence range) relative to those in the absence of sucroferric oxyhydroxide.
Tmax and t1/2
The Tmax value of losartan was significantly reduced when sucroferric oxyhydroxide was administered with the medication relative to the value obtained in the absence of sucroferric oxyhydroxide (Table 4). The Tmax values of losartan, EXP 3174, furosemide, omeprazole, digoxin and R- and S-warfarin were also significantly reduced when sucroferric oxyhydroxide (and food) was administered 2 h before the medications.
A significant decrease in the t1/2 of losartan and EXP 3174 and an increase in t1/2 of furosemide were observed when sucroferric oxyhydroxide (and food) was administered with the medications, as compared to when medications were administered ìn the absence of sucroferric oxyhydroxide (Table 4).
Safety
Across the five studies, 126/210 (60.0 %) subjects experienced treatment-emergent adverse events (TEAEs). Overall, 82/210 (39.1 %) subjects reported treatment-related TEAEs. These were reported by an average of 22.9 % (n = 47/205) of subjects during ‘Schedule 1’ dosing, 5.0 % (n = 10/199) during ‘Schedule 2’ dosing, and 22.0 % (n = 44/200) during ‘Schedule 3’ dosing. GI events were the most common class of treatment-related TEAE, occurring in an average of 30.0 % (n = 63/210) of subjects across studies. Of these, discolored feces were the most frequently reported treatment-related GI event and occurred in an average of 20.0 % of subjects across the studies.
One subject in the warfarin study developed a TEAE (rhabdomyolysis) that was considered to be both serious and severe, but unrelated to study treatment. The subject reported an unplanned period of strenuous physical activity a few days prior to complaining of muscle soreness that was associated with elevated muscle enzymes. The event resolved spontaneously within a few days. There were no deaths across the studies.
Discussion
The data reported here indicate that sucroferric oxyhydroxide does not affect systemic exposure (based on AUC0–∞) to any of the drugs tested in this study when they are administered with sucroferric oxyhydroxide or 2 h after sucroferric oxyhydroxide. Similarly, sucroferric oxyhydroxide does not affect systemic exposure (based on AUC0–24) for any of the drugs, irrespective of whether sucroferric oxyhydroxide was administered with the medication or 2 h earlier. However, no AUC0–24 values could be obtained for omeprazole because drug levels were below the limit of quantification in all subjects by 8–12 h but AUC0–∞ values were within the bioequivalence criteria. Taken together, the results indicate that sucroferric oxyhydroxide may be administered concomitantly with losartan, furosemide, omeprazole, digoxin or warfarin without the need to adjust drug dosages or administration regimen.
The study data also suggest that the Cmax values of losartan, furosemide, omeprazole and digoxin are sensitive to the timing of sucroferric oxyhydroxide administration. When losartan, furosemide, omeprazole and digoxin were administered 2 h after sucroferric oxyhydroxide (and food), but ≥1 h before the next meal, their Cmax values were increased relative to those observed when the medications were given with food in the absence of sucroferric oxyhydroxide. It is possible that these differences are caused by a ‘food effect’. Cmax values for furosemide, omeprazole and digoxin have been observed to decrease when these agents are administered with food [14–16]. However, a direct effect of sucroferric oxyhydroxide on the rate of absorption of these compounds cannot be excluded because sucroferric oxyhydroxide was associated with decreased Cmax values for losartan (although the Cmax of its active metabolite EXP 3174 was unaffected), furosemide and omeprazole when given with the drugs relative to Cmax values in the absence of sucroferric oxyhydroxide—food being given with the agents in both cases. A similar action may underlie the observed effects of sucroferric oxyhydroxide on the Tmax and t1/2 of some agents investigated in these studies. However, given that the overall exposure for these agents was largely unaffected by sucroferric oxyhydroxide, as discussed above, these changes are unlikely to be clinically significant.
Sucroferric oxyhydroxide was generally well tolerated when administered with the medications in healthy subjects. The TEAEs related to treatment were almost entirely non-severe and consistent with the known safety profile of sucroferric oxyhydroxide [7, 9, 10]. Discolored feces were a common GI-related event among subjects after receiving sucroferric oxyhydroxide. Discolored feces are a known effect of sucroferric oxyhydroxide as well as other iron-based phosphate binders [9, 17] and iron-based products in general.
In previous clinical studies, sucroferric oxyhydroxide was effective at reducing serum phosphorus concentrations in CKD patients undergoing dialysis, and showed similar efficacy and tolerability to sevelamer [9, 10], while having a lower tablet burden [10]. Therefore, sucroferric oxyhydroxide may represent a new treatment option for CKD dialysis patients, with the potential for improved adherence and low risk of DDIs with the medications investigated in these studies.
References
Hruska KA, Mathew S (2011) The roles of the skeleton and phosphorus in the CKD mineral bone disorder. Adv Chronic Kidney Dis 18:98–104
Block GA (2001) Control of serum phosphorus: implications for coronary artery calcification and calcific uremic arteriolopathy (calciphylaxis). Curr Opin Nephrol Hypertens 10:741–747
Block GA, Klassen PS, Lazarus JM, Ofsthun N, Lowrie EG, Chertow GM (2004) Mineral metabolism, mortality, and morbidity in maintenance hemodialysis. J Am Soc Nephrol 15:2208–2218
Palmer SC, Hayen A, Macaskill P et al (2011) Serum levels of phosphorus, parathyroid hormone, and calcium and risks of death and cardiovascular disease in individuals with chronic kidney disease: a systematic review and meta-analysis. JAMA 305:1119–1127
Kanbay M, Goldsmith D, Akcay A, Covic A (2009) Phosphate—the silent stealthy cardiorenal culprit in all stages of chronic kidney disease: a systematic review. Blood Purif 27:220–230
Tentori F, Blayney MJ, Albert JM et al (2008) Mortality risk for dialysis patients with different levels of serum calcium, phosphorus, and PTH: the Dialysis Outcomes and Practice Patterns Study (DOPPS). Am J Kidney Dis 52:519–530
Geisser P, Philipp E (2010) PA21: a novel phosphate binder for the treatment of hyperphosphatemia in chronic kidney disease. Clin Nephrol 74:4–11
Hergesell O, Ritz E (1999) Stabilized polynuclear iron hydroxide is an efficient oral phosphate binder in uraemic patients. Nephrol Dial Transplant 14:863–867
Wüthrich RP, Chonchol M, Covic A, Gaillard S, Chong E, Tumlin JA (2013) Randomized clinical trial of the iron-based phosphate binder PA21 in hemodialysis patients. Clin J Am Soc Nephrol 8:280–289
Floege J, Ketteler M, Rastogi A et al (2012) Efficacy and safety of PA21 in hyperphosphatemic CKD patients on dialysis. J Am Soc Nephrol 23:abstract SA-PO1103
Sprague S, Floege J, Covic A et al (2013) Efficacy of PA21, a novel iron-based phosphate binder, maintained to 52 weeks in dialysis patients with hyperphosphatemia. J Am Soc Nephrol 24:abstract TH-OR027
Rifkin DE, Winkelmayer WC (2010) Medication issues in older individuals with CKD. Adv Chronic Kidney Dis 17:320–328
Mason NA, Bakus JL (2010) Strategies for reducing polypharmacy and other medication-related problems in chronic kidney disease. Semin Dial 23:55–61
Johnson BF, O’Grady J, Sabey GA, Bye C (1978) Effect of a standard breakfast on digoxin absorption in normal subjects. Clin Pharmacol Ther 23:315–319
Vaz-da-Silva M, Loureiro AI, Nunes T et al (2005) Bioavailability and bioequivalence of two enteric-coated formulations of omeprazole in fasting and fed conditions. Clin Drug Investig 25:391–399
Beermann B, Midskov C (1986) Reduced bioavailability and effect of furosemide given with food. Eur J Clin Pharmacol 29:725–727
Sinsakul M, Sika M, Koury M et al (2012) The safety and tolerability of ferric citrate as a phosphate binder in dialysis patients. Nephron Clin Pract 121:c25–c29
Acknowledgments
This manuscript was prepared with the editorial assistance of AXON Communications, Richmond, UK. This manuscript and the five Phase I pharmacokinetic studies mentioned therein were sponsored by Vifor (International) AG, St Gallen, Switzerland.
Conflict of interest
EC and VK are employees of Vifor. EC was Clinical Development Lead of the studies reported in the manuscript. VK was Sponsor Contact and author of the clinical study reports for the studies reported in the manuscript. SW was Coordinating Investigator for the warfarin study. PW was Coordinating Investigator for the losartan, furosemide, omeprazole and digoxin studies.
Ethical standard
Study documentation was approved by an Institutional Review Board/Independent Ethics Committee. The study was performed in accordance with the Declaration of Helsinki and subsequent amendments. Informed consent was obtained from all participants.
Author information
Authors and Affiliations
Corresponding author
Additional information
Clinical trial registration numbers: NCT01477411, NCT01324752, NCT01438359, NCT01452906, NCT01477424.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution License which permits any use, distribution, and reproduction in any medium, provided the original author(s) and the source are credited.
About this article
Cite this article
Chong, E., Kalia, V., Willsie, S. et al. Drug–drug interactions between sucroferric oxyhydroxide and losartan, furosemide, omeprazole, digoxin and warfarin in healthy subjects. J Nephrol 27, 659–666 (2014). https://doi.org/10.1007/s40620-014-0080-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40620-014-0080-1