Abstract
Objective
Previous studies on residential green space were inconsistent with blood lipid levels and hyperlipidemia. Thus, our study aims to explore the relationship between urban residential greenness and the blood lipid level and hyperlipidemia of the Chinese elderly population.
Methods
A total of 59,865 older adults were collected from the Shenzhen healthy aging Research (SHARE). Blood lipid levels [total cholesterol (TC), triglycerides (TG), low-density lipoprotein cholesterol (LDL-C), and high-density lipoprotein cholesterol (HDL-C)] were measured. Participants’ exposure to residential greenness was measured by the satellite-based normalized difference vegetation index (NDVI). Generalized linear mixed models (GLMMs) and logistic regression were performed to assess the associations of residential greenness with lipid levels and dyslipidemia (high TG, high TC, low HDL-C, and high LDL-C).
Results
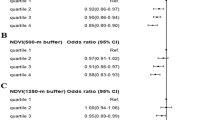
Each per 1 standard deviation (SD) increase in NDVI250-m was associated with a higher HDL-C level (β = 0.003, 95% (confidence interval, CI):0.001–0.005) and lower TG level (β = − 0.005, 95% CI − 0.141–0.121), after fully adjusting for covariates. Each increment in per interquartile range (IQR)-unit increase in NDVI250-m was associated with lower odds of high TG (odds ratio, OR 0.94, 95% CI 0.91–0.97) and low HDL-C (OR 0.96, 95% CI 0.94–0.99). The NDVI250-m has the highest protective effect on the incidence of high TG and low HDL-C, followed by NDVI500-m and NDVI1250-m. Stratified analyses showed that association between residential greenness and hyperlipidemia was modified by sex, age, BMI, household registration, and physical activity.
Conclusion
Higher greenness exposure was beneficially associated with lipid levels and dyslipidemia among Chinese city-dwelling older adults.




Similar content being viewed by others
Data availability
Not applicable
Code availability
Not applicable
References
Alloubani A, Nimer R, Samara R (2021) Relationship between Hyperlipidemia, cardiovascular disease and stroke: a systematic review. Curr Cardiol Rev 17(6):e051121189015. https://doi.org/10.2174/1573403x16999201210200342
Opoku S, Gan Y, Fu W et al (2019) Prevalence and risk factors for dyslipidemia among adults in rural and urban China: findings from the China National Stroke Screening and prevention project (CNSSPP). BMC Public Health 19(1):1500. https://doi.org/10.1186/s12889-019-7827-5
Pan L, Yang Z, Wu Y et al (2016) The prevalence, awareness, treatment and control of dyslipidemia among adults in China. Atherosclerosis 248:2–9. https://doi.org/10.1016/j.atherosclerosis.2016.02.006
Li Y, Zhao L, Yu D, Ding G (2018) The prevalence and risk factors of dyslipidemia in different diabetic progression stages among middle-aged and elderly populations in China. PLoS ONE 13(10):e0205709. https://doi.org/10.1371/journal.pone.0205709
Berberich AJ, Hegele RA (2019) The role of genetic testing in dyslipidaemia. Pathology 51(2):184–192. https://doi.org/10.1016/j.pathol.2018.10.014
Aslam F, Haque A, Lee LV, Foody J (2009) Hyperlipidemia in older adults. Clin Geriatr Med 25(4):591–606. https://doi.org/10.1016/j.cger.2009.08.001
Mannu GS, Zaman MJ, Gupta A, Rehman HU, Myint PK (2013) Evidence of lifestyle modification in the management of hypercholesterolemia. Curr Cardiol Rev 9(1):2–14. https://doi.org/10.2174/157340313805076313
Ruixing Y, Jinzhen W, Yaoheng H, Jing T, Hai W, Muyan L et al (2008) Associations of diet and lifestyle with hyperlipidemia for middle-aged and elderly persons among the Guangxi Bai Ku Yao and Han populations. J Am Diet Assoc 108(6):970–976. https://doi.org/10.1016/j.jada.2008.03.010
Markevych I, Standl M, Sugiri D, Harris C, Maier W, Berdel D et al (2016) Residential greenness and blood lipids in children: a longitudinal analysis in GINIplus and LISAplus. Environ Res 151:168–173. https://doi.org/10.1016/j.envres.2016.07.037
Rammah A, Whitworth KW, Amos CI, Estarlich M, Guxens M, Ibarluzea J et al (2021) Air Pollution, Residential greenness and metabolic dysfunction during early pregnancy in the INfancia y Medio Ambiente (INMA) cohort. Int J Environ Res Public Health 18(17):9354. https://doi.org/10.3390/ijerph18179354
Brown SC, Lombard J, Wang K, Byrne MM, Toro M, Plater-Zyberk E et al (2016) Neighborhood greenness and chronic health conditions in medicare beneficiaries. Am J Prev Med 51(1):78–89. https://doi.org/10.1016/j.amepre.2016.02.008
Kim HJ, Min JY, Kim HJ, Min KB (2016) Parks and green areas are associated with decreased risk for hyperlipidemia. Int J Environ Res Public Health 13(12):1205. https://doi.org/10.3390/ijerph13121205
Paquet C, Coffee NT, Haren MT, Howard NJ, Adams RJ, Taylor AW et al (2014) Food environment, walkability, and public open spaces are associated with incident development of cardio-metabolic risk factors in a biomedical cohort. Health Place 28:173–176. https://doi.org/10.1016/j.healthplace.2014.05.001
Bloemsma LD, Gehring U, Klompmaker JO, Hoek G, Janssen NAH, Lebret E et al (2019) Green space, air pollution, traffic noise and cardiometabolic health in adolescents: the PIAMA birth cohort. Environ Int 131:104991. https://doi.org/10.1016/j.envint.2019.104991
Egorov AI, Griffin SM, Converse RR, Styles JN, Sams EA, Wilson A et al (2017) Vegetated land cover near residence is associated with reduced allostatic load and improved biomarkers of neuroendocrine, metabolic and immune functions. Environ Res 158:508–521. https://doi.org/10.1016/j.envres.2017.07.009
Fan S, Yang BY, Xue Z, Huang WZ, Zhou Z, Yuan J et al (2020) Associations between residential greenness and blood lipids in Chinese Uyghur adults. Environ Int 142:105903. https://doi.org/10.1016/j.envint.2020.105903
Jiang J, Mao S, Xie Y, Chen X, Abulaiti K, Liu M et al (2022) Is residential greenness associated with dyslipidemia and lipid levels in Chinese rural-dwelling adults? The Henan rural cohort study. Environ Sci Pollut Res Int 29(4):5852–5862. https://doi.org/10.1007/s11356-021-16026-3
Yang BY, Markevych I, Heinrich J, Bloom MS, Qian Z, Geiger SD et al (2019) Residential greenness and blood lipids in urban-dwelling adults: the 33 communities Chinese health study. Environ Pollut 250:14–22. https://doi.org/10.1016/j.envpol.2019.03.128
Zhou Y, Huang B, Wang J, Chen B, Kong H, Norford L (2019) Climate-conscious urban growth mitigates urban warming: evidence from Shenzhen. China Environ Sci Technol 53(20):11960–11968. https://doi.org/10.1021/acs.est.9b01645
Ni W, Yuan X, Zhang J, Li P, Zhang HM, Zhang Y et al (2021) Factors associated with treatment and control of hypertension among elderly adults in Shenzhen, China: a large-scale cross-sectional study. BMJ Open 11(8):e044892. https://doi.org/10.1136/bmjopen-2020-044892
Zhu Junren, Gao Runlin, Zhao Shuijing et al (2016) Guidelines for the Prevention and Treatment of Dyslipidemia in Chinese Adults (Revised 2016). Chin J Circ
Thiering E, Markevych I, Brüske I, Fuertes E, Kratzsch J, Sugiri D et al (2016) Associations of residential long-term air pollution exposures and satellite-derived greenness with insulin resistance in german adolescents. Environ Health Perspect 124(8):1291–1298. https://doi.org/10.1289/ehp.1509967
Chen H, Burnett RT, Bai L, Kwong JC, Crouse DL, Lavigne E et al (2020) Residential greenness and cardiovascular disease incidence, readmission, and mortality. Environ Health Perspect 128(8):87005. https://doi.org/10.1289/ehp6161
Ji JS, Zhu A, Bai C, Wu CD, Yan L, Tang S et al (2019) Residential greenness and mortality in oldest-old women and men in China: a longitudinal cohort study. Lancet Planet Health 3(1):e17–e25. https://doi.org/10.1016/s2542-5196(18)30264-x
Ji JS, Zhu A, Lv Y, Shi X (2020) Interaction between residential greenness and air pollution mortality: analysis of the Chinese longitudinal healthy longevity survey. Lancet Planet Health 4(3):e107–e115. https://doi.org/10.1016/s2542-5196(20)30027-9
Yang Y, Diez-Roux AV (2012) Walking distance by trip purpose and population subgroups. Am J Prev Med 43(1):11–19. https://doi.org/10.1016/j.amepre.2012.03.015
James P, Hart JE, Banay RF, Laden F (2016) Exposure to greenness and mortality in a nationwide prospective cohort study of women. Environ Health Perspect 124(9):1344–1352. https://doi.org/10.1289/ehp.1510363
Zhu A, Zeng Y, Ji JS (2020) Residential greenness alters serum 25(oh)d concentrations: a longitudinal cohort of chinese older adults. J Am Med Dir Assoc 21(12):1968–72.e2. https://doi.org/10.1016/j.jamda.2020.04.026
Zhou BF (2002) Predictive values of body mass index and waist circumference for risk factors of certain related diseases in Chinese adults–study on optimal cut-off points of body mass index and waist circumference in Chinese adults. Biomed Environ Sci 15(1):83–96
Guo J, Wu J, Wei D, Wang T, Hu Y, Lin Y et al (2022) Association between greenness and dyslipidemia in patients with coronary heart disease: a proteomic approach. Ecotoxicol Environ Saf 231:113199. https://doi.org/10.1016/j.ecoenv.2022.113199
Liu T, Cai B, Peng W, Xiao L, Shi H, Wu X et al (2021) Association of neighborhood greenness exposure with cardiovascular diseases and biomarkers. Int J Hyg Environ Health 234:113738. https://doi.org/10.1016/j.ijheh.2021.113738
Yeager R, Riggs DW, DeJarnett N, Tollerud DJ, Wilson J, Conklin DJ et al (2018) Association between residential greenness and cardiovascular disease risk. JAHA 7(24):e009117. https://doi.org/10.1161/jaha.118.009117
Hirabayashi S, Nowak DJ (2016) Comprehensive national database of tree effects on air quality and human health in the United States. Environ Pollut 215:48–57. https://doi.org/10.1016/j.envpol.2016.04.068
Geneshka M, Coventry P, Cruz J, Gilbody S (2021) Relationship between green and blue spaces with mental and physical health: a systematic review of longitudinal observational studies. Int J Environ Res Public Health 18(17):9010. https://doi.org/10.3390/ijerph18179010
Mu X, Yu K, Long P, Niu R, Li W, Chen H et al (2021) Leisure-time physical activity and risk of incident cardiovascular disease in Chinese retired adults. Sci Rep 11(1):24202. https://doi.org/10.1038/s41598-021-03475-6
Cohen-Cline H, Turkheimer E, Duncan GE (2015) Access to green space, physical activity and mental health: a twin study. J Epidemiol Community Health 69(6):523–529. https://doi.org/10.1136/jech-2014-204667
Jiang Y, Huang J, Shi T, Wang H (2021) Interaction of Urban rivers and green space morphology to mitigate the urban heat island effect: case-based comparative analysis. Int J Environ Res Public Health 18(21):11404. https://doi.org/10.3390/ijerph182111404
Gonzales-Inca C, Pentti J, Stenholm S, Suominen S, Vahtera J, Käyhkö N (2022) Residential greenness and risks of depression: longitudinal associations with different greenness indicators and spatial scales in a finnish population cohort. Health Place 74:102760. https://doi.org/10.1016/j.healthplace.2022.102760
Bai X, Li Z, Chen J, Liu C, Wu X (2020) Socioeconomic inequalities in mental distress and life satisfaction among older Chinese men and women: the role of family functioning. HEALTH SOC CARE COMM 28(4):1270–1281. https://doi.org/10.1111/hsc.12960
Liu H, Wu B, Feng Z (2020) Social participation and self-perception of being old in China. INT J AGING HUM DEV 91(3):219–234. https://doi.org/10.1177/0091415019875456
Acknowledgements
We thank all individuals who participated in the physical examination. We also thank all the medical staff in the community health service centers in Shenzhen.
Funding
Z.G.Z was supported by Shenzhen medical key discipline construction fund and Sanming Project of Medicine in Shenzhen (Grant No. SZSM201811093). J.X. was supported by the Science and Technology Planning Project of Shenzhen City, Guangdong Province, China (Grant No. KCXFZ20201221173600001). W.Q.N. was supported by the Medical Scientific Research Foundation of Guangdong Province, China (grant number A2022082). The funders had no role in study design, data collection, writing, or the decision to submit this manuscript.
Author information
Authors and Affiliations
Contributions
Z.G.Z. designed the study. W.Q.N. contributed data. H.M. Z. drafted the analysis plan. J.X. performed the statistical analysis and wrote the manuscript. Y.Y.S., P.K, and M.Z.X., contributed to the statistical analysis. WQN, XLY and YZ interpreted the data and made many substantial contributions to the data analysis, such as data analysis and interpretation in Tables 1, 2 and 3. Z.G.Z is the guarantors of this work and, as such, had full access to all the data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis. All authors reviewed and edited the manuscript and approved of its submission.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no competing interests and funding in our study.
Ethics approval
The study was approved by the Shenzhen Center for Chronic Disease Control Human Ethics Committee (No. SZCCC-2021-061-01-PJ).
Consent to participate
As claims data were provided anonymously, informed consent was exempted by the Shenzhen Center for Chronic Disease Control Human Ethics Committee.
Consent for publication
All authors declare that they agree to the manuscript publish to Journal of Endocrine Investigation.
Sponsor’s role
Not applicable
Human and animal rights
All procedures performed in studies invovling human participants were in accordance with the ethical standards of the institutional and the study was approved by the Shenzhen Center for Chronic Disease Control Human Ethics Committee (No. SZCCC-2021-061-01-PJ), and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Author statements
The material presented in our manuscript is original and has not been submitted for publication else where.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Xu, J., Yuan, X., Ni, W. et al. Associations between residential greenness and blood lipids in Chinese elderly population. J Endocrinol Invest 45, 2329–2339 (2022). https://doi.org/10.1007/s40618-022-01870-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40618-022-01870-y