Abstract
Purpose
The purpose of this study was to estimate how many individuals with severe obesity and NAFLD should be referred to hepatologists according to the EASL–EASD–EASO guidelines and whether the choice of specific indicators of liver fibrosis would significantly impact the number of referrals.
Methods
This was a single-center retrospective study of 495 individuals with severe obesity screened at our institution between 2012 and 2018 for a bariatric surgery intervention. The guidelines were applied using the NAFLD Liver Fat Score (NLFS) to assess the presence of steatosis and the NAFLD fibrosis score (NFS), Fibrosis-4 (FIB-4) and Hepamet Fibrosis Score (HFS) to assess the risk of advanced fibrosis.
Results
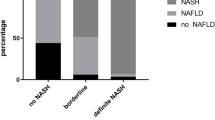
Three hundred and seventy-nine patients (76.6%) had evidence of liver steatosis. The application of the guidelines would lead to referral of 66.3% of patients using NFS, 31.7% using FIB-4 and 34.2% using HFS. When referrals due to abnormal liver function tests were excluded, these percentages dropped to 55.8%, 7.3% and 12.1%, respectively. The strongest inter-biomarker agreement was found between FIB-4 and HFS (κ = 0.86, 95% CI 0.815–0.910).
Conclusion
Strict application of the guidelines in individuals with severe obesity would probably lead to over-referral, although a great variability exists among the different scores.


Similar content being viewed by others
Data availability
The datasets are available from the corresponding author on reasonable request.
Abbreviations
- AASLD:
-
American Association for the Study of Liver Diseases
- EASD:
-
European Association for the Study of Diabetes
- EASL:
-
European Association for the Study of the Liver
- EASO:
-
European Association for the Study of Obesity
- GGT:
-
γ-Glutamyltransferase
- FIB-4:
-
Fibrosis-4
- FLI:
-
Fatty Liver Index
- HFS:
-
Hepamet Fibrosis Score
- NAFLD:
-
Non-alcoholic fatty liver disease
- NASH:
-
Non-alcoholic steatohepatitis
- NFS:
-
NAFLD fibrosis score
References
Pimpin L, Cortez-Pinto H, Negro F, Corbould E, Lazarus JV, Webber L, Sheron N (2018) Burden of liver disease in Europe: epidemiology and analysis of risk factors to identify prevention policies. J Hepatol 69(3):718–735. https://doi.org/10.1016/j.jhep.2018.05.011
Younossi ZM, Koenig AB, Abdelatif D, Fazel Y, Henry L, Wymer M (2016) Global epidemiology of nonalcoholic fatty liver disease-meta-analytic assessment of prevalence, incidence, and outcomes. Hepatology 64(1):73–84. https://doi.org/10.1002/hep.28431
Younossi ZM, Golabi P, de Avila L, Paik J, Srishord M, Fukui N, Qiu Y, Burns L, Afendy A, Nader F (2019) The Global Epidemiology of NAFLD and NASH in Patients with type 2 diabetes: a systematic review and meta-analysis. J Hepatol. https://doi.org/10.1016/j.jhep.2019.06.021
Machado M, Marques-Vidal P, Cortez-Pinto H (2006) Hepatic histology in obese patients undergoing bariatric surgery. J Hepatol 45(4):600–606. https://doi.org/10.1016/j.jhep.2006.06.013
Ekstedt M, Hagstrom H, Nasr P, Fredrikson M, Stal P, Kechagias S, Hultcrantz R (2015) Fibrosis stage is the strongest predictor for disease-specific mortality in NAFLD after up to 33 years of follow-up. Hepatology 61(5):1547–1554. https://doi.org/10.1002/hep.27368
Adams LA, Lymp JF, Sauver J, Sanderson SO, Lindor KD, Feldstein A, Angulo P (2005) The natural history of nonalcoholic fatty liver disease: a population-based cohort study. Gastroenterology 129(1):113–121
Chalasani N, Younossi Z, Lavine JE, Charlton M, Cusi K, Rinella M, Harrison SA, Brunt EM, Sanyal AJ (2018) The diagnosis and management of nonalcoholic fatty liver disease: practice guidance from the American Association for the Study of Liver Diseases. Hepatology 67(1):328–357. https://doi.org/10.1002/hep.29367
European Association for the Study of the L, European Association for the Study of D, European Association for the Study of O (2016) EASL–EASD–EASO Clinical Practice Guidelines for the management of non-alcoholic fatty liver disease. J Hepatol 64(6):1388–1402. https://doi.org/10.1016/j.jhep.2015.11.004
Blond E, Disse E, Cuerq C, Drai J, Valette PJ, Laville M, Thivolet C, Simon C, Caussy C (2017) EASL–EASD–EASO clinical practice guidelines for the management of non-alcoholic fatty liver disease in severely obese people: do they lead to over-referral? Diabetologia 60(7):1218–1222. https://doi.org/10.1007/s00125-017-4264-9
Levey AS, Stevens LA, Schmid CH, Zhang YL, Castro AF 3rd, Feldman HI, Kusek JW, Eggers P, Van Lente F, Greene T, Coresh J (2009) A new equation to estimate glomerular filtration rate. Ann Intern Med 150(9):604–612. https://doi.org/10.7326/0003-4819-150-9-200905050-00006
Alberti KG, Eckel RH, Grundy SM, Zimmet PZ, Cleeman JI, Donato KA, Fruchart JC, James WP, Loria CM, Smith SC Jr (2009) Harmonizing the metabolic syndrome: a joint interim statement of the International Diabetes Federation Task Force on Epidemiology and Prevention; National Heart, Lung, and Blood Institute; American Heart Association; World Heart Federation; International Atherosclerosis Society; and International Association for the Study of Obesity. Circulation 120(16):1640–1645. https://doi.org/10.1161/circulationaha.109.192644
Classification and Diagnosis of Diabetes (2018) Standards of medical care in diabetes-2018. Diabetes Care 41(1):S13–S27. https://doi.org/10.2337/dc18-S002
Mottin CC, Moretto M, Padoin AV, Swarowsky AM, Toneto MG, Glock L, Repetto G (2004) The role of ultrasound in the diagnosis of hepatic steatosis in morbidly obese patients. Obes Surg 14(5):635–637. https://doi.org/10.1381/096089204323093408
Bedogni G, Bellentani S, Miglioli L, Masutti F, Passalacqua M, Castiglione A, Tiribelli C (2006) The Fatty Liver Index: a simple and accurate predictor of hepatic steatosis in the general population. BMC Gastroenterol 6:33. https://doi.org/10.1186/1471-230X-6-33
Kotronen A, Peltonen M, Hakkarainen A, Sevastianova K, Bergholm R, Johansson LM, Lundbom N, Rissanen A, Ridderstråle M, Groop L, Orho-Melander M, Yki-Järvinen H (2009) Prediction of non-alcoholic fatty liver disease and liver fat using metabolic and genetic factors. Gastroenterology 137(3):865–872. https://doi.org/10.1053/j.gastro.2009.06.005
Sterling RK, Lissen E, Clumeck N, Sola R, Correa MC, Montaner J, Sulkowski S, Torriani FJ, Dieterich DT, Thomas DL, Messinger D, Nelson M, Investigators AC (2006) Development of a simple noninvasive index to predict significant fibrosis in patients with HIV/HCV coinfection. Hepatology 43(6):1317–1325. https://doi.org/10.1002/hep.21178
Angulo P, Hui JM, Marchesini G, Bugianesi E, George J, Farrell GC, Enders F, Saksena S, Burt AD, Bida JP, Lindor K, Sanderson SO, Lenzi M, Adams LA, Kench J, Therneau TM, Day CP (2007) The NAFLD fibrosis score: a noninvasive system that identifies liver fibrosis in patients with NAFLD. Hepatology 45(4):846–854. https://doi.org/10.1002/hep.21496
Ampuero J, Pais R, Aller R, Gallego-Durán R, Crespo J, García-Monzón C, Boursier J, Vilar E, Petta S, Ming-Hua Z, Escudero D, Calleja JL, Aspichueta P, Diago M, Rosales JM, Caballería J, Camarero J, Iacono O, Benlloch S, Albillos A, Turnes J, Banales JM, Ratziu V, Romero-Gómez M (2019) Development and validation of hepamet fibrosis scoring system a simple, noninvasive test to identify patients with nonalcoholic fatty liver disease with advanced fibrosis. Clin Gastroenterol Hepatol. https://doi.org/10.1016/j.cgh.2019.05.051
D'Agostino RB (1971) An omnibus test of normality for moderate and large size samples. Biometrika 58(2):341–348. https://doi.org/10.2307/2334522
Altman DG (1990) Practical statistics for medical research. CRC Press, New York
Landis JR, Koch GG (1977) The measurement of observer agreement for categorical data. Biometrics 33(1):159–174. https://doi.org/10.2307/2529310
Bedossa P, Tordjman J, Wisnewsky J, Poitou C, Oppert J-M, Torcivia A, Bouillot J-L, Paradis V, Ratziu V, Clément K (2017) Systematic review of bariatric surgery liver biopsies clarifies the natural history of liver disease in patients with severe obesity. Gut 66(9):1688–1696. https://doi.org/10.1136/gutjnl-2016-312238
Ong JP, Elariny H, Collantes R, Younoszai A, Chandhoke V, Reines HD, Goodman Z, Younossi ZM (2005) Predictors of nonalcoholic steatohepatitis and advanced fibrosis in morbidly obese patients. Obes Surg 15(3):310–315. https://doi.org/10.1381/0960892053576820
Morita S, Dde S, Morita FH, Morita NK, Lobo SM (2015) Prevalence of non-alcoholic fatty liver disease and steatohepatitis risk factors in patients undergoing bariatric surgery. Obes Surg 25(12):2335–2343. https://doi.org/10.1007/s11695-015-1696-5
Ooi GJ, Burton PR, Doyle L, Wentworth JM, Bhathal PS, Sikaris K, Cowley MA, Roberts SK, Kemp W, O'Brien PE, Brown WA (2017) Modified thresholds for fibrosis risk scores in nonalcoholic fatty liver disease are necessary in the obese. Obes Surg 27(1):115–125. https://doi.org/10.1007/s11695-016-2246-5
Praveen Raj P, Gomes RM, Kumar S, Senthilnathan P, Karthikeyan P, Shankar A, Palanivelu C (2015) The effect of surgically induced weight loss on nonalcoholic fatty liver disease in morbidly obese Indians: "NASHOST" prospective observational trial. Surg Obes Relat Dis 11(6):1315–1322. https://doi.org/10.1016/j.soard.2015.02.006
Xiao G, Zhu S, Xiao X, Yan L, Yang J, Wu G (2017) Comparison of laboratory tests, ultrasound, or magnetic resonance elastography to detect fibrosis in patients with nonalcoholic fatty liver disease: a meta-analysis. Hepatology 66(5):1486–1501. https://doi.org/10.1002/hep.29302
Qureshi K, Clements RH, Abrams GA (2008) The utility of the "NAFLD fibrosis score" in morbidly obese subjects with NAFLD. Obes Surg 18(3):264–270. https://doi.org/10.1007/s11695-007-9295-8
Li L, Liu D-W, Yan H-Y, Wang Z-Y, Zhao S-H, Wang B (2016) Obesity is an independent risk factor for non-alcoholic fatty liver disease: evidence from a meta-analysis of 21 cohort studies. Obes Rev 17(6):510–519. https://doi.org/10.1111/obr.12407
Jang ES, Jeong S-H, Hwang SH, Kim HY, Ahn SY, Lee J, Lee SH, Park YS, Hwang JH, Kim J-W, Kim N, Lee DH (2012) Effects of coffee, smoking, and alcohol on liver function tests: a comprehensive cross-sectional study. BMC Gastroenterol 12(1):145. https://doi.org/10.1186/1471-230X-12-145
Acknowledgements
We thank the staff of the department of Metabolic Medicine, Bariatric Surgery and Biology, Policlinico di Monza, for their helpful assistance.
Funding
The authors received no specific funding for this work.
Author information
Authors and Affiliations
Contributions
All authors made substantial contributions to the conception and design or acquisition, analysis and interpretation of data. All authors drafted the article or revised it critically for important intellectual content. All authors approved the final version of the manuscript to be published. GP is the guarantor of this work.
Corresponding author
Ethics declarations
Conflict of interest
All authors declare no conflict of interest related to this study.
Research involving human participants and/or animals
All procedures followed were in accordance with the ethical standards of the responsible committee on human experimantation (Institutional and National) and with the Helsinki Declaration of 1964 and later versions.
Informed consent
Informed consent was obtained from all patients for being included in the study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Ciardullo, S., Ronchetti, C., Muraca, E. et al. Impact of using different biomarkers of liver fibrosis on hepatologic referral of individuals with severe obesity and NAFLD. J Endocrinol Invest 43, 1019–1026 (2020). https://doi.org/10.1007/s40618-020-01188-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40618-020-01188-7