Abstract
Objective
The purpose of this study was to predict the poor and excessive ovarian response using anti-Müllerian hormone (AMH) levels following a long agonist protocol in IVF candidates.
Research design and methods
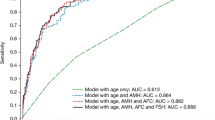
Through a prospective cohort study, the type of relationship and appropriate scale for AMH were determined using the fractional polynomial regression. To determine the effect of AMH on the outcomes of ovarian stimulation and different ovarian responses, the multi-nominal and negative binomial regression models were fitted using backward stepwise method. The ovarian response of study subject who entered a standard long-term treatment cycle with GnRH agonist was evaluated using prediction model, separately and in combined models with (ROC) curves.
Results
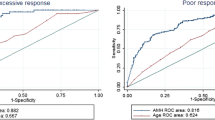
The use of standard long-term treatments with GnRH agonist led to positive pregnancy test results in 30 % of treated patients. With each unit increase in the log of AMH, the odds ratio of having poor response compared to normal response decreases by 64 % (OR 0.36, 95 % CI 0.19–0.68). Also the results of negative binomial regression model indicated that for one unit increase in the log of AMH blood levels, the odds of releasing an oocyte increased 24 % (OR 1.24, 95 % CI 1.14–1.35). The optimal cut-off points of AMH for predicting excessive and poor ovarian responses were 3.4 and 1.2 ng/ml, respectively, with area under curves of 0.69 (0.60–0.77) and 0.76 (0.66–0.86), respectively.
Conclusion
By considering the age of the patient undergoing infertility treatment as a variable affecting ovulation, use of AMH levels showed to be a good test to discriminate between different ovarian responses.


Similar content being viewed by others
References
Ubaldi F, Vaiarelli A, D’Anna R, Rienzi L (2014) Management of poor responders in IVF: is there anything new? Biomed Res Int 2014:Art ID 352098. doi:10.1155/2014/352098
Jirge PR, Chougule SM, Gavali VG, Bhomkar DA (2014) Impact of dehydroepiandrosterone on clinical outcome in poor responders: a pilot study in women undergoing in vitro fertilization, using bologna criteria. JHRS 7:175
Ravhon A, Lavery S, Michael S, Donaldson M, Margara R, Trew G et al (2000) Dynamic assays of inhibin B and oestradiol following buserelin acetate administration as predictors of ovarian response in IVF. Hum Reprod 15:2297–2301
Fauser B, Diedrich K, Devroey P (2008) Predictors of ovarian response: progress towards individualized treatment in ovulation induction and ovarian stimulation. Hum Reprod Update 14:1–14
Yassin MM, Sharif FA, Laqqan MM (2013) Anti-mullerian hormone as a predictor of ovarian reserve and ovarian response in IVF women from Gaza strip. Iran J Reprod Med 11:261
Maheshwari A, Fowler P, Bhattacharya S (2006) Assessment of ovarian reserve—should we perform tests of ovarian reserve routinely? Hum Reprod 21:2729–2735
Lass A, Skull J, McVeigh E, Margara R, Winston R (1997) Measurement of ovarian volume by transvaginal sonography before ovulation induction with human menopausal gonadotrophin for in vitro fertilization can predict poor response. Hum Reprod 12:294–297
Broekmans FJ, Faddy M, te Velde ER (2005) Ovarian reserve and reproductive age may be determined from measurement of ovarian volume by transvaginal sonography. Hum Reprod 20:1114–1115
Chang M-Y, Chiang C-H, Hsieh T, Soong Y, Hsu K (1998) Use of the antral follicle count to predict the outcome of assisted reproductive technologies. Fertil Steril 69:505–510
Hendriks DJ, Mol BWJ, Bancsi LF, Te Velde ER, Broekmans FJ (2005) Antral follicle count in the prediction of poor ovarian response and pregnancy after in vitro fertilization: a meta-analysis and comparison with basal follicle-stimulating hormone level. Fertil Steril 83:291–301
Jayaprakasan K, Campbell B, Hopkisson J, Johnson I, Raine-Fenning N (2010) A prospective, comparative analysis of anti-Müllerian hormone, inhibin-B, and three-dimensional ultrasound determinants of ovarian reserve in the prediction of poor response to controlled ovarian stimulation. Fertil Steril 93:855–864
Van Rooij I, Broekmans F, Te Velde E, Fauser B, Bancsi L, De Jong F et al (2002) Serum anti-Müllerian hormone levels: a novel measure of ovarian reserve. Hum Reprod 17:3065–3071
La Marca A, Sighinolfi G, Radi D, Argento C, Baraldi E, Artenisio AC et al (2010) Anti-Müllerian hormone (AMH) as a predictive marker in assisted reproductive technology (ART). Hum Reprod Update 16:113–130
Lin P-Y, Huang F-J, Kung F-T, Chiang H-J, Lin Y-J, Lin Y-C et al (2014) Evaluation of serum anti-mullerian hormone as a biomarker of early ovarian aging in young women undergoing IVF/ICSI cycle. Int J Clin Exp Patho 7:6245
Chang HJ, Han SH, Lee JR, Jee BC, Lee BI, Suh CS et al (2010) Impact of laparoscopic cystectomy on ovarian reserve: serial changes of serum anti-Müllerian hormone levels. Fertil Steril 94:343–349
Singh N, Malik E, Banerjee A, Chosdol K, Sreenivas V, Mittal S (2013) “Anti-Mullerian hormone: marker for ovarian response in controlled ovarian stimulation for IVF patients”: a first pilot study in the Indian population. J Obstet Gynecol India 63:268–272
Li HWR, Wong CYG, Yeung WSB, Ho PC, Ng EHY (2011) Serum anti-müllerian hormone level is not altered in women using hormonal contraceptives. Contraception 83:582–585
Royston P, Altman DG, Sauerbrei W (2006) Dichotomizing continuous predictors in multiple regression: a bad idea. Stat Med 25:127–141
Jacoby WG (2000) Loess. a nonparametric, graphical tool for depicting relationships between variables. Electoral Stud 19:577–613
Royston P, Sauerbrei W (2008) Multivariable model-building: a pragmatic approach to regression anaylsis based on fractional polynomials for modelling continuous variables. Wiley, London
Harrell FE (2001) Regression modeling strategies: with applications to linear models, logistic regression, and survival analysis. Springer, Berlin
Hilbe JM (2011) Negative binomial regression. Cambridge University Press, Cambridge
Anderson R, Nelson S, Wallace W (2012) Measuring anti-Müllerian hormone for the assessment of ovarian reserve: when and for whom is it indicated? Maturitas 71:28–33
Streuli I, Fraisse T, Pillet C, Ibecheole V, Bischof P, De Ziegler D (2008) Serum antimüllerian hormone levels remain stable throughout the menstrual cycle and after oral or vaginal administration of synthetic sex steroids. Fertil Steril 90:395–400
La Marca A, Stabile G, Artenisio AC, Volpe A (2006) Serum anti-Mullerian hormone throughout the human menstrual cycle. Hum Reprod 21:3103–3107
Hamdine O, Eijkemans M, Lentjes E, Torrance H, Macklon N, Fauser B et al (2015) Ovarian response prediction in GnRH antagonist treatment for IVF using anti-Müllerian hormone. Hum Reprod 30:170–178
Ficicioglu C, Cenksoy PO, Yildirim G, Kaspar C (2014) Which cut-off value of serum anti-Müllerian hormone level can predict poor ovarian reserve, poor ovarian response to stimulation and in vitro fertilization success? A prospective data analysis. Gynecol Endocrinol 30:372–376
Ganidou MA, Kolibianakis EM, Venetis CA, Gerou S, Makedos GA, Klearchou N et al (2014) Is assessment of anti-mullerian hormone and/or antral follicle count useful in the prediction of ovarian response in expected normal responders treated with a fixed dose of recombinant FSH and GnRH antagonists? A prospective observational study. Gynecol Endocrinol 30:817–821
Vural B, Cakiroglu Y, Vural F, Filiz S (2014) Hormonal and functional biomarkers in ovarian response. Arch Gynecol Obstet 289:1355–1361
Broekmans F, Kwee J, Hendriks D, Mol B, Lambalk C (2006) A systematic review of tests predicting ovarian reserve and IVF outcome. Hum Reprod Update 12:685–718
Tokura Y, Yoshino O, Ogura-Nose S, Motoyama H, Harada M, Osuga Y et al (2013) The significance of serum anti-Müllerian hormone (AMH) levels in patients over age 40 in first IVF treatment. J Assist Reprod Genet 30:821–825
Verhagen T, Hendriks D, Bancsi L, Mol B, Broekmans F (2008) The accuracy of multivariate models predicting ovarian reserve and pregnancy after in vitro fertilization: a meta-analysis. Hum Reprod Update 14:95–100
Cook NR (2008) Statistical evaluation of prognostic versus diagnostic models: beyond the ROC curve. Clin Chem 54:17–23
Elder K, Dale B (2010) In-vitro fertilization. Cambridge University Press, Cambridge
Acknowledgments
The author would like to thank Infertility and Reproductive Health Research Center of Shahid Beheshti University of Medical Sciences for their financial support of this study.
Conflict of interest
The authors have stated explicitly that there are no conflicts of interest in connection with this article.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
All the individuals had been informed of the purposes of the study and gave their oral informed consent.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Heidar, Z., Bakhtiyari, M., Mirzamoradi, M. et al. Prediction of different ovarian responses using anti-Müllerian hormone following a long agonist treatment protocol for IVF. J Endocrinol Invest 38, 1007–1015 (2015). https://doi.org/10.1007/s40618-015-0297-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40618-015-0297-4