Abstract
Background
Recently, an increased scientific interest was focused on mild approaches for ovarian stimulation in clinical practice. Milder stimulation aims to develop safer and more patient-friendly protocols which are more physiological, less drug use, less expensive and the risks of treatment are highly minimized.
Aim
To investigate the efficacy and safety of a mild ovarian stimulation protocol in patients at high risk of developing ovarian hyperstimulation syndrome (OHSS), compared to conventional long down-regulation protocol.
Subjects and methods
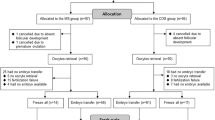
This a prospective, open, randomized study, included 349 infertile patients considered at high risk of developing OHSS, undergoing in vitro fertilization treatment in two private assisted reproduction centers. The patients were randomized into two groups: group A (n = 148) had a mild/minimal stimulation protocol of recombinant FSH (rFSH) combined with GnRH antagonist. Group B (n = 201) (control group) had a standard long protocol of rFSH combined with GnRH agonist.
Results
There was no significant difference observed between the two groups regarding the mean number of oocytes retrieved per patient, mature metaphase II oocytes, fertilization rate, and embryo cleavage rate. Significantly higher implantation rate (21.5 vs 14.5 %) (p < 0.05), pregnancy rate (37.7 vs 23.4 %) (p < 0.05), and delivery rate (32.8 vs 20.1 %) (p < 0.05) were observed in favor of groups A compared to group B. Lower proportion of patients (4.7 %), though not statistically significant, has developed OHSS in group A compared to group B (8.4 %).
Conclusion
Our study shows that mild stimulation regimen is highly effective for ovarian stimulation of patients who have experienced OHSS complication without increasing the risk of OHSS.
Similar content being viewed by others
Abbreviations
- OHSS:
-
Ovarian hyperstimulation syndrome
- rFSH:
-
Recombinant follicle-stimulating hormone
- IVF:
-
In vitro fertilization
- PCOS:
-
Polycystic ovarian syndrome
References
Templeton A, Morris JK (1998) Reducing the risk of multiple births by transfer of two embryos after in vitro fertilization. N Engl J Med 339:573–577
Macklon NS, Stouffer RL, Giudice LC, Fauser BC (2006) The science behind 25 years of ovarian stimulation for in vitro fertilization. Endocr Rev 27:170–207
Fauser BC, Devroey P (2005) Why is the clinical acceptance of gonadotropin-releasing hormone antagonist cotreatment during ovarian hyperstimulation for in vitro fertilization so slow? Fertil Steril 83:1607–1611
Wang YA, Sullivan EA, Black D, Dean J, Bryant J, Chapman M (2005) Preterm birth and low birth weight after assisted reproductive technology-related pregnancy in Australia between 1996 and 2000. Fertil Steril 83:1650–1658
Navot D, Bergh PA, Laufer N (1992) Ovarian hyperstimulation syndrome in novel reproductive technologies: prevention and treatment. Fertil Steril 58:249–261
Golan A, Ron-El R, Soffer Y, Weinraub Z, Caspi E (1989) Ovarian hyperstimulation syndrome: an update review. Obstet Gynecol Surv 44:430–440
Smitz J, Camus M, Devroey P, Erard P, Wisanto A, Van Steirteghem AC (1990) Incidence of severe ovarian hyperstimulation syndrome after GnRH agonist/HMG superovulation for in vitro fertilization. Hum Reprod 5:993–997
Schenker JG, Weinstein D (1978) Ovarian hyperstimulation syndrome: a current survey. Fertil Steril 30:255–268
Aboulghar MA, Mansour RT, Serour GI et al (1992) Follicular aspiration does not protect against the development of ovarian hyperstimulation syndrome. J Assist Reprod Genet 9:238–243
Delvigne A, Dubois M, Battheu B et al (1993) The ovarian hyperstimulation syndrome in in vitro fertilization: a Belgian multicentric study. II. Multiple discriminant analysis for risk prediction. Hum Reprod 8:1361–1366
Ragni G, Vegetti W, Riccaboni A, Engl B, Brigante C, Crosignani PG (2005) Comparison of GnRH agonists and antagonists in assisted reproduction cycles of patients at high risk of ovarian hyperstimulation syndrome. Hum Reprod 20:2421–2425
Ferraretti AP, Gianaroli L, Magli C, Fortini D, Selman HA, Feliciani E (1999) Elective cryopreservation of all pronucleate embryos in women at risk of ovarian hyperstimulation syndrome: efficiency and safety. Hum Reprod 14:1457–1460
Gianaroli L, Ferraretti AP, Fiorentino A (1996) The ovarian hyperstimulation syndrome. Reprod Med Rev 5:169–184
Gonen Y, Balakier H, Powel W, Casper RF (1990) Use of gonadotrophin releasing hormone agonist to trigger follicular maturation for in vitro fertilization. J Clin Endocrinol Metab 71:918–922
Tomazevic T, Meden-Vrtovec H (1996) Early timed follicular aspiration prevents severe ovarian hyperstimulation syndrome. J Assist Reprod Genet 13:282–286
Koenig E, Bussen S, Suetterlin M, Stteck T (1998) Prophylactic intravenous hydroxylethyl starch solution prevents moderate-severe ovarian hyperstimulation in in vitro fertilization patients: a prospective randomized, doubleblind and placebo-controlled study. Hum Reprod 13:2421–2424
Edwards RG, Lobo R, Bouchard P (1996) Time to revolutionize ovarian stimulation. Hum Reprod 11:917–919
Edwards B (2007) IVF, IVM, natural cycle IVF, minimal stimulation IVF—time for a rethink. RBM online 15:106–119
Nargund G, Fauser BCJM, Macklon NS, Ombelet W, Nygren K, Frydman R (2007) For the Rotterdam ISMAAR consensus group on terminology for ovarian stimulation for IVF: the ISMAAR proposal on terminology for ovarian stimulation for IVF. Hum Reprod 22:2801–2804
Tozer AJ, Iles RK, Iammarrone E, Gillott CM, Al-Shawaf T, Grudzinskas JG (2004) The effects of ‘coasting’ on follicular fluid concentrations of vascular endothelial growth factor in women at risk of developing ovarian hyperstimulation syndrome. Hum Reprod 19:522–528
Chen C-D, Chao KH, Yang J-H (2003) Comparison of coasting and intravenous albumin in the prevention of ovarian hyperstimulation syndrome. Fertil Steril 80:86–90
Youssef MA, Van der Veen F, Al-Inany HG, Griesinger G, Mochtar MH, van Wely M (2011) Gonadotropin-releasing hormone agonist versus hCG for oocyte triggering in antagonist assisted reproductive technology cycles. Cochrane Database Syst Rev 1:CD008046
Kol S, Itskovitz-Eldor J (2010) Gonadotropin-releasing hormone agonist trigger: the way to eliminate ovarian hyperstimulation syndrome—a 20-year experience. Semin Reprod Med 28:500–505
Kol S, Humaidan P (2013) GnRH agonist triggering: recent developments. Reprod Biomed Online 26:226–230
Youssef MA, van Wely M, Hassan MA et al (2010) Can dopamine agonists reduce the incidence and severity of OHSS in IVF/ICSI treatment cycles? a systematic review and meta-analysis. Hum Reprod Update 16:459–466
Whelan JG, Vlahos NF (2000) The ovarian hyperstimulation syndrome. Fertil Steril 73(883–89):6
Ulug U, Bahceci M, Erden HF, Shalev E, Ben-Shlomo I (2002) The significance of coasting duration during ovarian stimulation for conception in assisted fertilization cycles. Hum Reprod 17:310–313
Blondin P, Guilbault LA, Sirard MA (1997) The time interval between FSH-P administration and slaughter can influence the developmental competence of beef heifer oocytes. Theriogenology 48:803–813
Krasnow JS, Berga SL, Guzick DS, Zeleznik AJ, Yeo KT (1996) Vascular permeability factor and vascular endothelial growth factor in ovarian hyperstimulation: a preliminary report. Fert Steril 65:552–555
Fluker MR, Copeland JE, Yuzpe AA (2000) An ounce of prevention: outpatient management of the ovarian hyperstimulation syndrome. Fertil Steril 73:821–824
Carizza C, Abdelmassih V, Abdelmassih S et al (2008) Cabergoline reduces the early onset of ovarian hyperstimulation syndrome: a prospective randomized study. Reprod Biomed Online 17:751–755
Tehraninejad ES, Hafezi M, Arabipoor A, Aziminekoo E, Chehrazi M, Bahmanabadi A (2010) Comparison of cabergoline and intravenous albumin in the prevention of ovarian hyperstimulation syndrome: a randomized clinical trial. J Assist Reprod Genet 29:259–264
Gómez R, Soares SR, Busso C, Garcia-Velasco JA, Simón C, Pellicer A (2010) Physiology andpathology of ovarian hyperstimulation syndrome. Semin Reprod Med 28:448–457
Aboulghar M, Evers JH, Al-Inany H (2002) Intravenous albumin for preventing severe ovarian hyperstimulation syndrome: a Cochrane review. Hum Reprod 17:3027–3032
Jee BC, Suh CS, Kim YB, Kim SH, Choi YM, Kim JG, Moon SY (2010) Administration of intravenous albumin around the time of oocyte retrieval reduces pregnancy rate without preventing ovarian hyperstimulation syndrome: a systematic review and meta-analysis. Gynecol Obstet Invest 70:47–54
Youssef MA, Al-Inany HG, Evers JL, Aboulghar M (2011) Intravenous fluids for the prevention of severe ovarian hyperstimulation syndrome. Cochrane Database Syst Rev 2:CD001302
Devroey P, Bourgain C, Macklon NS, Fauser BC (2004) Reproductive biology and IVF: ovarian stimulation and endometrial receptivity. Trends Endocrinol Metab 15:84–90
Beckers NG, Platteau P, Eijkemans MJ et al (2006) The early luteal phase administration of oestrogen and progesterone does not induce premature luteolysis in normo-ovulatory women. Eur J Endocrinol 155:355–363
Baart EB, Martini E, Eijkemans MJ et al (2007) Milder ovarian stimulation for in vitro fertilization reduces aneuploidy in the human preimplantation embryo: a randomized controlled trial. Hum Reprod 22:980–988
Westergaard LG, Erb K, Laursen S, Rasmussen PE, Rex S (1996) The effect of human menopausal gonadotropin and highly purified, urine-derived follicle stimulating hormone on the outcome of in vitro fertilisation in down regulated normogonadotropic women. Hum Reprod 11:1209–1213
Westergaard LG, Laurse SB, Anderson CY (2000) Increased risk of early pregnancy loss by profound suppression on luteinizing hormone during ovarian stimulation in normogonadotrophic women undergoing assisted reproduction. Hum Reprod 15:1003–1008
Fleming R, Lloyd F, Herbert M, Fenwick J, Griffiths T, Murdoch A (1998) Effects of profound suppression of luteinizing hormone during ovarian stimulation on follicular activity, oocyte and embryo function in cycles stimulated with purified follicle stimulating hormone. Hum Reprod 13:1788–1792
Janssens RMJ, Lambalk CB, Vermiden JPW et al (2000) Dose-finding study of triptorelin acetate for prevention of a premature LH surge in IVF: a prospective, randomised, double-blind placebo-controlled study. Hum Reprod 15:2333–2340
Cedrin-Durnerin I (2004) Antagonist protocols: residual LH levels and the value of exogenous LH supplementation. J Gynecol Obstet Biol Reprod (Paris) 33:3S29–3S31
Urman B, Fluker MR, Yuen BH, Fleige-Zahradka BG, Zouves CG, Moon YS (1992) The outcome of in vitro fertilization and embryo transfer in women with polycystic ovary syndrome failing to conceive after ovulation induction with exogenous gonadotropins. Fertil Steril 57:1269–1273
Homburg R, Berkowitz D, Levy T, Feldberg D, Ashkenazi J, Ben-Rafael Z (1993) In vitro fertilization and embryo transfer for the treatment of infertility associated with polycystic ovary syndrome. Fertil Steril 60:858–863
Doldi N, Marsiglio E, Destefani A, Gessi A, Merati G, Ferrari A (1999) Elevated serum progesterone on the day of hCG administration in IVF is associated with a higher pregnancy rate in polycystic ovary syndrome. Hum Reprod 14:601–605
Kodama H, Fukuda J, Karube H, Matsui T, Shimizu Y, Tanaka T (1995) High incidence of embryo transfer cancellations in patients with polycystic ovarian syndrome. Hum Reprod 10:1962–1967
Marci R, Senn A, Dessole S, Chanson A, Loumaye E, Grandi P, Germond M (2001) A low-dose stimulation protocol using highly purified follicle-stimulating hormone can lead to high pregnancy rates in in vitro fertilization patients with polycystic ovaries who are at risk of a high ovarian response to gonadotropins. Fertil Steril 75:1131–1135
Sundstrom P, Nilsson BO (1988) Meiotic and cytoplasmic maturation of oocytes collected in stimulated cycles is asynchronous. Hum Reprod 3:613–619
Moor RM, Osborn JC, Crosby IM (1985) Gonadotrophin-induced abnormalities in sheep oocytes after superovulation. J Reprod Fertil 74:167–172
Tesarik J, Mendoza C (1995) Nongenomic effects of 17b-estradiol on maturing human oocytes: relationship to oocyte developmental potential. J Clin. Endocrino Metab 80:1438–1443
Tesarik J, Mendoza C (1997) Direct non-genomic effects of follicular steroids on maturing human oocytes: oestrogen versus androgen antagonism. Hum Reprod Update 3:95–100
Conflict of interest
The authors L. Rinaldi, F. Lisi, and H. Selman declare that they have no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Rinaldi, L., Lisi, F. & Selman, H. Mild/minimal stimulation protocol for ovarian stimulation of patients at high risk of developing ovarian hyperstimulation syndrome. J Endocrinol Invest 37, 65–70 (2014). https://doi.org/10.1007/s40618-013-0021-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40618-013-0021-1