Abstract
Purpose of Review
Children’s environmental health researchers are increasingly interested in identifying time intervals during which individuals are most susceptible to adverse impacts of environmental exposures. We review recent advances in methods for assessing susceptible periods.
Recent Findings
We identified three general classes of modeling approaches aimed at identifying susceptible periods in children’s environmental health research: multiple informant models, distributed lag models, and Bayesian approaches. Benefits over traditional regression modeling include the ability to formally test period effect differences, to incorporate highly time-resolved exposure data, or to address correlation among exposure periods or exposure mixtures.
Summary
Several statistical approaches exist for investigating periods of susceptibility. Assessment of susceptible periods would be advanced by additional basic biological research, further development of statistical methods to assess susceptibility to complex exposure mixtures, validation studies evaluating model assumptions, replication studies in different populations, and consideration of susceptible periods from before conception to disease onset.
Similar content being viewed by others
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Barr M Jr, DeSesso JM, Lau CS, Osmond C, Ozanne SE, Sadler TW, et al. Workshop to identify critical windows of exposure for children’s health: cardiovascular and endocrine work group summary. Environ Health Perspect. 2000;108(Suppl 3):569–71.
Selevan SG, Kimmel CA, Mendola P. Identifying critical windows of exposure for children’s health. Environ Health Perspect. 2000;108(Suppl 3):451–5.
NIEHS (2012) Advancing science, improving health: a plan for environmental health research.
Braun JM, Gray K. Challenges to studying the health effects of early life environmental chemical exposures on children’s health. PLoS Biol. 2017;15(12):e2002800.
Hamra GB, Buckley JP. Environmental exposure mixtures: questions and methods to address them. Curr Epidemiol Rep. 2018;5(2):160–5.
Stafoggia M, Breitner S, Hampel R, Basagana X. Statistical approaches to address multi-pollutant mixtures and multiple exposures: the state of the science. Curr Environ Health Rep. 2017;4(4):481–90.
Larsen WJ. Human embryology. Philadelphia: Churchill Livingstone; 2001.
Kim JH, Scialli AR. Thalidomide: the tragedy of birth defects and the effective treatment of disease. Toxicol Sci. 2011;122(1):1–6.
Goderis J, De Leenheer E, Smets K, Van Hoecke H, Keymeulen A, Dhooge I. Hearing loss and congenital CMV infection: a systematic review. Pediatrics. 2014;134(5):972–82.
Rawlinson WD, Boppana SB, Fowler KB, Kimberlin DW, Lazzarotto T, Alain S, et al. Congenital cytomegalovirus infection in pregnancy and the neonate: consensus recommendations for prevention, diagnosis, and therapy. Lancet Infect Dis. 2017;17(6):e177–e88.
Diderichsen F, Hallqvist J, Whitehead M. Differential vulnerability and susceptibility: how to make use of recent development in our understanding of mediation and interaction to tackle health inequalities. Int J Epidemiol 2018.
Raz R, Roberts AL, Lyall K, Hart JE, Just AC, Laden F, et al. Autism spectrum disorder and particulate matter air pollution before, during, and after pregnancy: a nested case-control analysis within the Nurses’ Health Study II Cohort. Environ Health Perspect. 2015;123(3):264–70.
Kalkbrenner AE, Windham GC, Serre ML, Akita Y, Wang X, Hoffman K, et al. Particulate matter exposure, prenatal and postnatal windows of susceptibility, and autism spectrum disorders. Epidemiology (Cambridge, Mass). 2015;26(1):30–42.
•• Chen YH, Ferguson KK, Meeker JD, McElrath TF, Mukherjee B. Statistical methods for modeling repeated measures of maternal environmental exposure biomarkers during pregnancy in association with preterm birth. Environ Health. 2015;14:9 Compares several methods for examining susceptible periods with repeated biomarker measures in relation to a time-fixed binary outcome.
Sanchez BN, Hu H, Litman HJ, Tellez-Rojo MM. Statistical methods to study timing of vulnerability with sparsely sampled data on environmental toxicants. Environ Health Perspect. 2011;119(3):409–15.
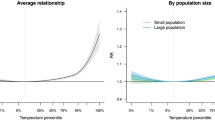
• Wilson A, Chiu YM, Hsu HL, Wright RO, Wright RJ, Coull BA. Potential for Bias when estimating critical windows for air pollution in children’s health. Am J Epidemiol. 2017;186(11):1281–9 Allows for the timing of susceptible periods to depend on a modifier.
Gasparrini A. Modeling exposure-lag-response associations with distributed lag non-linear models. Stat Med. 2014;33(5):881–99.
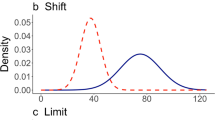
•• Wilson A, Chiu YM, Hsu HL, Wright RO, Wright RJ, Coull BA. Bayesian distributed lag interaction models to identify perinatal windows of vulnerability in children’s health. Biostatistics (Oxford, England). 2017;18(3):537–52 Demonstrates bias when using trimester-averaged exposure that is not present when using distributed lag models to identify susceptible periods.
• Liu SH, Bobb JF, Lee KH, Gennings C, Claus Henn B, Bellinger D, et al. Lagged kernel machine regression for identifying time windows of susceptibility to exposures of complex mixtures. Biostatistics. 2018;19(3):325–41 Examines periods of susceptibility to exposure mixtures using a highly flexible extension of distributed lag models based on Bayesian Kernel Machine Regression.
Warren J, Fuentes M, Herring A, Langlois P. Spatial-temporal modeling of the association between air pollution exposure and preterm birth: identifying critical windows of exposure. Biometrics. 2012;68(4):1157–67.
Horton NJ, Laird NM, Zahner GEP. Use of multiple informant data as a predictor in psychiatric epidemiology. Int J Methods Psychiatr Res. 1999;8(1):6–18.
Litman HJ, Horton NJ, Hernandez B, Laird NM. Incorporating missingness for estimation of marginal regression models with multiple source predictors. Stat Med. 2007;26(5):1055–68.
Stacy SL, Papandonatos GD, Calafat AM, Chen A, Yolton K, Lanphear BP, et al. Early life bisphenol a exposure and neurobehavior at 8 years of age: identifying windows of heightened vulnerability. Environ Int. 2017;107:258–65.
Vuong AM, Yolton K, Poston KL, Xie C, Webster GM, Sjodin A, et al. Prenatal and postnatal polybrominated diphenyl ether (PBDE) exposure and measures of inattention and impulsivity in children. Neurotoxicol Teratol. 2017;64:20–8.
Vuong AM, Yolton K, Xie C, Webster GM, Sjodin A, Braun JM, et al. Childhood polybrominated diphenyl ether (PBDE) exposure and neurobehavior in children at 8 years. Environ Res. 2017;158:677–84.
Braun JM, Chen A, Hoofnagle A, Papandonatos GD, Jackson-Browne M, Hauser R, et al. Associations of early life urinary triclosan concentrations with maternal, neonatal, and child thyroid hormone levels. Horm Behav. 2018;101:77–84.
Vuong AM, Braun JM, Webster GM, Thomas Zoeller R, Hoofnagle AN, Sjodin A, et al. Polybrominated diphenyl ether (PBDE) exposures and thyroid hormones in children at age 3years. Environ Int. 2018;117:339–47.
Vuong AM, Braun JM, Yolton K, Wang Z, Xie C, Webster GM, et al. Prenatal and childhood exposure to perfluoroalkyl substances (PFAS) and measures of attention, impulse control, and visual spatial abilities. Environ Int. 2018;119:413–20.
Vuong AM, Yolton K, Poston KL, Xie C, Webster GM, Sjodin A, et al. Childhood polybrominated diphenyl ether (PBDE) exposure and executive function in children in the HOME Study. Int J Hyg Environ Health. 2018;221(1):87–94.
Vuong AM, Yolton K, Wang Z, Xie C, Webster GM, Ye X, et al. Childhood perfluoroalkyl substance exposure and executive function in children at 8years. Environ Int. 2018;119:212–9.
Zhang H, Yolton K, Webster GM, Ye X, Calafat AM, Dietrich KN, et al. Prenatal and childhood perfluoroalkyl substances exposures and children’s reading skills at ages 5 and 8years. Environ Int. 2018;111:224–31.
Jackson-Browne MS, Papandonatos GD, Chen A, Calafat AM, Yolton K, Lanphear BP, et al. Identifying vulnerable periods of neurotoxicity to triclosan exposure in children. Environ Health Perspect. 2018;126(5):057001.
Stacy SL, Papandonatos GD, Calafat AM, Chen A, Yolton K, Lanphear BP, et al. Early life bisphenol a exposure and neurobehavior at 8years of age: identifying windows of heightened vulnerability. Environ Int 2017.
Gasparrini A, Scheipl F, Armstrong B, Kenward MG. A penalized framework for distributed lag non-linear models. Biometrics. 2017.
Chiu YH, Hsu HH, Coull BA, Bellinger DC, Kloog I, Schwartz J, et al. Prenatal particulate air pollution and neurodevelopment in urban children: examining sensitive windows and sex-specific associations. Environ Int. 2016;87:56–65.
Hsu HH, Chiu YH, Coull BA, Kloog I, Schwartz J, Lee A, et al. Prenatal particulate air pollution and asthma onset in urban children. Identifying sensitive windows and sex differences. Am J Respir Crit Care Med. 2015;192(9):1052–9.
Martens DS, Cox B, Janssen BG, Clemente DBP, Gasparrini A, Vanpoucke C, et al. Prenatal air pollution and newborns’ predisposition to accelerated biological aging. JAMA Pediatr. 2017;171(12):1160–7.
Raz R, Levine H, Pinto O, Broday DM, Yuval, Weisskopf MG. Traffic-related air pollution and autism spectrum disorder: a population-based nested case-control study in Israel. Am J Epidemiol. 2018;187(4):717–25.
Vicedo-Cabrera AM, Olsson D, Forsberg B. Exposure to seasonal temperatures during the last month of gestation and the risk of preterm birth in Stockholm. Int J Environ Res Public Health. 2015;12(4):3962–78.
Vicedo-Cabrera AM, Iniguez C, Barona C, Ballester F. Exposure to elevated temperatures and risk of preterm birth in Valencia, Spain. Environ Res. 2014;134:210–7.
Benmarhnia T, Auger N, Stanislas V, Lo E, Kaufman JS. The relationship between apparent temperature and daily number of live births in Montreal. Matern Child Health J. 2015;19(12):2548–51.
Cox B, Vicedo-Cabrera AM, Gasparrini A, Roels HA, Martens E, Vangronsveld J, et al. Ambient temperature as a trigger of preterm delivery in a temperate climate. J Epidemiol Community Health. 2016.
Claus Henn B, Austin C, Coull BA, Schnaas L, Gennings C, Horton MK, et al. Uncovering neurodevelopmental windows of susceptibility to manganese exposure using dentine microspatial analyses. Environ Res. 2018;161:588–98.
• Bello GA, Arora M, Austin C, Horton MK, Wright RO, Gennings C. Extending the distributed lag model framework to handle chemical mixtures. Environ Res. 2017;156:253–64 Extends distributed lag models to address periods of susceptibility to exposure mixtures using weighted quantile sum or tree-based methods.
Welty LJ, Peng RD, Zeger SL, Dominici F. Bayesian distributed lag models: estimating effects of particulate matter air pollution on daily mortality. Biometrics. 2009;65(1):282–91.
Roberts EM, English PB. Bayesian modeling of time-dependent vulnerability to environmental hazards: an example using autism and pesticide data. Stat Med. 2013;32(13):2308–19.
Lee A, Leon Hsu HH, Mathilda Chiu YH, Bose S, Rosa MJ, Kloog I, et al. Prenatal fine particulate exposure and early childhood asthma: effect of maternal stress and fetal sex. J Allergy Clin Immunol. 2018;141(5):1880–6.
Chiu YM, Hsu HL, Wilson A, Coull BA, Pendo MP, Baccarelli A, et al. Prenatal particulate air pollution exposure and body composition in urban preschool children: examining sensitive windows and sex-specific associations. Environ Res. 2017;158:798–805.
Bose S, Chiu YM, Hsu HL, Di Q, Rosa MJ, Lee A, et al. Prenatal nitrate exposure and childhood asthma. Influence of maternal prenatal stress and fetal sex. Am J Respir Crit Care Med. 2017;196(11):1396–403.
Brunst KJ, Sanchez-Guerra M, Chiu YM, Wilson A, Coull BA, Kloog I, et al. Prenatal particulate matter exposure and mitochondrial dysfunction at the maternal-fetal interface: effect modification by maternal lifetime trauma and child sex. Environ Int. 2018;112:49–58.
Warren J, Fuentes M, Herring A, Langlois P. Bayesian spatial-temporal model for cardiac congenital anomalies and ambient air pollution risk assessment. Environmetrics. 2012;23(8):673–84.
Warren JL, Fuentes M, Herring AH, Langlois PH. Air pollution metric analysis while determining susceptible periods of pregnancy for low birth weight. ISRN Obstet Gynecol. 2013;2013:387452.
Warren JL, Stingone JA, Herring AH, Luben TJ, Fuentes M, Aylsworth AS, et al. Bayesian multinomial probit modeling of daily windows of susceptibility for maternal PM2.5 exposure and congenital heart defects. Stat Med. 2016;35(16):2786–801.
• Chang HH, Warren JL, Darrow LA, Reich BJ, Waller LA. Assessment of critical exposure and outcome windows in time-to-event analysis with application to air pollution and preterm birth study. Biostatistics. 2015;16(3):509–21 Addresses susceptible periods when the outcome is time-varying.
Perrier F, Giorgis-Allemand L, Slama R, Philippat C. Within-subject pooling of biological samples to reduce exposure misclassification in biomarker-based studies. Epidemiology (Cambridge, Mass). 2016;27(3):378–88.
Kuchenhoff H, Mwalili SM, Lesaffre E. A general method for dealing with misclassification in regression: the misclassification SIMEX. Biometrics. 2006;62(1):85–96.
Cole SR, Chu H, Greenland S. Multiple-imputation for measurement-error correction. Int J Epidemiol. 2006;35(4):1074–81.
Rosner B, Willett WC, Spiegelman D. Correction of logistic regression relative risk estimates and confidence intervals for systematic within-person measurement error. Stat Med. 1989;8(9):1051–69 discussion 71–3.
Gore AC, Chappell VA, Fenton SE, Flaws JA, Nadal A, Prins GS, et al. EDC-2: the endocrine society’s second scientific statement on endocrine-disrupting chemicals. Endocr Rev. 2015;36(6):E1–E150.
Carlin DJ, Rider CV, Woychik R, Birnbaum LS. Unraveling the health effects of environmental mixtures: an NIEHS priority. Environ Health Perspect. 2013;121(1):A6–8.
Braun JM, Gennings C, Hauser R, Webster TF. What can epidemiological studies tell us about the impact of chemical mixtures on human health? Environ Health Perspect. 2016;124(1):A6–9.
Warren JL, Son JY, Pereira G, Leaderer BP, Bell ML. Investigating the impact of maternal residential mobility on identifying critical windows of susceptibility to ambient air pollution during pregnancy. Am J Epidemiol. 2018;187(5):992–1000.
Dionisio KL, Chang HH, Baxter LK. A simulation study to quantify the impacts of exposure measurement error on air pollution health risk estimates in copollutant time-series models. Environ Health. 2016;15(1):114.
Keller JP, Drton M, Larson T, Kaufman JD, Sandler DP, Szpiro AA. Covariate-adaptive clustering of exposures for air pollution epidemiology cohorts. Ann Appl Stat. 2017;11(1):93–113.
Weisskopf MG, Seals RM, Webster TF. Bias amplification in epidemiologic analysis of exposure to mixtures. Environ Health Perspect. 2018;126(4):047003.
Funding
JPB and GBH: 5U24OD023382
JMB: R01 ES025214, R01 ES024381, R01 ES027408, and UG3 OD023313
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Joseph M. Braun was financially compensated for serving as an expert witness for plaintiffs in litigation related to tobacco smoke exposures. Jessie P. Buckley and Ghassan B. Hamra report grants from NIH during the conduct of the study.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Methods in Environmental Epidemiology
Rights and permissions
About this article
Cite this article
Buckley, J.P., Hamra, G.B. & Braun, J.M. Statistical Approaches for Investigating Periods of Susceptibility in Children’s Environmental Health Research. Curr Envir Health Rpt 6, 1–7 (2019). https://doi.org/10.1007/s40572-019-0224-5
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40572-019-0224-5