Opinion statement
It was originally thought that, as all betalactams share a four-member ring, they would cross-react, and so the classical recommendation was for allergic patients to avoid all betalactams. However, later studies found that some individuals selectively responded to one betalactam only and tolerated others. This was shown to be more frequent than initially thought, and this finding has led to a change from the initial recommendations of complete avoidance. Selective responses to amoxicillin are mainly due to recognition of the side chain structure, making benzylpenicillin a safe alternative. These amoxicillin-selective responders comprise up to 55 and 90 % of patients with immediate allergic reactions to amoxicillin and amoxicillin-clavulanic, respectively. Additionally, more than 85 % of penicillin-allergic patients can tolerate cephalosporins with different R1 side chains, decreasing to 65 % if the side chain is identical. It is known that third and fourth generation cephalosporins are well tolerated by penicillin-allergic patients, probably because their chemical structures differ more from penicillins that those from the first generation. In patients with IgE-mediated allergic reactions to cephalosporins, penicillins can be an alternative treatment in up to 75 % of cases. Moreover, 40 % of patients primarily sensitized to a given cephalosporin also react to others, which might be because some cephaloporins have the same (ceftriaxone and cefotaxime) or very similar (ceftriaxone and cefuroxime) side chain structures. Finally, carbapenems and monobactams are good alternative for patients with penicillin and/or cephalosporin allergy because cross-reactivity occurs in <1 % of these cases. For all betalactams, tolerance is higher in T-cell-mediated reactions than IgE-mediated. These results show that alternative treatments for infectious disease are available to patients with allergic reactions to betalactams, from within the same group of antibiotics. Nevertheless, this general rules need to be analyzed patient by patient, and skin tests and graded challenge with the betalactam that is going to be administered are recommended.
Keypoints
• Patients with IgE- or T-cell-mediated allergy to betalactams can have selective reactions, specific to one betalactam with good tolerance to others, or be cross-reactive, recognizing several different chemically related betalactams.
• The percentage of selective reactions to the different betalactam compounds is higher than previously reported and patients should be studied in order to increase the treatment options available.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Drug reactions with an immunological basis or allergic drug reactions account for 6–10 % of all adverse drug reactions [1]. They can be induced by heterogeneous compounds with very different chemical structures, and one of the most frequent culprits is antibiotics, especially betalactams (BL) [2].
BL allergy is overestimated, and <40 % of the cases initially considered allergic are confirmed [2]. This diagnosis, real or not, led to the use of alternative and more expensive antibiotics with more adverse effects, potentially leading to bacterial resistance and longer hospital stays [3•]. This allergic response, whether IgE- or T-cell-mediated, can be specific to one BL, with the patient having good tolerance to others, or cross-reactive, with the patient reacting to different BLs. From a clinical point of view, the term BL cross-reactivity implicates the possibility of reacting to a BL that is different to the one inducing the primary sensitization, but chemically related.
Immunochemistry
To analyze clinical cross-reactivity, it is necessary to understand the basic aspects of the chemical structures, the degradation pathways, and immunological recognition.
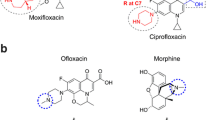
BL chemical structure
BLs have a common four-member BL ring, which provides the antibacterial activity, and are classified into different groups: penicillins, cephalosporins, monobactams, carbapenems, and clavams (Fig. 1). In all except monobactams, the BL ring is condensed to another different ring: in penicillins, a five-member sulfur ring (thiazolidine); in cephalosporins, a six-member sulfur ring (dihydrothiazine); in carbapenems, a five-member ring (dihydropyrrole); and in clavams, a five-member oxygen ring (oxazolidine). Both fused rings taken together (the bicyclic structure) constitute the core, or nuclear region, of every BL group.
Moreover, all these antibiotics, except clavams, display different R substituents, also called side chains. In all cases, a side chain (R or R1) is bound to the BL ring, and cephalosporins and carbapenems contain additional side chains (R2 and/or R3) associated with the second ring.
BL antigenic determinants
The formation of the antigenic determinants of BLs requires the nucleophilic attack at the BL carbonyl by the amino groups of the protein, leading to the drug–protein adduct (Fig. 2). For benzylpenicillin (BP), a number of products have been described such as the benzylpenicilloyl (BPO), formed after its spontaneous conjugation to proteins and represents 95 % of the antibody recognition [4]. The remaining percentage is formed by structures produced after metabolism (benzylpenicillenate, benzylpenicilloic acid, benzylpenicillanyl, benzylpenamaldate, benzylpenaldate, d-benzylpenicillamine, and benzylpenicilloyl), which have not been fully characterized immunochemically [5]. The production of monoclonal antibodies helped to characterize BP and amoxicillin (AX) antigenic determinants [6, 7], with three different epitopes identified (the side chain, the thiazolidine ring, and the part that results from the conjugation of BL to the protein carrier), although these regions can overlap [7].
Although penicillins and cephalosporins share the BL ring, there are big differences in the determinants they produce after binding to a protein carrier because of their different degradation processes. Cephalosporins undergo fragmentation of the BL and dihydrothiazine rings, and the resultant compounds are extremely unstable with cephalosporoyl adducts degrading through dihydrothiazine ring rupture, with the expulsion of R2 the substituent, leading to multiple structures that have not been well defined [8, 9]. This unresolved question, as well as whether R1 and/or R2 side chains are part of the antigenic determinant, may have important implications for the allergic response. In the majority of clinically relevant cephalosporins, the presence of a good leaving group at the 3′ position (—CH2—R2 side chain) increases the reactivity of the BL via the elimination of R2. However, for other cephalosporins such as cefaclor, ceftizoxime, cefrodaxime, cefadroxil, cephalexin, and cephradine, there is no R2 group at the 3′ position, but instead a substituent (e.g., chloride, methyl, or methoxy) whose expulsion is not so evident [10]. Regardless of the reactivity of R2, there is clinical evidence that the R1 side chain may form part of the antigenic determinant and contribute to IgE induction and cross-reactivity.
Carbapenems differ from penicillins in that their five-member ring is unsaturated and contains a carbon atom instead of sulfur. They form adducts that include a stable dihydropyrrole ring structure leading to a high density of homogeneous epitopes [11].
Monobactams contain a monocyclic BL ring. The only commercially available compound is aztreonam, which has the same side chain as ceftazidime [12].
Finally, for clavams, the only available compound is clavulanic acid (CLV), which is prescribed in combination with AX. Its structure presents an increased chemical reactivity due to its bicyclic structure, which lacks an R side chain substituent in its BL ring, and the presence of an exo-p-hydroxyethylidene function at C-2. The resulting adducts show a high instability due to a complex degradation pathways that leads to multiple possible determinants [11].
BL immunological recognition
The antigenic determinants described above can be involved in IgE and T cell allergic reactions, and the details of the immunological recognition have been more highly studied using penicillins. Early studies from Levine indicated that IgE antibodies to BPO recognize both BP and part of the carrier protein [13]. However, later studies showed that small structures such as the side chain are relevant for recognition, and this has been specifically reported with AX, in an animal model [7] and in humans [14]. Three patterns of IgE response have been described in humans: patients mainly responding to AX and it side chain p-hydroxylphenylglycine, patients mainly responding to BP, and patients who recognize BP, AX, and the nuclear part of the BL (6-aminopenicillanic) [14].
This in vitro pattern of recognition correlates with the clinical response: to AX alone (selective reactions) or to both BP and AX (cross-reacting responders). However, selective and cross-reacting are clinical concepts, and although in vitro tests can help, they are not always able to predict the response, in most cases overestimating cross-reactivity [5]. In fact, some degree of IgE recognition to BP has been found in immunoassays and basophil activation test (BAT) in patients with selective reaction to AX and good clinical tolerance to BP [5, 9, 15, 16]. As with IgE-mediated reactions, T-cell-mediated responses to aminopenicillins involve recognition of both the core structure of the BL and the whole molecule (core structure plus side chain) by T cells [17]. However, this recognition often does not correlate with the clinical response, which is in most cases selective.
Although we are far from a full understanding of cephalosporin antigenic determinants, considerable advances have been made in the precise design of well-characterized structures hypothesized to be responsible of the IgE allergic response. One study analyzed synthetic structures consisting of the R1 side chain bound to the open BL with a small fragment of the dihydrothiazine ring, without the R2 side chain. They confirmed the cross-reactivity among cephalosporins with the same (ceftriaxone, cefotaxime, and ceftazidime) or similar (cefuroxime, cefotaxime, and cephalotine) R1 side chains [18]. Differences in the immunochemistry patterns have been described for cephalosporins with an amino group in the R1 side chain, such as cefaclor and cephalexin, due to the intramolecular cyclation of these aminocephalosporins [19]. On the other hand, cross-reactivity due to similarities in R2 has not been studied extensively [5], with results having certain degree of speculation, and unable to confirm R2 as the epitope.
Less information is available for other BL. Carbapenems are able to induce the formation of specific IgG antibodies in animal models and specific IgE in exposed subjects, leading to allergic reactions [11]. Furthermore, aztreonam has been proven to be immunogenic, inducing IgG antibodies [12], and studies using monoclonal antibodies [20] revealed the importance of the side chain as they could recognize aztreonam and ceftazidime. Considering CLV, initial studies indicated a very low immunogenicity [11], although in the last decade, selective IgE-mediated reactions to this compound have been reported by BAT [21, 22••].
Alternative treatments
The increasing prevalence of bacterial resistance and the limited number of antibiotics available makes the assessment of BL cross-reactivity and the use of alternative treatments crucial for the management of infectious diseases. However, this is not an easy task due to the limited value of skin and in vitro tests, often because the degradation components have not been identified and commercialized diagnostic reagents are only available for few BLs [23]. Moreover, in vitro tests may overestimate clinical cross-reactivity and are not able to rule out the presence of coexisting antibodies with different specificities [14, 24]. Additionally, the time interval between the reaction and the study influences the sensitivity of the test, especially for selective IgE-mediated reactions [25, 26•].
The main goal for studying cross-reactivity is to determine the tolerance to BL from different or even from the same chemical group in order to find the best alternative. We will now describe clinical studies mainly based on skin tests and gradual challenge, largely focusing on IgE-mediated reactions.
Penicillin as an alternative treatment
In 1990, Blanca et al. [27, 28] described a group of patients who developed severe anaphylactic reactions to AX but had good tolerance to BP. In vitro studies confirmed that these patients had IgE antibodies that preferentially recognized the AX side chain structure [29]. These initial studies changed the paradigm that patients with hypersensitivity reactions to any particular penicillin should avoid penicillins altogether. Moreover, it was demonstrated that this response did not change even after repeated doses of BP and penicillin V treatment [30]. This observation, performed in a limited number of patients, was later confirmed in a larger population including 290 patients with proven IgE-mediated hypersensitivity reactions to penicillins [31]. This study demonstrated the importance of selective responses to AX (57.9 %) compared to cross-reactions to BLs (42.1 %) [31]. The number of cross-reactions to BP seems to be decreasing. In fact, in a recent study performed in 55 patients from the same population with IgE-mediated hypersensitivity reactions to AX-CLV, 9 % were cross-reactors to BP, whereas 62 and 29 % were selective reactors to AX and CLV, respectively [22••]. These changes in cross-reactivity likely reflect differences in the pattern of BL consumption. Additionally, in T-cell-mediated reactions to AX, the percentage of selective reactions to this BL is even higher [32, 33], and recent work suggests that it is unnecessary to perform skin testing with BP determinants in their evaluation [34].
It seems that the possibility of inducing selective responses is lower with other penicillins. A recent study of 48 Italian subjects with IgE-mediated allergic reactions to ampicillin found that only three (6.25 %) cases were selective reactors [35]. IgE allergic selective reactions to penicillin V [36–38], cloxacillin [39, 40], and piperacillin [41, 42] have also been reported for a limited number of cases. In T-cell-mediated reactions, it is worth mentioning that selective reactions to piperacillin have been described in patients with cystic fibrosis [43, 44] and as an occupational allergy [45].
Taken together, these results indicate that it is important to explore whether patients that are allergic to one penicillin can tolerate others. This has been confirmed for children [46•] and is now included in European guidelines [47].
Penicillin can also be a safe alternative in patients with allergic reactions to cephalosporins as these responses can be selective, although penicillin cross-reactivity can sometimes occur. The percentage of patients with IgE-mediated allergic reactions to cephalosporins that tolerate penicillin ranges from 50 to 90 %, differences that may be related to the culprit cephalosporin [48–51]. Tolerance to penicillin is lower with first-generation cephalosporins, probably due to the similarity in the R1 side chain chemical structure. A recent prospective study performed in 98 subjects with IgE-mediated allergic reactions to cephalosporins and skin test positive confirmed that only 25.5 % had cross-reactivity with penicillins. The risk of cross-reaction with penicillin increase threefold if the culprit cephalosporin has the same or similar side chain at the R1 position. However, others factors must be involved, since more than 50 % of cross-reactive cases responded to penicillins and cephalosporins with different side chain structures [52]. In another study including ten patients with confirmed IgE-mediated allergy to cefazolin, cross-reactivity with penicillin was only detected in 10 % of cases [51]. In children, similar figures of cross-reactivity have been found, ranging from 0.3 to 23.9 %, with the figure being higher for earlier generation cephalosporins [53].
Given that a large percentage of selective responses in penicillin-allergic patients are due to the side chain structure of AX, BP can be a safe alternative in up to 55 % of patients with IgE-mediated allergic reactions to AX and 90 % to AX-CLV. Moreover, nearly 30 % of cases with reactions to AX-CLV tolerate AX. In patients with IgE-mediated allergic reactions to cephalosporins, penicillins can be an alternative of treatment in up to 75 % of cases. Tolerance in T-cell reactions is even higher.
Cephalosporin as an alternative treatment
Cephalosporins cross-reactivity has been mainly evaluated in patients originally allergic to penicillins. Soon after cephalotin commercialization, anaphylactic reactions in patients with a history of penicillin allergy were reported [54]. The initial incidence of penicillin and cephalosporin cross-reactivity was overestimated at nearly 50 % due to contamination of cephalosporins with penicillin traces [55]. However, this percentage has gradually decreased to 12 % since the 1980s [8, 15, 56–59]. These studies also highlight the importance of the side-chain chemical structure for predicting cross-reactivity. Initial studies indicated that IgE recognizing BP cross-react with some cephalosporins, such as cephalotin and cephaloridine, which contain a similar side chain to BP, but poorly with cefuroxime and cefotaxime, which have very different side chains. In fact, cross-reactivity of penicilllins with cephamandole and cephaloridine was reported in only 10 % of cases [15], increasing to nearly 40 % for AX and cefadroxil, which have identical R1 side chains [9]. Similar results were detected between ampicillin and cephalexin, which also share the same R1 side chain [57]. A recent prospective study performed in a large number of patients confirmed these results, finding cross-reactivity in 10.9 % of cases [8]. This increased to 38 % in those with selective reactions to AX receiving cefadroxil [59]. Finally, a meta-analysis has confirmed a significant increase in allergic reactions to first-generation cephalosporins plus cefamandole [odd’s ration (OR) = 4.8; 95% confidence interval (95 %CI) = 3.7 to 6.2] but no increase with second (OR = 1.1; 95 %CI = 0.6–2.1) or third-generation cephalosporins (OR = 0.5; 95 %CI = 0.2–1.1) [60].
Data obtained from numerous studies have established different percentages of cephalosporin cross-reactivity in penicilllin-allergic patients depending on penicillin skin test results. This was 3.5–6 % in patients with positive versus 0.6–0.7 % in those with negative penicillin skin test results [15, 56, 57, 61]. This indicated a greater risk of an adverse drug reaction to cephalosporin in patients with a history of penicillin allergy and a positive penicillin skin test. On the other hand, the role of skin testing for determining cross-reactivity has not been established: It is generally agreed that a positive cephalosporin skin test in penicillin allergic patients indicates cross-reactivity, but disagreement as to whether a negative cephalosporin skin test indicates good tolerance. While some studies have found that all patients with confirmed IgE-mediated allergy to penicillin and negative skin test results with cephalosporins tolerate the administration of the latter [8], others have found that some patients with IgE-mediated selective reactions to AX and negative skin tests to cefadroxil cannot tolerate this cephalosporin [59].
Cross-reactivity is quite rare for T-cell-mediated reactions to penicillins. It has been shown that 97.2 % of 71 patients with T-cell-mediated allergy to aminopenicillins tolerate cephalosporins without an aminobenzyl side chain such as cefpodoxime or cefixime and 71.8 % also tolerate penicillin V, confirming that most are selective reactors [62].
In patients with IgE-mediated allergic reactions to cephalosporins and good tolerance to penicillins, there are two main groups: those only reacting to the culprit cephalosporin and those reacting to more than one cephalosporin. The percentage of patients reacting to one cephalosporin ranges from 57.7 to 63.2 % and the percentage of those reacting to more than one from 36.8 to 42.3 % [48, 50]. The different percentages are probably due to the cephalosporin generation involved in the reaction (selective responders) and similarities in side chain structures (cross-reactors). Taken together, these results indicate that cephalosporins are a safe option for patients with IgE-mediated allergy to penicillins, with 90 % of cases tolerating their administration, decreasing to 60 % when the R1 side chain is identical to the initial culprit. They may also be a safe option for more than 50 % of patients with IgE-mediated allergy to cephalosporins, with the R1 side chain structure being critical for predicting tolerance, although other factors appear to be involved.
Carbapenem as an alternative treatment
The incidence of carbapenem hypersensitivity is lower than 3 % [63]. The similarity in the chemical structure between penicillins and carbapenems suggests that great cross-reactivity could exist. Indeed, an early study showed that 25.6 % of penicillin-allergic patients and 47 % of those with positive penicillin skin tests had cross-reactivity with imipenem [64]. Therefore, it was initially recommended to adopt similar precautions as with penicillin when administering imipenem to penicillin-allergic patients, especially in those with positive skin tests.
However, later retrospective studies indicated that cross-reactivity was lower than initially thought, ranging from 9.2 to 11 % [63, 65, 66]. One of these [65]analyzed the medical records of 63 bone marrow transplant recipients with fever and neutropenia, and only 9.5 % developed imipenem allergy, less than for those with well-documented allergies (33 %). Other studies [63, 66] showed that the rate of carbapenem hypersensitivity was higher in those with previous penicillin allergy (ranging from 9.2 to 11 %) than in those without penicillin allergy (ranging from 2.7 to 3.9 %). It has recently been stated that patients considered allergic to penicillins are no more likely to have a reaction to carbapenem than those who were not considered allergic [67].
In the last 10 years, there has been a great interest in the elucidation of the rate of carbapenems cross-reactivity in patients with allergic reactions to penicillins. A number of prospective studies [52, 68–72, 73•, 74], most coming from the same group, have been published for adults and children with IgE-mediated allergic reactions to penicillins or to cephalosporins. Two studies evaluated patients with IgE-mediated hypersensitivity to penicillin and positive skin tests and found that 0.9 % were skin test positive to imipenem [68, 69] or meropenem [68, 69], with all skin test negative cases tolerating their administration. These results have been recently confirmed with imipenem, meropenem, and etarpenem [70]. Similar studies performed in children [71, 72] had equivalent results detecting a cross-reactivity of 0.9 % with meropenem and 0.8 % with imipenem. These low rates are likely to be due to the majority of IgE antibodies from penicillin-allergic patients recognizing specific penicillin determinants and not the shared common nuclear BL [70].
Carbapenems cross-reactivity has also been evaluated in patients with IgE-mediated hypersensitivity reactions to cephalosporins. In a prospective study [52] of 98 patients with IgE-mediated reactions and a positive skin test to cephalosporins, the rate of cross-reactivity to imipenem/cilastatin and meropenem was 1 %. A systematic review [73•] including published data on children and adults who received carbapenem indicated that cross-reactivity was lower in those with penicillin allergy (2.4 %) than in those with cephalosporin allergy (10 %), differences that could be explained by the low number of patients included in the cephalosporin group.
Regarding T-cell-mediated hypersensitivity, animal models have detected very low cross-reactivity between imipinem and other BLs [75]. Studies carried out in humans [74] found a rate of cross-reactivity between different BLs and imipenem of 5.5 %, which was higher than for IgE-mediated reactions. However, these results could not be reproduced in a large series of patients, where absence of cross-reactivity was detected [76].
These studies indicate that carbapenems can be a safe alternative in more than 99 % of patients with either IgE- or T-cell-mediated reactions to penicillins or cephalosporins.
Aztreonam as an alternative treatment
Aztreonam is generally well tolerated, only causing allergic reactions in 2.1 % of cases, and only 0.2 % are IgE-mediated [77]. Initial studies in experimental animals [12] and humans [78, 79] showed that aztreonam has a negligible cross-reactivity with penicillins [78, 79]. This has been later confirmed in various prospective studies [70, 80–82]. The most recent study found that all penicillin-allergic patients with negative skin tests to aztreonam tolerated their administration with escalating doses [70]. Similar results have been published in patients with delayed reactions to penicillins [83].
It is important to mention that cross-reactivity of aztreonam seems to be higher in patients with cystic fibrosis, probably reflecting repeated administration. In fact, in a study performed by Moss [84] on cystic fibrosis patients, 6.2 % of cases with allergy to semisynthetic penicillins had a positive skin test result to aztreonam.
Cross-reactivity between cephalosporins and aztreonam can be higher in those sharing the same side chain, as occurs with ceftazidime [85]. In a recent prospective study [52] performed in patients with IgE-mediated allergic reactions to cephalosporin and who were skin test positive, 3.06 % of cases (three patients) had positive skin tests to aztreonam (one was positive to all BL determinants tested, the other to ceftazidime, and the third to cefodizime).
These results indicate that aztreonam is a safe alternative for patients with IgE- and/or T-cell mediated penicillin allergy and for patients who are allergic to cephalosporins with different side chains.
To conclude, contrary to what was previously thought, it is clear that some BLs can be an option of treatment for patients allergic to other BLs. This is particularly the case for patients with T-cell-mediated reactions. However, chemical structure must be taken into account when selecting an alternative. Treatment options must be analyzed patient by patient, and a skin test for any BL that is going to be administered, followed by a graded challenge, is recommended.
References and Recommended Reading
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Gomes ER, Demoly P. Epidemiology of hypersensitivity drug reactions. Curr Opin Allergy Clin Immunol. 2005;5:309–16.
Dona I, Blanca-Lopez N, Torres MJ, et al. Drug hypersensitivity reactions: response patterns, drug involved, and temporal variations in a large series of patients. J Investig Allergol Clin Immunol. 2012;22:363–71.
Macy E, Contreras R. Health care use and serious infection prevalence associated with penicillin “allergy” in hospitalized patients: a cohort study. J Allergy Clin Immunol. 2014;133:790–6. This study shows that overdiagnosis of penicillin allergy, often uncofirmed, can lead to increased hospital stays, nosocomial infections and admission frequency.
Batchelor FR, Dewdney JM, Gazzard D. Penicillin allergy: the formation of the penicilloyl determinant. Nature. 1965;206:362–4.
Baldo BA. Penicillins and cephalosporins as allergens—structural aspects of recognition and cross-reactions. Clin Exp Allergy. 1999;29:744–9.
de Haan P, de Jonge AJ, Verbrugge T, et al. Three epitope-specific monoclonal antibodies against the hapten penicillin. Int Arch Allergy Appl Immunol. 1985;76:42–6.
Mayorga C, Obispo T, Jimeno L, et al. Epitope mapping of beta-lactam antibiotics with the use of monoclonal antibodies. Toxicology. 1995;97:225–34.
Romano A, Gueant-Rodriguez RM, Viola M, et al. Cross-reactivity and tolerability of cephalosporins in patients with immediate hypersensitivity to penicillins. Ann Intern Med. 2004;141:16–22.
Miranda A, Blanca M, Vega JM, et al. Cross-reactivity between a penicillin and a cephalosporin with the same side chain. J Allergy Clin Immunol. 1996;98:671–7.
Perez-Inestrosa E, Suau R, Montanez MI, et al. Cephalosporin chemical reactivity and its immunological implications. Curr Opin Allergy Clin Immunol. 2005;5:323–30.
Edwards RG, Dewdney JM, Dobrzanski RJ, et al. Immunogenicity and allergenicity studies on two beta-lactam structures, a clavam, clavulanic acid, and a carbapenem: structure-activity relationships. Int Arch Allergy Appl Immunol. 1988;85:184–9.
Adkinson Jr NF, Swabb EA, Sugerman AA. Immunology of the monobactam aztreonam. Antimicrob Agents Chemother. 1984;25:93–7.
Levine BB, Ovary Z. Studies on the mechanism of the formation of the penicillin antigen. III. The N-(D-alpha-benzylpenicilloyl) group as an antigenic determinant responsible for hypersensitivity to penicillin G. J Exp Med. 1961;114:875–904.
Moreno F, Blanca M, Mayorga C, et al. Studies of the specificities of IgE antibodies found in sera from subjects with allergic reactions to penicillins. Int Arch Allergy Immunol. 1995;108:74–81.
Blanca M, Fernandez J, Miranda A, et al. Cross-reactivity between penicillins and cephalosporins: clinical and immunologic studies. J Allergy Clin Immunol. 1989;83:381–5.
Torres MJ, Padial A, Mayorga C, et al. The diagnostic interpretation of basophil activation test in immediate allergic reactions to betalactams. Clin Exp Allergy. 2004;34:1768–75.
Padovan E, Bauer T, Tongio MM, et al. Penicilloyl peptides are recognized as T cell antigenic determinants in penicillin allergy. Eur J Immunol. 1997;27:1303–7.
Montannez MI, Mayorga C, Torres MJ, et al. Synthetic approach to gain insight into antigenic determinants of cephalosporins: in vitro studies of chemical structure-IgE molecular recognition relationships. Chem Res Toxicol. 2011;24:706–17.
Venemalm L. Pyrazinone conjugates as potential cephalosporin allergens. Bioorg Med Chem Lett. 2001;11:1869–70.
Shimizu T, Souma S, Nagakura N, et al. Epitope analysis of aztreonam by antiaztreonam monoclonal antibodies and possible consequences in beta-lactams hypersensitivity. Int Arch Allergy Immunol. 1992;98:392–7.
Sanchez-Morillas L, Perez-Ezquerra PR, Reano-Martos M, et al. Selective allergic reactions to clavulanic acid: a report of 9 cases. J Allergy Clin Immunol. 2010;126:177–9.
Torres MJ, Ariza A, Mayorga C, et al. Clavulanic acid can be the component in amoxicillin-clavulanic acid responsible for immediate hypersensitivity reactions. J Allergy Clin Immunol. 2010;125:502–05 e2. This is one of the few studies showing selective reactions to clavulanic acid. This article found that almost a third of amoxicillin-clavulanic allergic patients had good tolerance to benzylpenicillin and amoxicillin but were selective responders to clavulanic acid.
Pichichero ME. A review of evidence supporting the American Academy of Pediatrics recommendation for prescribing cephalosporin antibiotics for penicillin-allergic patients. Pediatrics. 2005;115:1048–57.
Romano A, Quaratino D, Aimone-Gastin I, et al. Cephalosporin allergy: characterization of unique and cross-reacting cephalosporin antigens. Int J Immunopathol Pharmacol. 1997;10:187–92.
Blanca M, Torres MJ, Garcia JJ, et al. Natural evolution of skin test sensitivity in patients allergic to beta-lactam antibiotics. J Allergy Clin Immunol. 1999;103:918–24.
Romano A, Gaeta F, Valluzzi RL, et al. Natural evolution of skin-test sensitivity in patients with IgE-mediated hypersensitivity to cephalosporins. Allergy. 2014;69:806–9. Study showing the prevalence of cross reactivity between penicillins and cepahlosporins as well as among cephalosporins.
Blanca M, Perez E, Garcia J, et al. Anaphylaxis to amoxycillin but good tolerance for benzyl penicillin. In vivo and in vitro studies of specific IgE antibodies. Allergy. 1988;43:508–10.
Blanca M, Vega JM, Garcia J, et al. Allergy to penicillin with good tolerance to other penicillins; study of the incidence in subjects allergic to beta-lactams. Clin Exp Allergy. 1990;20:475–81.
Sastre J, Quijano LD, Novalbos A, et al. Clinical cross-reactivity between amoxicillin and cephadroxil in patients allergic to amoxicillin and with good tolerance of penicillin. Allergy. 1996;51:383–86.
Fernandez T, Torres MJ, R-Pena R, et al. Decrease of selective immunoglobulin E response to amoxicillin despite repeated administration of benzylpenicillin and penicillin V. Clin Exp Allergy. 2005;35:1645–50.
Torres MJ, Romano A, Mayorga C, et al. Diagnostic evaluation of a large group of patients with immediate allergy to penicillins: the role of skin testing. Allergy. 2001;56:850–6.
Torres MJ, Sanchez-Sabate E, Alvarez J, et al. Skin test evaluation in nonimmediate allergic reactions to penicillins. Allergy. 2004;59:219–24.
Padial A, Antunez C, Blanca-Lopez N, et al. Non-immediate reactions to beta-lactams: diagnostic value of skin testing and drug provocation test. Clin Exp Allergy. 2008;38:822–8.
Romano A, Gaeta F, Valluzzi RL, et al. The very limited usefulness of skin testing with penicilloyl-polylysine and the minor determinant mixture in evaluating nonimmediate reactions to penicillins. Allergy. 2010;65:1104–7.
Romano A, Torres MJ, Fernandez J, et al. Allergic reactions to ampicillin. Studies on the specificity and selectivity in subjects with immediate reactions. Clin Exp Allergy. 1997;27:1425–31.
Blanca M, Carmona MJ, Moreno F, et al. Selective immediate allergic response to penicillin V. Allergy. 1996;51:961–3.
Linares T, Marcos C, Gavilan M, et al. Hypersensitivity to penicillin V with good tolerance to other beta-lactams. J Investig Allergol Clin Immunol. 2007;17:50–1.
Sanchez-Morillas L, Rojas-Perez-Ezquerra P, Gonzalez-Mendiola R, et al. Selective sensitization to Penicillin V with tolerance to other betalactams. Recent Pat Inflamm Allergy Drug Discov. 2014;8:74–6.
Dominguez-Ortega J, Martinez-Alonso JC, Marcos-Perez MC, et al. Allergy to cloxacillin with normal tolerance to amoxicillin and cefuroxime. Allergol Immunopathol (Madr). 2006;34:37–8.
Torres MJ, Blanca M, Fernandez J, et al. Selective allergic reaction to oral cloxacillin. Clin Exp Allergy. 1996;26:108–11.
Cabanas R, Munoz L, Lopez-Serrano C, et al. Hypersensitivity to piperacillin. Allergy. 1998;53:819–20.
Romano A, Di Fonso M, Viola M, et al. Selective hypersensitivity to piperacillin. Allergy. 2000;55:787.
Moss RB, Babin S, Hsu YP, et al. Allergy to semisynthetic penicillins in cystic fibrosis. J Pediatr. 1984;104:460–6.
Whitaker P, Naisbitt D, Peckham D. Nonimmediate beta-lactam reactions in patients with cystic fibrosis. Curr Opin Allergy Clin Immunol. 2012;12:369–75.
Kim JE, Kim SH, Kim JH, et al. A case of piperacillin-induced occupational anaphylaxis: detection of serum IgE to piperacillin-HSA conjugate. J Korean Med Sci. 2011;26:682–5.
Zambonino MA, Corzo JL, Munoz C, et al. Diagnostic evaluation of hypersensitivity reactions to beta-lactam antibiotics in a large population of children. Pediatr Allergy Immunol. 2014;25:80–7. Study carried out in children describing that most of cases considered to be allergic, finally tolearate BLs.
Blanca M, Romano A, Torres MJ, et al. Update on the evaluation of hypersensitivity reactions to betalactams. Allergy. 2009;64:183–93.
Romano A, Mayorga C, Torres MJ, et al. Immediate allergic reactions to cephalosporins: cross-reactivity and selective responses. J Allergy Clin Immunol. 2000;106:1177–83.
Romano A, Gueant-Rodriguez RM, Viola M, et al. Diagnosing immediate reactions to cephalosporins. Clin Exp Allergy. 2005;35:1234–42.
Antunez C, Blanca-Lopez N, Torres MJ, et al. Immediate allergic reactions to cephalosporins: evaluation of cross-reactivity with a panel of penicillins and cephalosporins. J Allergy Clin Immunol. 2006;117:404–10.
Pipet A, Veyrac G, Wessel F, et al. A statement on cefazolin immediate hypersensitivity: data from a large database, and focus on the cross-reactivities. Clin Exp Allergy. 2011;41:1602–8.
Romano A, Gaeta F, Valluzzi RL, et al. IgE-mediated hypersensitivity to cephalosporins: cross-reactivity and tolerability of penicillins, monobactams, and carbapenems. J Allergy Clin Immunol. 2010;126:994–9.
Atanaskovic-Markovic M, Velickovic TC, Gavrovic-Jankulovic M, et al. Immediate allergic reactions to cephalosporins and penicillins and their cross-reactivity in children. Pediatr Allergy Immunol. 2005;16:341–7.
Scholand JF, Tennenbaum JI, Cerilli GJ. Anaphylaxis to cephalothin in a patient allergic to penicillin. JAMA. 1968;206:130–2.
Girard JP. Common antigenic determinants of penicillin G, ampicillin and the cephalosporins demonstrated in men. Int Arch Allergy Appl Immunol. 1968;33:428–38.
Novalbos A, Sastre J, Cuesta J, et al. Lack of allergic cross-reactivity to cephalosporins among patients allergic to penicillins. Clin Exp Allergy. 2001;31:438–43.
Audicana M, Bernaola G, Urrutia I, et al. Allergic reactions to betalactams: studies in a group of patients allergic to penicillin and evaluation of cross-reactivity with cephalosporin. Allergy. 1994;49:108–13.
Apter AJ, Kinman JL, Bilker WB, et al. Is there cross-reactivity between penicillins and cephalosporins? Am J Med. 2006;119:354 e11–9.
Torres M, Blanca-Lopez N, Martin E, et al. Cross-reactivity between penicillins and cephalosporins with the same side chain: amoxicillin and cefadroxil. J Allergy Clin Immunol. 2007;119:S38.
Pichichero ME, Casey JR. Safe use of selected cephalosporins in penicillin-allergic patients: a meta-analysis. Otolaryngol Head Neck Surg. 2007;136:340–7.
Shepherd RK, Xu SA, Clark GM. Partial hearing loss in the macaque following the co-administration of kanamycin and ethacrynic acid. Hear Res. 1994;72:89–98.
Trcka J, Seitz CS, Brocker EB, et al. Aminopenicillin-induced exanthema allows treatment with certain cephalosporins or phenoxymethyl penicillin. J Antimicrob Chemother. 2007;60:107–11.
Sodhi M, Axtell SS, Callahan J, et al. Is it safe to use carbapenems in patients with a history of allergy to penicillin? J Antimicrob Chemother. 2004;54:1155–7.
Saxon A, Adelman DC, Patel A, et al. Imipenem cross-reactivity with penicillin in humans. J Allergy Clin Immunol. 1988;82:213–7.
McConnell SA, Penzak SR, Warmack TS, et al. Incidence of imipenem hypersensitivity reactions in febrile neutropenic bone marrow transplant patients with a history of penicillin allergy. Clin Infect Dis. 2000;31:1512–4.
Prescott Jr WA, DePestel DD, Ellis JJ, et al. Incidence of carbapenem-associated allergic-type reactions among patients with versus patients without a reported penicillin allergy. Clin Infect Dis. 2004;38:1102–7.
Wall GC, Nayima VA, Neumeister KM. Assessment of hypersensitivity reactions in patients receiving carbapenem antibiotics who report a history of penicillin allergy. J Chemother. 2014;26:150–3.
Romano A, Viola M, Gueant-Rodriguez RM, et al. Imipenem in patients with immediate hypersensitivity to penicillins. N Engl J Med. 2006;354:2835–7.
Romano A, Viola M, Gueant-Rodriguez RM, et al. Brief communication: tolerability of meropenem in patients with IgE-mediated hypersensitivity to penicillins. Ann Intern Med. 2007;146:266–9.
Gaeta F, Valluzzi RL, Alonzi C, et al. Tolerability of aztreonam and carbapenems in patients with IgE-mediated hypersensitivity to penicillins. J Allergy Clin Immunol. 2015. doi:10.1016/j.jaci.2014.10.011.
Atanaskovic-Markovic M, Gaeta F, Medjo B, et al. Tolerability of meropenem in children with IgE-mediated hypersensitivity to penicillins. Allergy. 2008;63:237–40.
Atanaskovic-Markovic M, Gaeta F, Gavrovic-Jankulovic M, et al. Tolerability of imipenem in children with IgE-mediated hypersensitivity to penicillins. J Allergy Clin Immunol. 2009;124:167–9.
Kula B, Djordjevic G, Robinson JL. A systematic review: can one prescribe carbapenems to patients with IgE-mediated allergy to penicillins or cephalosporins? Clin Infect Dis. 2014;59:1113–22. This sistematic review clearly states that cross-reactivity between penicillins and carbapenems is less than 3 % and betwen cephalosporins and carbapenems less than 10%.
Schiavino D, Nucera E, Lombardo C, et al. Cross-reactivity and tolerability of imipenem in patients with delayed-type, cell-mediated hypersensitivity to beta-lactams. Allergy. 2009;64:1644–8.
Nagakura N, Souma S, Shimizu T, et al. Comparison of cross-reactivities of imipenem and other beta-lactam antibiotics by delayed-type hypersensitivity reaction in guinea pigs. Chem Pharm Bull (Tokyo). 1991;39:765–8.
Romano A, Gaeta F, Valluzzi RL, et al. Absence of cross-reactivity to carbapenems in patients with delayed hypersensitivity to penicillins. Allergy. 2013;68:1618–21.
Adkinson Jr NF. Immunogenicity and cross-allergenicity of aztreonam. Am J Med. 1990;88:12S–5S. discussion 38S-42S.
Saxon A, Swabb EA, Adkinson Jr NF. Investigation into the immunologic cross-reactivity of aztreonam with other beta-lactam antibiotics. Am J Med. 1985;78:19–26.
Saxon A, Hassner A, Swabb EA, et al. Lack of cross-reactivity between aztreonam, a monobactam antibiotic, and penicillin in penicillin-allergic subjects. J Infect Dis. 1984;149:16–22.
Martin JA, Igea JM, Fraj J, et al. Allergy to amoxicillin in patients who tolerated benzylpenicillin, aztreonam, and ceftazidime. Clin Infect Dis. 1992;14:592–3.
Vega JM, Blanca M, Garcia JJ, et al. Tolerance to aztreonam in patients allergic to beta-lactam antibiotics. Allergy. 1991;46:196–202.
Patriarca G, Schiavino D, Lombardo C, et al. Tolerability of aztreonam in patients with IgE-mediated hypersensitivity to beta-lactams. Int J Immunopathol Pharmacol. 2008;21:375–9.
Buonomo A, Nucera E, De Pasquale T, et al. Tolerability of aztreonam in patients with cell-mediated allergy to beta-lactams. Int Arch Allergy Immunol. 2011;155:155–9.
Moss RB. Sensitization to aztreonam and cross-reactivity with other beta-lactam antibiotics in high-risk patients with cystic fibrosis. J Allergy Clin Immunol. 1991;87:78–88.
Perez Pimiento A, Gomez Martinez M, Minguez Mena A, et al. Aztreonam and ceftazidime: evidence of in vivo cross allergenicity. Allergy. 1998;53:624–5.
Acknowledgments
The study was funded by FIS-Thematic Networks and Cooperative Research Centres (RIRAAF/RD012/0013), Junta de Andalucía (CTS 06603, PI-0545-2010, and PI-0699-2011), ISCIII (PI12/02529), and Fundación Salud 2000 and from the People Programme (Marie Curie Actions) of the European Union’s Seventh Framework Programme (FP7/2007-2013) under REA grant agreement no. 300230. We thank James R. Perkins for help with the English language version of the manuscript.
Compliance with Ethics Guidelines
Conflict of Interest
María Isabel Montañez declares that she has no conflict of interest. Adriana Ariza declares that she has no conflict of interest. Cristobalina Mayorga declares that she has no conflict of interest. Tahia Diana Fernandez declares that she has no conflict of interest. María José Torres declares that she has no conflict of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Author information
Authors and Affiliations
Corresponding author
Additional information
This article is part of the Topical Collection on Drug Allergy
Rights and permissions
About this article
Cite this article
Montañez, M.I., Ariza, A., Mayorga, C. et al. Cross-Reactivity in Betalactam Allergy: Alternative Treatments. Curr Treat Options Allergy 2, 141–154 (2015). https://doi.org/10.1007/s40521-015-0050-4
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40521-015-0050-4