Abstract
Background
The incidence of antibiotic-related diarrhea (AAD) is high in older adults.
Aim
To examine the gut microbiota changes in older adults who received antibiotics to identify the microbial signatures associated with antibiotic use and AAD.
Methods
A nested prospective observational cohort study was conducted between December 2019 and June 2021 in patients ≥ 65 years old at Huashan Hospital affiliated with Fudan University. The patients were grouped as antibiotic-treated (HA group) and no antibiotics (HC group); the HA group was subdivided as with vs. without AAD. Fecal samples were collected at admission (i.e., before eventual antibiotics) and after 7 days.
Result
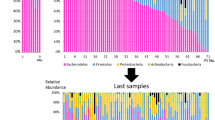
Thirty-eight and 19 participants were included in the HA and HC groups. There were significant differences in gut microbiota between the HA after antibiotics vs. HC groups, with a higher Firmicutes/Bacteroidetes ratio. Before antibiotics in the HA group, the relative abundances of Akkermansia and Alistipes were lower in the AAD subgroup than the no-AAD subgroup, while the relative abundance of Actinomyces was higher. After antibiotics in the HA group, specific bacterial species were decreased in the AAD subgroup compared with the no-AAD subgroup. Among HA participants without probiotics, the abundance of Akkermansia in the patients without AAD was higher than in the patients with AAD at baseline (P = 0.007).
Conclusion
Patients with or without AAD have different gut microbiota compositions before antibiotics. Antibiotics can lead to dysbiosis, with a decrease in beneficial bacteria and an increase in Enterococcus.









Similar content being viewed by others
Availability of data and materials
All data generated or analyzed during this study are included in this published article.
References
Giannelli FR (2017) Antibiotic-associated diarrhea. JAAPA 30:46–47. https://doi.org/10.1097/01.JAA.0000524721.01579.c9
Kyne L, Warny M, Qamar A et al (2000) Asymptomatic carriage of Clostridium difficile and serum levels of IgG antibody against toxin A. N Engl J Med 342:390–397. https://doi.org/10.1056/NEJM200002103420604
Furuya-Kanamori L, Marquess J, Yakob L et al (2015) Asymptomatic Clostridium difficile colonization: epidemiology and clinical implications. BMC Infect Dis 15:516. https://doi.org/10.1186/s12879-015-1258-4
Hicks LA, Bartoces MG, Roberts RM et al (2015) US outpatient antibiotic prescribing variation according to geography, patient population, and provider specialty in 2011. Clin Infect Dis 60:1308–1316. https://doi.org/10.1093/cid/civ076
Arizpe A, Reveles KR, Aitken SL (2016) Regional variation in antibiotic prescribing among medicare part D enrollees, 2013. BMC Infect Dis 16:744. https://doi.org/10.1186/s12879-016-2091-0
Shin JH, High KP, Warren CA (2016) Older is not wiser, immunologically speaking: effect of aging on host response to Clostridium difficile infections. J Gerontol A Biol Sci Med Sci 71:916–922. https://doi.org/10.1093/gerona/glv229
Cohen SH, Gerding DN, Johnson S et al (2010) Clinical practice guidelines for Clostridium difficile infection in adults: 2010 update by the society for healthcare epidemiology of America (SHEA) and the infectious diseases society of America (IDSA). Infect Control Hosp Epidemiol 31:431–455. https://doi.org/10.1086/651706
Gill SR, Pop M, Deboy RT et al (2006) Metagenomic analysis of the human distal gut microbiome. Science 312:1355–1359. https://doi.org/10.1126/science.1124234
Claesson MJ, Cusack S, O’Sullivan O et al (2011) Composition, variability, and temporal stability of the intestinal microbiota of the elderly. Proc Natl Acad Sci U S A 108:4586–4591. https://doi.org/10.1073/pnas.1000097107
Claesson MJ, Jeffery IB, Conde S et al (2012) Gut microbiota composition correlates with diet and health in the elderly. Nature 488:178–184. https://doi.org/10.1038/nature11319
Salazar N, Lopez P, Valdes L et al (2013) Microbial targets for the development of functional foods accordingly with nutritional and immune parameters altered in the elderly. J Am Coll Nutr 32:399–406. https://doi.org/10.1080/07315724.2013.827047
Ragonnaud E, Biragyn A (2021) Gut microbiota as the key controllers of “healthy” aging of elderly people. Immun Ageing 18:2. https://doi.org/10.1186/s12979-020-00213-w
Dogra SK, Dore J, Damak S (2020) Gut microbiota resilience: definition, link to health and strategies for intervention. Front Microbiol 11:572921. https://doi.org/10.3389/fmicb.2020.572921
O’Toole PW, Jeffery IB (2015) Gut microbiota and aging. Science 350:1214–1215. https://doi.org/10.1126/science.aac8469
O’Sullivan O, Coakley M, Lakshminarayanan B et al (2013) Alterations in intestinal microbiota of elderly Irish subjects post-antibiotic therapy. J Antimicrob Chemother 68:214–221. https://doi.org/10.1093/jac/dks348
Bartosch S, Fite A, Macfarlane GT et al (2004) Characterization of bacterial communities in feces from healthy elderly volunteers and hospitalized elderly patients by using real-time PCR and effects of antibiotic treatment on the fecal microbiota. Appl Environ Microbiol 70:3575–3581. https://doi.org/10.1128/AEM.70.6.3575-3581.2004
Jeffery IB, Lynch DB, O’Toole PW (2016) Composition and temporal stability of the gut microbiota in older persons. ISME J 10:170–182. https://doi.org/10.1038/ismej.2015.88
Clark RI, Salazar A, Yamada R et al (2015) Distinct shifts in microbiota composition during Drosophila aging impair intestinal function and drive mortality. Cell Rep 12:1656–1667. https://doi.org/10.1016/j.celrep.2015.08.004
McFarland LV (2008) Antibiotic-associated diarrhea: epidemiology, trends and treatment. Future Microbiol 3:563–578. https://doi.org/10.2217/17460913.3.5.563
Rinninella E, Raoul P, Cintoni M et al (2019) What is the healthy gut microbiota composition? A changing ecosystem across age, environment, diet, and diseases. Microorganisms. https://doi.org/10.3390/microorganisms7010014
Panda S, El khader I, Casellas F et al (2014) Short-term effect of antibiotics on human gut microbiota. PLoS One 9:e95476. https://doi.org/10.1371/journal.pone.0095476
Lloyd-Price J, Arze C, Ananthakrishnan AN et al (2019) Multi-omics of the gut microbial ecosystem in inflammatory bowel diseases. Nature 569:655–662. https://doi.org/10.1038/s41586-019-1237-9
Parnanen K, Karkman A, Hultman J et al (2018) Maternal gut and breast milk microbiota affect infant gut antibiotic resistome and mobile genetic elements. Nat Commun 9:3891. https://doi.org/10.1038/s41467-018-06393-w
Gasparrini AJ, Wang B, Sun X et al (2019) Persistent metagenomic signatures of early-life hospitalization and antibiotic treatment in the infant gut microbiota and resistome. Nat Microbiol 4:2285–2297. https://doi.org/10.1038/s41564-019-0550-2
Elvers KT, Wilson VJ, Hammond A et al (2020) Antibiotic-induced changes in the human gut microbiota for the most commonly prescribed antibiotics in primary care in the UK: a systematic review. BMJ Open 10:e035677. https://doi.org/10.1136/bmjopen-2019-035677
Ramirez J, Guarner F, Bustos Fernandez L et al (2020) Antibiotics as major disruptors of gut microbiota. Front Cell Infect Microbiol 10:572912. https://doi.org/10.3389/fcimb.2020.572912
Rashid MU, Zaura E, Buijs MJ et al (2015) Determining the long-term effect of antibiotic administration on the human normal intestinal microbiota using culture and pyrosequencing methods. Clin Infect Dis 60:S77-84. https://doi.org/10.1093/cid/civ137
Allen SJ, Wareham K, Wang D et al (2013) Lactobacilli and bifidobacteria in the prevention of antibiotic-associated diarrhoea and Clostridium difficile diarrhoea in older inpatients (PLACIDE): a randomised, double-blind, placebo-controlled, multicentre trial. Lancet 382:1249–1257. https://doi.org/10.1016/S0140-6736(13)61218-0
Jafarnejad S, Shab-Bidar S, Speakman JR et al (2016) Probiotics reduce the risk of antibiotic-associated diarrhea in adults (18–64 years) but not the elderly (>65 years): a meta-analysis. Nutr Clin Pract 31:502–513. https://doi.org/10.1177/0884533616639399
Lee KJ, Kim JH, Cho SW (2005) Gabapentin reduces rectal mechanosensitivity and increases rectal compliance in patients with diarrhoea-predominant irritable bowel syndrome. Aliment Pharmacol Ther 22:981–988. https://doi.org/10.1111/j.1365-2036.2005.02685.x
Rondanelli M, Faliva MA, Perna S et al (2017) Using probiotics in clinical practice: where are we now? A review of existing meta-analyses. Gut Microbes 8:521–543. https://doi.org/10.1080/19490976.2017.1345414
Krawczyk B, Wityk P, Galecka M et al (2021) The many faces of Enterococcus spp.-commensal, probiotic and opportunistic pathogen. Microorganisms. https://doi.org/10.3390/microorganisms9091900
Gu X, Sim JXY, Lee WL et al (2022) Gut Ruminococcaceae levels at baseline correlate with risk of antibiotic-associated diarrhea. iScience 25:103644. https://doi.org/10.1016/j.isci.2021.103644
Konikoff T, Gophna U (2016) Oscillospira: a central, enigmatic component of the human gut microbiota. Trends Microbiol 24:523–524. https://doi.org/10.1016/j.tim.2016.02.015
Feng W, Liu J, Ao H et al (2020) Targeting gut microbiota for precision medicine: focusing on the efficacy and toxicity of drugs. Theranostics 10:11278–11301. https://doi.org/10.7150/thno.47289
Rodrigues VF, Elias-Oliveira J, Pereira IS et al (2022) Akkermansia muciniphila and gut immune system: a good friendship that attenuates inflammatory bowel disease, obesity, and diabetes. Front Immunol 13:934695. https://doi.org/10.3389/fimmu.2022.934695
Zhou K (2017) Strategies to promote abundance of Akkermansia muciniphila, an emerging probiotics in the gut, evidence from dietary intervention studies. J Funct Foods 33:194–201. https://doi.org/10.1016/j.jff.2017.03.045
Daniel N, Gewirtz AT, Chassaing B (2023) Akkermansia muciniphila counteracts the deleterious effects of dietary emulsifiers on microbiota and host metabolism. Gut. https://doi.org/10.1136/gutjnl-2021-326835
Wu Z, Xu Q, Gu S et al (2022) Akkermansia muciniphila ameliorates Clostridioides difficile infection in mice by modulating the intestinal microbiome and metabolites. Front Microbiol 13:841920. https://doi.org/10.3389/fmicb.2022.841920
Xiang XW, Wang R, Yao LW et al (2021) Anti-inflammatory effects of Mytilus coruscus polysaccharide on RAW264.7 cells and DSS-induced colitis in mice. Mar Drugs. https://doi.org/10.3390/md19080468
Hsiao YC, Lee YH, Ho CM et al (2021) Clinical characteristics of Actinomyces viscosus Bacteremia. Medicina (Kaunas). https://doi.org/10.3390/medicina57101064
Korf JM, Ganesh BP, McCullough LD (2022) Gut dysbiosis and age-related neurological diseases in females. Neurobiol Dis 168:105695. https://doi.org/10.1016/j.nbd.2022.105695
Holmes A, Finger C, Morales-Scheihing D et al (2020) Gut dysbiosis and age-related neurological diseases; an innovative approach for therapeutic interventions. Transl Res 226:39–56. https://doi.org/10.1016/j.trsl.2020.07.012
Buford TW (2017) (Dis)Trust your gut: the gut microbiome in age-related inflammation, health, and disease. Microbiome 5:80. https://doi.org/10.1186/s40168-017-0296-0
Koppie TM, Serio AM, Vickers AJ et al (2008) Age-adjusted Charlson comorbidity score is associated with treatment decisions and clinical outcomes for patients undergoing radical cystectomy for bladder cancer. Cancer 112:2384–2392. https://doi.org/10.1002/cncr.23462
Funding
This work was supported by the clinical project of the Shanghai Municipal Health Commission (No. 201940312) and Shanghai Municipal Key Clinical Specialty (Geriatrics, No. shslczdzk02802).
Author information
Authors and Affiliations
Contributions
YW, YW, and JR carried out the studies, participated in collecting data, and drafted the manuscript. YW, YZ, and JZ performed the statistical analysis and participated in its design. LZ and HQ participated in the acquisition, analysis, or interpretation of data and drafted the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no competing interests.
Ethical approval and consent to participate
This study was approved by the Clinical Research Ethics Committee of Huashan Hospital (KY2018-437). Informed consent was obtained from all subjects or, in cases of cognitive impairment, next of kin, in accordance with the Ethics Committee’s guidelines.
Statement of human and animal rights
All procedures performed in this study involving human participants were in accordance with the ethical standards of the institutional and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Consent for publication
Not applicable.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Zhao, L., Zhang, Y., Wang, Y. et al. Gut microbiota diversity of hospitalized older adult patients with and without antibiotic-associated diarrhea. Aging Clin Exp Res 35, 1541–1555 (2023). https://doi.org/10.1007/s40520-023-02436-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40520-023-02436-5