Abstract
Background
This study compares the performance at the Mini-Mental State Examination (MMSE) and Montreal Cognitive Assessment (MoCA) across the healthy adult lifespan in an Italian population sample.
Methods
The MMSE and MoCA were administered to 407 Italian healthy native-speakers (165 males; age range 20–93 years; education range 4–25 years). A generalized Negative Binomial mixed model was run to profile MMSE and MoCA scores across 8 different age classes (≤ 30; 31–40; 41–50; 51–60; 61–70; 71–80; 81–85; ≥ 86) net of education and sex.
Results
MMSE and MoCA total scores declined with age (p < 0.001), with the MoCA proving to be “more difficult” than the MMSE (p < 0.001). The Age*Test interaction (p < 0.001) indicates that the MoCA proved to profile a sufficiently linear involutional trend in cognition with advancing age and to be able to detect poorer cognitive performances in individuals aged ≥ 71 years. By contrast, MMSE scores failed in capturing the expected age-related trajectory, reaching a plateau in the aforementioned age classes.
Discussion
The MoCA seems to be more sensitive than the MMSE in detecting age-related physiological decline of cognitive functioning across the healthy adult lifespan. The MoCA might be therefore more useful than the MMSE as a test for general cognitive screening aims.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
There is an overall favor among European [1], and especially Italian [2], healthcare practitioners towards the relevance of screening for cognitive impairment in asymptomatic adults within primary care settings, due to its beneficial entailments in respect to a timely intervention.
However, less consensus has been reached as to which test is most suitable to this aim [3]: the Mini-Mental State Examination (MMSE), despite being the most widespread cognitive screening test worldwide, has been questioned as to its feasibility in primary care [4], as being heavily subjected to ceiling effects [5] and thus scarcely sensitive to sub-clinical deficits [6]. By contrast, the Montreal Cognitive Assessment (MoCA), as widespread as the MMSE, has been highlighted as more sensitive than specific [7], and thus appropriate to detect even subtle cognitive changes when screening putatively healthy individuals [8, 9].
According to the World Health Organization (WHO), for a general-population screening program to be implemented, “[…] there should be a suitable diagnostic test that is available […]”, as well as “an agreed policy, based on respectable test findings and national standards […]” (http://www.euro.who.int/document/E88698.pdf). Hence, within the framework of cognitive screening, a first step for such requirements to be met would be to provide country-specific data on the performance on the MMSE and MoCA across the healthy adult lifespan, in order to explore their capability at detecting age-related, physiological changes in cognitive functioning and thus their feasibility for general-population screening aims.
To date, such an investigation has been only performed by Gluhm et al. [4], who showed that, in healthy English adults aged from 20 to 89 years, the MoCA was superior to the MMSE in cross-sectionally profiling involutional cognitive trajectories across age decades. Given that in Italy such data have not been provided yet [10], this study aimed at comparing MMSE and MoCA scores across the healthy adult lifespan in a large Italian population sample. Specifically, within this work, it was postulated that, in line with the findings of Gluhm et al. [4], the MoCA would outperform the MMSE as to the capability of detecting age-related physiological decline of cognitive functioning across the healthy adult lifespan also in the Italian population, based on the notion of the MoCA being “more difficult” to execute, and thus coming with a greater sensitivity when compared to the MMSE [7,8,9].
Methods
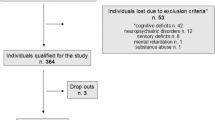
The sample consisted in 407 Italian native-speakers (165 males, 242 females), with a mean age of 60.61 ± 13.74 years (range 20–93 years) and a mean education of 12.2 ± 4.42 years (range 4–25 years), who were recruited from different regions of Northern Italy. Sample stratification is shown in Supplementary Table 1. Participants had no history of (1) neurological/psychiatric disorders, (2) active psychotropic medications, (3) uncompensated, severe metabolic/internal conditions, (4) organ/system failures and (5) un-corrected vision and hearing deficits.
Participants were sub-divided into the following 8 age classes: ≤ 30; 31–40; 41–50; 51–60; 61–70; 71–80; 81–85; ≥86.
The Italian MMSE [11] and MoCA [12] were administered to every participant in a randomized order. To control for ceiling effects and high inter-individual variability in test scores (skewness and kurtosis values ≥ |1| and |3|, respectively) [13], a Negative Binomial mixed model was performed, by addressing the raw number of errors as the outcome [14], in order to test the Age*Test interaction (between-subject factor: Age; within-subject factor: Test) net of Education and Sex. Subject was addressed as the cluster, within which only a random intercept was fitted.
Significance level was set at α = 0.05 and multiple comparisons were Bonferroni-corrected. Analyses were run via SPSS 27 (IBM Corp., 2021).
Results
The mean MMSE and MoCA scores for the whole sample were of 28.31±1.92 (range 20–30) and 25.62±3.84 (range 13–30), respectively. Error rates of participants on each test are shown separately for age classes in Table 1.
Both Age (F(7,796) = 8.52; p < 0.001) and Test (F(1,796) = 58.65; p < 0.001) main terms were significant, with error rates being overall higher on the MoCA when compared to the MMSE regardless of age, and linearly increasing on both tests with advancing age. As to covariates, Education was found to positively predict test scores (F(1,796) = 42.36; p < 0.001), whereas no Sex differences were detected (F(1,796) = 0.43; p = 0.514).
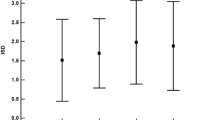
The Age*Test interaction (net of education and sex), displayed in Fig. 1, was also significant (F(7,796)=8.38; p < 0.001). Its post-hoc decomposition (Table 1) revealed that: (1) the error rate on the MMSE was lower than that on the MoCA in participants aged 41–50 and for those aged ≥ 61; (2) error rates on the MMSE were lower for participants aged 31–60 when compared to those 61–70; (3) error rates on the MoCA for participants aged ≤ 30 were lower when compared to all other age classes, as well as those of participants aged 31–70 when compared to those aged ≥ 71. No other significant differences were detected.
Due to the significant main effect of Education, a further, specular model was run to test the Education*Test interaction, which instead addressed raw Age values and recoded Education (namely, ≤ 5, 6–11, 12–16 and ≥ 17 years). Net of other main effects that remained the same, such an interaction was significant too, with the error rate on the MoCA being higher than that on the MMSE in all Education classes (p ≤ 0.028). However, no significant comparisons yielded as to both the MoCA and the MMSE error rates across Education classes.
Discussion
This study provides Italian clinicians and researchers with relevant information on the capability of the MMSE and MoCA in profiling age-related trends in cognitive functioning across the adult lifespan. Overall, the MoCA proved to be abler than the MMSE as to the detection of physiological cognitive changes with advancing age. Compliantly with WHO principles on general-population screening programs, the present Country-specific findings represent a first effort towards the identification of an adequate cognitive screening test to be administered to putatively normotypical, community-dwelling individuals. In this respect, consistently with the previous report by Gluhm et al. [4] in English healthy adults, the present results suggest that, at variance with the MMSE, the MoCA succeeds in capturing cognitive changes as a function of age, net of education and sex.
More specifically, the MoCA proved (1) to profile a sufficiently linear involutional trend in cognition with increasing age and (b) to be able to detect poorer cognitive performances in critical age classes, namely in individuals aged ≥ 71 years. By contrast, MMSE scores failed in capturing the expected age-related trajectory, but it also reaches a plateau in critical age classes. Notably, such a finding is in line with a recent Italian normative study on the MMSE [15] that showed that MMSE scores are overall similar, at a descriptive level, in healthy individuals aged from 70 to 94 years. It is thereupon reasonable to postulate that the MMSE would yield relatively low informativity as to age-related cognitive changes, and thus scarce utility for general-population screening aims, at variance with the MoCA.
In this last respect, it should be however noted that a recent meta-analysis by Nagaratnam et al. [16] suggests that the MMSE shows its highest capability in detecting cognitive decline among healthy individuals aged ≥ 84 years; however, this hypothesis cannot be confuted based on the present work since it includes a relatively small number of individuals falling under such an age range. Notably, Nagaratnam et al.’s [16] study also addressed ultra-centenary individuals, which were not represented in the present sample, despite their increase in number in the general population due to the overall higher life expectancy in Western countries. Future investigations should therefore focus MMSE performances in individuals in the eighth, ninth and tenth age decade.
This work also shows that, regardless of age, the MoCA is “more difficult” to execute than the MMSE, with such a discrepancy widening the most starting from the seventh age decade. This result is also supported by the fact that the error rates at the MoCA were systematically higher than that at the MMSE in all the education classes considered. Thereupon, findings herewith reported support the widespread notion [6] of the MoCA being more sensitive than the MMSE. Albeit such a feature is undoubtedly desirable for a screening test, it should be at the same time noted that the present data warn, in accordance with the literature [7], on the possibility that the MoCA may give rise to a higher false positive rates when compared to the MMSE. However, due to the absence of a third, independent gold-standard to explore the diagnostic accuracy of both tests, this work does not provide exhaustive information on the aforementioned possibility.
Besides those mentioned above, a number of further limitations should be finally listed: first, this study is cross-sectional, this limiting its external validity as to longitudinal inferences; second, age classes were partially inhomogeneous in size; third, the sample, although sufficiently well-stratified for age, education and sex, is region-specific.
In conclusion, the present work suggests that the MoCA is more sensitive than the MMSE in detecting age-related, physiological decline of cognitive functioning across the healthy adult lifespan in the Italian population. Such findings thus provide promising, albeit preliminary, evidence supporting the use of the MoCA, instead of the MMSE, as a test for general population-screening aims, in turn prompting future research aimed at confirming this hypothesis.
Data availability
Data analyzed within the present study are openly accessible at https://osf.io/8vr2s/.
References
Bond J, Graham N, Padovani A et al (2010) Screening for cognitive impairment, Alzheimer’s disease and other dementias: opinions of European caregivers, payors, physicians and the general public. J Nutr Health Aging 14:558–562
Bianchetti A, Ferrara N, Padovani A et al (2019) Timely detection of mild cognitive impairment in Italy: an expert opinion. J Alzheimer’s Dis 68:1401–1414
Tsoi KK, Chan JY, Hirai HW et al (2015) Cognitive tests to detect dementia: a systematic review and meta-analysis. JAMA Intern Med 175:1450–1458
Gluhm S, Goldstein J, Loc K et al (2013) Cognitive performance on the Mini-Mental State Examination and the Montreal Cognitive Assessment across the healthy adult lifespan. Cogn Behav Neurol 26:1–5
Franco-Marina F, García-González JJ, Wagner-Echeagaray F et al (2010) The Mini-mental State Examination revisited: ceiling and floor effects after score adjustment for educational level in an aging Mexican population. Int Psychogeriatr 22:72–81
Trzepacz PT, Hochstetler H, Wang S et al (2015) Relationship between the Montreal Cognitive Assessment and Mini-mental State Examination for assessment of mild cognitive impairment in older adults. BMC Geriatr 15:107
Larner AJ (2012) Screening utility of the Montreal Cognitive Assessment (MoCA): in place of–or as well as–the MMSE? Int Psychogeriatr 24:391–396
Ihle-Hansen H, Vigen T, Berge T et al (2017) Montreal Cognitive Assessment in a 63-to 65-year-old Norwegian cohort from the general population: data from the Akershus Cardiac Examination 1950 study. Dement Geriatr Cogn Disord 7:318–327
Krishnan K, Rossetti H, Hynan LS et al (2017) Changes in Montreal Cognitive Assessment scores over time. Assessment 24:772–777
Aiello EN, Rimoldi S, Bolognini N et al (2021) Psychometrics and diagnostics of Italian cognitive screening tests: a systematic review. Neurol Sci 43:821–845
Carpinelli Mazzi M, Iavarone A, Russo G et al (2020) Mini-Mental State Examination: new normative values on subjects in Southern Italy. Aging Clin Exp Res 32:699–702
Aiello EN, Gramegna C, Esposito A et al (2022) The Montreal Cognitive Assessment (MoCA): updated norms and psychometric insights into adaptive testing from healthy individuals in Northern Italy. Aging Clin Exp Res 34:375–382
Kim HY (2013) Statistical notes for clinical researchers: assessing normal distribution (2) using skewness and kurtosis. Restor Dent Endod 38:52–54
Aiello EN, Depaoli EG, Gallucci M (2020) Usability of the negative binomial model for analyzing ceiling and highly-inter-individually-variable cognitive data. Neurol Sci 41:S273–S274
Foderaro G, Isella V, Mazzone A et al (2022) Brand new norms for a good old test: Northern Italy normative study of MiniMental State Examination. Neurol Sci 43:3053–3063
Nagaratnam JM, Sharmin S, Diker A et al (2022) Trajectories of Mini-mental state examination scores over the lifespan in general populations: a systematic review and Meta-regression analysis. Clin Gerontol 45:467–476
Acknowledgement
None.
Funding
Open access funding provided by Università degli Studi di Milano - Bicocca within the CRUI-CARE Agreement. Research funded by the Italian Minsitry of Health to N.B.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no known conflicts of interest.
Ethical approval
The study received approval by the local Research Ethics Committees (University of Milano-Bicocca and University of Pavia) and conducted in accordance with the Declaration of Helsinki; participants provided informed consent.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Aiello, E.N., Pasotti, F., Appollonio, I. et al. Trajectories of MMSE and MoCA scores across the healthy adult lifespan in the Italian population. Aging Clin Exp Res 34, 2417–2420 (2022). https://doi.org/10.1007/s40520-022-02174-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40520-022-02174-0