Abstract
Background
The studies on the association of various midlife risk factors with reaching 90 years or more are scarce. We studied this association in a socioeconomically homogenous cohort of businessmen.
Methods
The study consists of men (n = 970) from the Helsinki Businessmen Study cohort (born 1919–1928). Five major cardiovascular disease (CVD) risk factors (smoking, BMI, blood pressure, serum lipids, fasting glucose), consumption of alcohol and coffee, self-rated health and self-rated fitness, were assessed in 1974, at an average age of 50 years. The number of major risk factors was tested as a risk burden. The Charlson Comorbidity Index and the RAND-36 (SF-36) Physical and Mental health summary scores were calculated from surveys in year 2000, at age of 73 years. Mortality dates were retrieved through 31 March 2018 from the Population Information System of Finland.
Results
244 men survived to the age of 90 representing 25.2% of the study cohort. The survivors had less risk factor burden in midlife, and less morbidity and higher physical health summary score in 2000. Of those with five major risk factors only 7% survived up to 90 years, whereas 51% of those without any risk factors reached that age. Single risk factors reducing odds of reaching 90 years were smoking (odds ratio [OR] 0.48, 95% confidence interval [CI] 0.34–0.67), glucose (0.66, 0.49–0.88), BMI (0.63, 0.46–0.86), and cholesterol (0.71, 0.53–0.96).
Conclusion
Lack of five major CVD risk factors in midlife strongly increased odds of reaching 90 years of age and also predicted factors related to successful ageing in late life.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Life expectancy has remarkably increased in Europe in the past decades [1]. Increasing numbers of people reach exceptional longevity, 90 years or more [1]. For example, in Finland the probability of a 50-year old man of reaching the age of 90 has increased from 12 to 20% in 44 years [2].
Earlier studies have revealed the multitude of factors associated with longevity [3,4,5,6,7,8,9,10,11]: genetic factors may explain approximately 25% of the variation of lifespan, while healthy lifestyle habits in midlife also play an important role [12].
For exceptional longevity, Yates et al. [13] studied the association of factors in age of 70 with survival till 90, and they revealed that the probability of reaching 90 years of age was 54% for those men who did not have any risk factors, and 4% for those who had five risk factors (smoking, diabetes, obesity, hypertension, sedentary lifestyle) at mean age of 72. In addition, a Swedish prospective study [14] among a heterogeneous cohort showed that non-smoking, socioeconomic status and general good health in midlife were strong predictors of survival to the age of 90.
To our knowledge, there are scarce prospective studies in homogeneous cohorts with very long follow-ups, especially exploring how combination of midlife major risk factors determines reaching 90 years of age. We investigated these midlife factors in a 44-year follow-up study of the Helsinki Businessmen Study cohort in which socioeconomic effects on longevity are inherently adjusted for. To reflect the quality of longer life, we also compared some factors related to “successful” ageing at the age of 73 years between those who did or did not reach 90 years of age.
Design and methods
Study population
HBS is a prospective cohort study of initially healthy Finnish businessmen and executives born between 1919 and 1934 (original n = 3490). Details of the study cohort have been described earlier [15]. The present study included those men who had the possibility to reach 90 years of age by March 2018 (born between 1919 and 1928) and had data of all major risk factors available in 1974 (n = 970). This sub-group has been followed-up for 44 years with mailed questionnaires, and clinical and laboratory assessments. The follow-up was approved by the Ethics Committee of the Helsinki University Hospital, Department of Medicine, and all participants had provided informed consents.
Baseline measurements
Midlife factors were assessed in 1974, at an average age of 50 years. Clinical and laboratory examinations included body mass index (BMI, kg/m2), systolic and diastolic blood pressure (mmHg), total serum cholesterol (mmol/L), triglycerides (mmol/L) and 1-h post-load glucose (mmol/L). In addition, the status of smoking and consumption of coffee (cups/day) and alcohol (g/week) were asked in a questionnaire. Major cardiovascular risk factors included smoking status (yes/no), systolic blood pressure (≥ 144 mmHg), total cholesterol (> 6.2), body mass index (> 25) and fasting glucose (≥ 4.7). Median was used as a cut-point for risk in continuous variables. The number of major risk factors was tested as a risk burden.
Self-rated health (SRH) and self-rated fitness (SRF) were assessed by asking “What do you think about your present state of health/fitness; is it “very good”, “fairly good”, “average”, “fairly poor” or “very poor”. The status as “very good” and “fairly good” were combined in analyses of SRH and SRF.
In 2000, men were sent a mailed questionnaire which included the survey of diseases and the validated Finnish version of the RAND-36 Health Survey [16]. The Charlson Comorbidity Index (CCI) was used as a measure of burden of disease [17]. The Physical and Mental health summary scores of the RAND-36 Health Survey were calculated and used in the analyses [18].
Mortality
The dates of death were drawn from the national Population Information System in March 2018. Between years 1974 and 2018, 830 men of this sub-cohort had died. Of the deceased persons, 104 had reached 90 years of age whereas 726 had died before the age of 90 (Fig. 1).
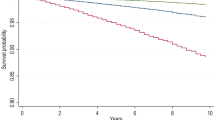
Statistical analyses
The descriptive statistics are presented as means with SDs or as counts with percentages. Statistical comparisons between the groups were made using the t test or Chi square test. In the case of violation of the assumptions (e.g., non-normality), a bootstrap-type test was used. Kaplan–Meier method with age is the time scale used to estimate the cumulative survival. To determine characteristics associated with reaching 90 years of age, multivariate logistic regression analysis was applied. The normality of the variables was tested using the Shapiro–Wilk W test. Stata 15.1 (StataCorp LP, College Station, TX, USA) was used for the analysis.
Results
The baseline characteristics of the study cohort in 1974 are shown in Table 1. The mean age was 50 years (range 46–55 years). 25.2% (n = 244) men of the cohort had reached 90 years or more by March 2018. Survivors to the age of 90 had less likely smoking history, and lower BMI than non-survivors. They had also lower levels of both systolic and diastolic blood pressure, fasting and 1-h glucose and serum lipids. They also consumed less alcohol. There were slight differences in midlife SRH and SRF between survivors to the age of 90 and non-survivors, but those were not significant.
In 2000, the Charlson comorbidity index was significantly lower for men who reached 90 years of age. In addition, the Physical health summary score in RAND-36 was significantly higher for those who survived till age of 90, but differences in the Mental health summary score were not significantly different.
Of those who had none of the major risk factors, 51% reached 90 years of age. With one major risk factor, the percentage was 33%, with two risk factors 30%, with three risk factors 20%, and with four risk factors 18%. Whereas of those with five major risk factors only 7% survived until 90. There was a linear relationship between the number of risk factors and reaching up to 90 years of age (Fig. 2).
In logistic regression analysis, significant risk factors were smoking (OR 0.48, 95% CI 0.34–0.67), glucose (OR 0.66, 95% CI 0.49–0.88), BMI (OR 0.63, 95% CI 0.46–0.86) and cholesterol (OR 0.71, 95% CI 0.53–0.96) whereas systolic blood pressure did not reach significance. Table 2.
Discussion
Our findings revealed that the burden of major cardiovascular risk factors is a linear and strong determinant of mortality and this burden efficiently prevents reaching 90 years of age. Of those having none of these major risk factors 51% survived until 90 years of age whereas among those with five risk factors only 7% reached that age. Smoking, higher BMI, and higher levels of glucose and cholesterol were significant predictors for mortality in logistic regression analysis and prevented survival to the age of 90. The survivors had significantly less chronic diseases at the mean age of 73 years, and their physical health summary score was also significantly higher than among non-survivors suggesting that the longer life span was not necessarily of poor quality.
Previous studies have reported that absence of various risk factors in midlife is associated with longer life expectancy [11, 14, 19,20,21]. Similar to our study, the burden of risk factors has been studied in the Framingham Heart Study cohort, but the study population was socioeconomically more diverse, and the educational level was also found to be associated with the survival to exceptional longevity [21]. Also, Yates et al. [13] have studied the cumulative effect of cardiovascular risk factors, and the results were similar to ours. However, the factors were measured at age 20 years older than in our cohort, and therefore the follow-up time was much shorter, 18 years. Yates et al. [13] found that the SRH was significantly higher at mean age of 72 among those who survived to the age of 90. However, there was no difference in SRH between those who did or did not reach 90 years in our study with a 44-year follow-up. This may be due to the fact that SRH has better prognostic value in shorter follow-ups when an individual has more accurate information about one’s condition [22].
The study of Wilhelmsen et al. [14] showed that high socioeconomic status and good functional capacity were associated with the survival to the age of 90 years [14]. In our study, the physical health summary score at mean age of 73 was higher among those businessmen who reached 90 years of age. Also, at the mean age of 73 those who did not survive up to that age had more disability and morbidity than survivors.
In midlife, the future survivors to 90 years of age had a significantly lower average systolic and diastolic blood pressure than non-survivors. However, in contrast to previous studies [13, 14, 20, 21], blood pressure was not an independent predictor of survival to the age of 90. This can be explained by correlation of blood pressure with BMI and smoking. Furthermore, antihypertensive treatments during follow-up may also have diluted potential differences.
The proportion of people who reach 90 years of age has increased over the past century [3]. During past decades the life expectancy has increased especially for the people who already have entered old age [3]. The concept of successful ageing has been generally associated with longevity, highlighting the importance of a very long, healthy and active life [3, 4]. The important aspect of this paradigm is ‘‘the compression of morbidity’’ explaining that disabilities and illnesses can be packed to a minimum period in later years and thus expand the healthy life span [3, 4]. Our results also support this theory. Prevention and advanced treatment of chronic diseases enable an individual to maintain functionality and age “successfully” [23,24,25,26,27,28,29,30,31,32]. Cardiovascular risk factors are well known, and their treatments have developed during past decades [33], although intensity of treatment varies between various risk factors despite effective treatments for, e.g., hypertension and dyslipidemia. The obesity epidemic, in turn, continues to lack effective treatments [33]. For aiming exceptional longevity, our results nevertheless highlight the cumulative effects of common risk factors, which should be taken account in practice and in health promotion interventions.
Longitudinal data on a combination of risk factors related to survival beyond 90 years have been limited. The strength of our study is the very long, 44-year follow-up of initially healthy men. Our study sample is also very homogeneous representing men from the upper social class which reduces confounding by socioeconomic factors. This is obviously also a limitation for the generalizability of the results. In addition, the cumulative CVD risk factors were only assessed at an average age of 50, and the quality of life and morbidity were only reported at an average age of 73 years. Furthermore, the analyses do not capture the variables of social context.
Implications
Our results show that the burden of midlife risk factors is associated with survival to advanced ages, and suggest that having a healthy lifestyle in midlife, especially avoiding smoking and obesity, may improve the probability of reaching exceptional longevity, 90 years or more. Therefore, the study gives important incentives for individuals and practitioners who wish to promote longevity.
References
Eurostat (2016) Available at https://ec.europa.eu/eurostat/. Accessed 2 Nov 2018
Statistics Finland (2017) Available at https://findikaattori.fi/fi/46. Accessed 2 Nov 2018
Newman AB, Murabito JM (2013) The epidemiology of longevity and exceptional survival. Epidemiol Rev 35:181–197. https://doi.org/10.1093/epirev/mxs013
Cosco TD, Prina AM, Perales J et al (2014) Operational definitions of successful aging: a systematic review. Int Psychogeriatr 26:373–381. https://doi.org/10.1017/S1041610213002287
Depp CA, Jeste DV (2006) Definitions and predictors of successful aging: a comprehensive review of larger quantitative studies. Am J Geriatr Psychiatry 14:6–20. https://doi.org/10.1097/01.JGP.0000192501.03069.bc
Fries JF (1980) Aging, natural death, and the compression of morbidity. N Engl J Med 303:130–135
Lafortune L, Martin S, Kelly S et al (2016) Behavioral risk factors in mid-life associated with successful aging, disability, dementia and frailty in later life: a rapid systematic review. PLoS One 11:1–34. https://doi.org/10.1371/journal.pone.0144405
Nosraty L, Jylhä M, Raittila T et al (2015) Perceptions by the oldest old of successful aging, Vitality 90 + Study. J Aging Stud 32:50–58. https://doi.org/10.1016/j.jaging.2015.01.002
Pruchno RA, Wilson-Genderson M (2013) A longitudinal examination of the effects of early influences and midlife characteristics on successful aging. J Gerontol B Psychol Sci Soc Sci 70:850–859. https://doi.org/10.1093/geronb/gbu046
Södergren M (2013) Lifestyle predictors of healthy aging in men. Maturitas 75:113–117. https://doi.org/10.1016/J.MATURITAS.2013.02.011
Clarke R, Emberson J, Fletcher A et al (2009) Life expectancy in relation to cardiovascular risk factors: 38 year follow-up of 19,000 men in Whitehall study. BMJ 16:b3513. https://doi.org/10.1136/bmj.b3513
Christensen K, Johnson TE, Vaupel JW (2006) The quest for genetic determinants of human longevity: challenges and insights. Nat Rev Genet 7:436–448
Yates LB, Djoussé L, Kurth T et al (2008) Exceptional longevity in men: modifiable factors associated with survival and function to age 90 years. Arch Intern Med 168:284–290
Wilhelmsen L, Svärdsudd K, Eriksson H et al (2010) Factors associated with reaching 90 years of age: a study of men born in 1913 in Gothenburg, Sweden. J Intern Med. https://doi.org/10.1111/j.1365-2796.2010.02331.x
Strandberg TE, Salomaa VV, Strandberg AY et al (2015) Cohort profile: the Helsinki Businessmen Study (HBS). Int J Epidemiol 45:1074. https://doi.org/10.1093/ije/dyv310
Aalto A-M, Aro AR, Teperi J (1991) RAND-36 as a measure of health-related quality of life: reliability, construct validity, and reference values in the Finnish general population. Helsinki, Finland: Stakes; Research Reports 101
Charlson ME, Pompei P, Ales KL et al (1987) A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis 40:373–383
Ware JE, Kosinski M (2001) SF-36 physical and mental health summary scales: a manual for users of version 1, 2nd edn. Quality Metric Inc., Lincoln
Licher S, Heshmatollah A, van der Willik KD et al (2019) Lifetime risk and multimorbidity of non-communicable diseases and disease-free life expectancy in the general population: a population-based cohort study. PLoS Med 16:e1002741. https://doi.org/10.1371/journal.pmed.1002741
Willcox BJ, He Q, Chen R et al (2006) Midlife risk factors and healthy survival in men. J Am Med Assoc 296:2343–2350
Terry DF, Pencina MJ, Vasan RS et al (2005) Cardiovascular risk factors predictive for survival and morbidity-free survival in the oldest-old Framingham Heart Study participants. J Am Geriatr Soc 53:1944–1950
Jylhä M (2009) What is self-rated health and why does it predict mortality? Towards a unified conceptual model. Soc Sci Med 69:307–316. https://doi.org/10.1016/j.socscimed.2009.05.013
Robinson SM, Jameson KA, Syddall HE et al (2013) Clustering of lifestyle risk factors and poor physical function in older adults: the Hertfordshire Cohort Study. J Am Geriatr Soc 61:1684–1691. https://doi.org/10.1111/jgs.12457
Lloyd-Jones DM, Larson MG, Beiser A et al (1999) Lifetime risk of developing coronary heart disease. Lancet 353:89–92
Strandberg AY, Strandberg TE, Pitkälä K et al (2008) The Effect of smoking in midlife on health-related quality of life in old age: a 26-year prospective study. Arch Intern Med 168:1968–1974. https://doi.org/10.1001/archinte.168.18.1968
Sabia S, Singh-Manoux A, Hagger-Johnson G et al (2012) Influence of individual and combined healthy behaviours on successful aging. Cancer Med Assoc J 18:1985–1992. https://doi.org/10.1503/cmaj.121080
Urtamo A, Huohvanainen E, Pitkälä KH et al (2019) Midlife predictors of active and healthy aging (AHA) among older businessmen. Aging Clin Exp Res 31:225. https://doi.org/10.1007/s40520-018-1100-0
Rantanen KK, Strandberg TE, Stenholm SS et al (2015) Clinical and laboratory characteristics of active and healthy aging (AHA) in octogenarian men. Aging Clin Exp Res 27:581–587. https://doi.org/10.1007/s40520-015-0329-0
Artaud F, Sabia S, Dugravot A et al (2016) Trajectories of unhealthy behaviors in midlife and risk of disability at older ages in the Whitehall II Cohort Study. J Gerontol A Biol Sci Med Sci 71:1500–1506. https://doi.org/10.1093/gerona/glw060
Grande G, Vetrano DL, Fratiglioni L et al (2019) Disability trajectories and mortality in older adults with different cognitive and physical profiles. Aging Clin Exp Res. https://doi.org/10.1007/s40520-019-01297-1
Strandberg TE, Strandberg AY, Salomaa VV et al (2007) The association between weight gain up to midlife, 30-year mortality, and quality of life in older men. Arch Intern Med 167:2260–2261
Stenholm S, Head J, Aalto V et al (2017) Body mass index as a predictor of healthy and disease-free life expectancy between ages 50 and 75: a multicohort study. Int J Obes (London) 41:769–775. https://doi.org/10.1038/ijo.2017.29
Flegal KM, Kit BK, Orpana H et al (2013) Association of all-cause mortality with overweight and obesity using standard body mass index categories: a systematic review and meta-analysis. J Am Med Assoc 309:71–82. https://doi.org/10.1001/jama.2012.113905
Acknowledgements
Open access funding provided by University of Helsinki including Helsinki University Central Hospital.
Funding
This study was supported by Helsinki University Hospital VTR (EVO), funding and Academy of Finland (311492).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors have no conflict of interest to report.
Statement of human and animal rights
The study has been approved by the ethical committee of the Department of Medicine, Helsinki University Hospital. The study is registered as ClinicalTrials.gov identifier: NCT02526082.
Informed consent
All participants had provided informed consents.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
About this article
Cite this article
Urtamo, A., Jyväkorpi, S.K., Kautiainen, H. et al. Major cardiovascular disease (CVD) risk factors in midlife and extreme longevity. Aging Clin Exp Res 32, 299–304 (2020). https://doi.org/10.1007/s40520-019-01364-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40520-019-01364-7