Abstract
Objectives
The present study explores the differences in gait parameters in elderly subjects with or without cognitive impairment measured by means of ambulatory actigraphy while performing a single and a dual task.
Methods
Sixty-nine participants of which 23 individuals were diagnosed with Alzheimer’s disease (AD), 24 individuals with mild cognitive impairment (MCI), and 22 healthy controls performed a single and dual walking task while wearing a wrist-worn accelerometer. Objective measures of gait features such as walking speed, cadence (i.e., number of steps per minute), and step variance (i.e., variance in time between two consecutive steps) were derived and analyzed.
Results
While differences in several gait parameters, namely walking speed, were found between MCI and AD patients, no differences between healthy elderly and MCI patients were found.
Conclusion
Walking speed seems to be a gait-related feature that differs significantly between MCI and AD patients and thus could be used as an additional measurement in clinical assessment. However, differences in gait may not be salient enough in the early stages of dementia to be detected by actigraphy. More research comparing different methods to measure gait in early stages of dementia under different dual task conditions is neccessary.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Alzheimer’s disease (AD) is the most common neurodegenerative disorder and one of the leading causes of death at old age [1, 2]. AD affects different domains of functioning, including cognitive and motor functioning [2, 3]. Motor functioning involves the integration of various cognitive functions including visuospatial perception, attention, and planning. Deficits in these cognitive functions can therefore affect motor functioning, and subtle changes in motor functioning could be an early indicator of cognitive decline [4]. Identifying patients in pre-dementia states, such as mild cognitive impairment (MCI), is an important clinical need since treatment may be more effective in early stages [1, 5]. This has led to an increase in research on early markers for cognitive decline, including motor markers [4]. The relation between motor activity and dementia has received increasing research attention over the past years [4, 6–24]. Studies have shown that compared to healthy elderly, AD patients walk more slowly and have an increased fall risk [9]. In addition, research has shown that gait disturbances can be observed in early AD and can predict progression from MCI to AD [7, 8, 11, 12, 20]. Research on gait disturbances as an early indicator for MCI and AD often uses the dual-task paradigm to explore the influence of cognitive functioning on motor functioning [4, 6, 15–19]. Dual tasking relies on dividing attention between two distinct tasks, often a motor task such as walking and a cognitively demanding task such as counting backwards. The dual-task paradigm can be used to study the allocation of attentional resources during a motor task and to separate the cognitive and motor components of executing a movement [4]. MCI and AD patients typically show more pronounced decrements in gait when performing two tasks simultaneously compared to healthy elderly [15, 16, 19]. Different cognitive tasks have been used for dual tasking including simple tasks such as counting backwards [6, 16], or more complex tasks such as a verbal fluency [6, 16] or reciting alternate letters of the alphabet [17]. Generally, increasing cognitive effort in the dual task increases sensitivity of the gait assessment but in older adults an attention-demanding arithmetic task such as counting backwards seems to be more appropriate for gait analyses [18].
Several studies have explored gait-related features such as speed of walking, stride frequency, and length and symmetry of steps in elderly with and without cognitive impairment during the performance of a single and a dual task [4, 6, 12, 15, 16, 18, 19]. In a study including 14 MCI patients, six AD patients, and 14 healthy control subjects, participants were asked to walk a distance of 45 m, while gait parameters were measured by means of two actigraphs attached at the participants’ waist [15]. AD patients were found to be slower than MCI patients who were found to be slower than healthy controls during the dual task involving walking and counting backwards. Additionally, MCI and mild AD patients showed deviations in other aspects of gait during the dual task compared to the single task, which were not found in healthy controls. Other studies that have only included MCI patients and not AD patients have found similar results [4, 6, 13, 16]. For instance, a study including 55 MCI patients found that participants walked significantly slower during a dual task than during a single task [6]. Similarly, a study measuring differences in in-home walking trajectories between 31 non-amnestic MCI patients and 54 healthy elderly found that individuals with non-amnestic MCI walked slower than healthy elderly [13]. Additionally, non-amnestic MCI patients showed a more pronounced decrease in walking speed variability over time than healthy controls whose walking speed variability remained stable. This finding suggests that walking speed and the variation in walking speed over time may be an early marker of MCI even at a state when memory functions are still intact [13]. Similarly, Beauchet et al. investigated stride velocity and stride-to-stride variability of stride time in 39 MCI patients, 33 AD patients, and 44 healthy elderly finding that both gait features increased during a dual-task condition compared to a single-task condition [12]. Moreover, stride-to-stride variability was found to be greater in MCI patients than in healthy elderly and AD patients in fast-pace walking suggesting that it is a specific feature of MCI under a fast-pace walking condition [12].
A possible explanation for the finding that individuals with cognitive decline show disturbances in their gait, particularly under dual-task conditions, is neuropathological changes in specific brain regions involved in the planning and execution of movements and that occur in early stages of dementia [2, 4, 21]. For instance, one study found a correlation between specific gait parameters (gait velocity, stride time variability) and the cerebral volume of the motor area as well as the presence of neurochemical changes in MCI patients during single and dual tasking [21].
Together, the findings of the studies described above suggest that changes in walking parameters, such as walking speed and variability in stride time, can be detected in early stages of cognitive decline and can therefore be a biomarker of MCI. Research has only recently started to look into ways to measure the link between cognitive and motor function and to more objectively detect subtle changes that could indicate MCI or progression from MCI to AD. Sensing technologies are used more and more to monitor and assess motor behavior in elderly people [25]. Most of the studies on gait in MCI and AD patients have employed pressure-point systems, such as GAITRite® System [4, 10–12, 17, 19, 21], or passive infrared sensors [13] which are not always affordable for all clinical sites. A more practical and low-cost solution for gait analysis is ambulatory actigraphy which consists of a piezoelectric accelerometer designed to record body movements. Actigraphy has previously been used in the assessment of various disorders including sleep–wake disorders, hyperactivity disorders, and dementia [22–24, 26–28]. The present study aims at exploring the relation between gait parameters, measured by means of ambulatory actigraphy during a single and dual task, and cognitive impairment in order to obtain more insights into the utility of such a paradigm as an additional indicator for the diagnosis of MCI and early AD.
Materials and methods
This study was conducted within the European project Dem@care which aims at developing a multiple sensor-based system to assess specific behaviors of people with dementia and to provide feedback to patients, caregivers, and clinicians.
Participants and procedure
Participants aged 65 years or older were recruited within the Dem@care protocol [29] at the Nice Memory Research Center located at the Geriatric Department of the University Hospital. The sample consisted of 24 individuals diagnosed with MCI, 23 individuals diagnosed with AD, and 22 healthy controls (HC). For the AD group, the diagnosis was determined using the proposed diagnostic criteria from Dubois et al. [30] requiring the presence of a progressive episodic memory impairment and biomarker evidence. For the MCI group, patients were diagnosed using the Petersen clinical criteria [31]. In addition, subjects were required to have a mini-mental state examination (MMSE) [32] score higher than 24. Subjects were not included if they had a history of head trauma with loss of consciousness, history of lower limb surgery, arthritis, obesity (BMI higher than 30), concomitant medication including benzodiazepines or antipsychotics, psychotic or aberrant motor activity (tremor, rigidity, Parkinsonism) as defined by the Movement Disorder Society Unified Parkinson Disease Rating Scale [33] in order to control for any possible motor disorders influencing the ability to carry out a walking task. The study was approved by the local ethics committee of the geriatric hospital in Nice, and only participants with the capacity to consent to the study were included. Each participant gave informed consent prior to the study. The consent was only given to publish demographic and accelerometer data but no biomarker data.
Assessments and clinical protocol
All participants performed a single walking task (ST) that consisted of walking 10 m, turning around and walking 10 m backwards. Subsequently, all participants performed a dual task (DT) that involved walking the same distance while counting backwards from 305 in steps of 1. All participants performed the tasks in the same corridor in the Memory clinic, which is approximately 10 m long and 2 m wide. The corridor had normal daylight and a stable room temperature of 25 °C. During both tasks, participants wore a wrist-worn accelerometer from which objective measures for walking speed, cadence (i.e., number of steps per minute), and step variance (i.e., variance in time between two consecutive steps) were derived. The accelerometer data were analyzed by determining segments of walking data from the raw signal, and by applying step detection using a step detection algorithm that selects steps based on peaks in the accelerometer magnitude signal using a set of heuristics related to the time between consecutive steps and the amplitudes of the signal peaks. Neuropsychological measures included the MMSE [31], frontal assessment battery (FAB) [34], and trail making test (TMT) A and B [35].
Motion data acquisition and analysis
Gait was measured using a CE-marked accelerometer research prototype (developed by Philips Research Laboratories Europe), a wrist-worn device containing a 3D accelerometer and data storage capabilities. The accelerometer was worn by the participants for the duration of the trial, after which the actigraphy data were retrieved from the device by the experimenter. During the trial, the experimenter indicated the start and end of both the ST and DT condition by pressing an event button on the accelerometer, creating an annotation on the device such that actigraphy data from both tasks could be easily extracted from the recording.
After extracting the actigraphy data, each recording was linked to the participant through a participant ID, and the actigraphy data for the individual ST and DT were extracted using the event markers recorded by the device. The actigraphy data for the tasks were then further cleaned by removing any initial and trailing periods of inactivity, caused by, e.g. the delay between the creation of the event marker and the commencement of the actual task.
Gait features were then determined algorithmically, using a heuristics-based step detection algorithm. The algorithm involves cleaning the accelerometer signal with a bandpass filter, finding a number of peaks in the filtered signal as potential steps, and creating a selection of the detected peaks which optimize a set of heuristic rules regarding the peak amplitude and distance to other peaks. From the detected steps, cadence was derived as the number of steps per minute, and step variance as the variance of the time between successive steps. Walking speed was derived as the distance traveled, divided by the time between the first and last step. Walking speed was derived as the distance traveled, divided by the time between the first and last step. A more detailed explanation of the algorithm and its performance on a previous dataset can be found in [36].
Statistical analysis
Statistical analysis was performed using SPSS 23. Analyses included Chi-square test, one-way analysis of variance (ANOVA), mixed between-within subjects ANOVA, and correlation analyses. Post hoc tests were performed with Bonferroni correction.
Results
Demographics and clinical assessments
The study included a total of 69 participants of which 23 individuals were diagnosed with AD (mean age = 77 years ± 9, MMSE = 17 ± 4.6), 24 individuals were diagnosed with MCI (mean age = 75 ± 9, MMSE = 24.8 ± 3.2), and 22 were healthy controls (mean age = 73 ± 7, MMSE = 28.4 ± 1.5). Demographic information and neuropsychological test results for the three groups are presented in Table 1.
There was no significant difference between the three groups in gender [χ²(2, 67) = 3.63, p = .163] or age [F(2, 66) = 1.63, p = .204]. Information about the MMSE was available for 67 participants. As expected, individuals diagnosed with AD had a lower MMSE [N = 23, mean = 17 (± 4.62)] than individuals diagnosed with MCI and HC, and individuals diagnosed with MCI [N = 24, mean = 24.75 (± 3.18)] had a lower MMSE than HC [N = 20, mean = 28.35 (± 1.5)]. All differences were statistically significant [F(2,66) = 63.23, p < .0001]. Information about the different subscales of the MMSE [24] was available for 47 participants.Footnote 1 As shown in Table 2, the differences between the HC and MCI are rather small and the differences between the HC and AD seem to be particularly pronounced in the temporal, attention and calculation, and recall subscores. A one-way ANOVA revealed significant differences for all subscalesFootnote 2 (orientation in time: F(2,46) = 24.47, p < .0001; orientation in place: F(2,46) = 22.1, p < .0001; registration: F(2,46) = 4.17, p = .022; attention and calculation: F(2,46) = 11.56, p < .0001; recall: F(2,46) = 23.52, p < .0001; language: F(2,46) = 9.24, p < .0001; and complex commands: F(2,45) = 7.25, p = .002). Post hoc tests revealed a significant difference between HC and AD (p < .0001) and MCI and AD (p < .0001) for the orientation in time subtest, between the HC and AD (p < .0001) and MCI and AD (p < .0001) for the orientation in place subtest, between MCI and AD (p = .033) for the registration subtest, between HC and AD (p < .0001) and MCI and AD (p = .008) for the attention and calculation subtest, between HC and MCI (p = .001), between HC and AD (p < .0001) and between MCI and AD (p = .003) for the recall subtest, between HC and AD (p = .002) and MCI and AD (p = .002) for the language subtest, and between HC and AD (p = .013) and MCI and AD (p = .003) for the complex commands subtest (Table 3).
Information about the FAB was available for 55 participants. Post hoc tests showed that participants diagnosed with AD [N = 18, mean = 10.89 (± 3.94)] had significantly lower scores on the FAB than individuals diagnosed with MCI [N = 20, mean = 15.1 (± 1.74), F(2,54) = 18.32, p < .0001] and HC [N = 17, mean = 15.94 (± 1.78), F(2,54) = 18.32, p < .0001].
Information about the TMT was available for 46 participants for version A and for 39 participants for version B. Information about the TMT A was available for 15 AD patients of whom three took so long that they were not asked to perform version B and who were therefore excluded from the analyses. When excluding these three patients, there was no difference between the three groups in time needed to perform version A of the TMT (F(2,42) = 2.58, p = .088). A one-way ANOVA did, however, find a difference between groups for the TMT B [F(2,37) = 12.22, p < .0001]. Post hoc tests revealed that AD patients [N = 7, mean = 279.29 s, (± 64.05 s)] needed significantly longer to complete the TMT B than both MCI patients [N = 15, mean = 171.73 s, (± 94.78 s), p = .007] and HC [N = 16, mean = 118 s, (± 45.7 s), p < .0001].
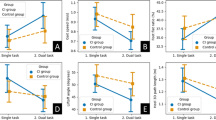
All participants were slower during the DT than during the ST (see Fig. 1). Interestingly, there seems to be a steeper increase in duration (i.e., a decrease in walking speed) from HC to MCI than from MCI to AD for both the ST and the DT. A mixed between-within ANOVA found a significant main effect for walking speed (Wilks’s Lambda = 0.76, F(1,66) = 20.89, p < .0001, partial eta squared = 0.24) with all groups showing a difference in walking speed between the ST and the DT. The difference between groups was significant [F(1,66) = 4.24, p = .019, partial eta squared = 0.114]. Post-hoc tests revealed that the difference in walking speed between the ST and DT differed between the HC [22.62 (± 3.03) vs. 26.46 (± 6.42)] and the AD group [26.34 (± 5.74) vs. 31.91 (± 7.79), p = .026] with the increase in duration (i.e., the decrease in walking speed) from the ST to the DT being greater for the AD patients. Although the increase in duration (i.e., the decrease in walking speed) from ST to DT was also greater for MCI [25.88 (± 7.7) vs. 30.95 (± 10)] patients than for HC, the difference between these two groups failed to reach significance (p = .072). No correlations were found between DT duration and neuropsychological measures of aspects of attention such as the MMSE subscale attention and calculation (r =−.19) and the TMT B (r = .294) or measures of motor performance such as the MMSE subscale complex commands (r =−.029).
All participants had a lower cadence during the DT than the ST (see Fig. 2). The difference in cadence between the ST and the DT is more pronounced for the MCI and AD patients than for the HC. A mixed between-within ANOVA found a significant main effect for cadence [Wilks’s Lambda = 0.57, F(1,66) = 50.28, p < .0001, partial eta squared = 0.432] with all groups showing a difference in cadence between the ST and the DT. The difference between groups did not reach statistical significance [F(2,66) = 2.89, p = .062, partial eta squared = 0.081]. No or low correlations were found between DT cadence and neuropsychological measures of aspects of attention such as the MMSE subscale attention and calculation (r = .125) and the TMT B (r = −326) or measures of motor performance such as the MMSE subscale complex commands (r = .037).
HC seem to have a smaller step variance and difference in step variance between ST and DT than MCI and AD patients (see Fig. 3). A mixed between-within ANOVA did, however, not find a significant main effect for step variance [Wilks’s Lambda = 0.97, F(1,65) = 1.73, p = .193, partial eta squared = 0.026]. There was a significant difference between groups [F(2,65) = 4.2, p = .019, partial eta squared = 0.115]. Post hoc tests revealed that the difference in step variance between the ST and DT differed between the HC [0.044 (± 0.05) vs. 0.039 (± 0.054)] and the AD group [0.067 (± 0.07) vs. 0.102 (± 0.099), p = .015] with the increase in step variance from the ST to the DT being greater for the AD patients. No or low correlations were found between DT step variance and neuropsychological measures of aspects of attention such as the MMSE subscale attention and calculation (r = −.211) and the TMT B (r = .348) or measures of motor performance such as the MMSE subscale complex commands (r = −.061).
Discussion
The findings of this study add to the growing body of research on the interaction between cognitive function and motor performance and show that there are changes in gait parameters that may help distinguish healthy elderly from elderly with cognitive impairment. These changes were detectable with an actigraph which seems to be a useful tool combined with the dual-task paradigm for gait assessment in clinical practice. As mentioned previously, actigraphy has already been proven to be of interest for the evaluation of behavioral symptoms in dementia patients such as apathy [22] or agitation [23]. For example, recently, Valembois et al. investigated the value of wrist actigraphy as a measure of disorder in motor behavior in 183 elderly people with dementia finding that motor activity levels can distinguish dementia patients with apathy and dementia patients with aberrant motor behavior [24]. We were interested in the effect of performing a dual task on gait parameters given that dual tasking represents a cognitive challenge since it requests the allocation of attentional resources to concomitant tasks. Although we found differences between the single and dual tasks as well as between healthy elderly and AD patients, we only found significant differences between patient groups for walking speed and not for cadence and step variance. It seems that changes in gait induced by simultaneously performing a cognitive task between healthy elderly and individuals with MCI are so subtle that they are difficult to measure with an actigraph. The changes may become more salient and, thus easier to detect when patients progress to more severe stages of the disease. This is in line with previous findings. Schwenk et al. state in their review on gait parameters for frailty in elderly that gait speed showed the highest effect size to discriminate between different frailty status groups which suggests that this parameter is particularly informative and plays a significant role in gait analysis in elderly [37].
Although significant dual-task decrements have been demonstrated in AD [8, 10, 14], studies on the effects of dual tasking in MCI have not yield conclusive results. For instance, while Maquet et al. found reduced stride frequency and walking speed in MCI patients compared to healthy control subjects [15], Muir et al. did not find any gait differences between MCI patients and healthy control subjects [38]. These inconclusive results may be caused by several factors. First, the distance participants are asked to walk and the cognitive task they are asked to perform during dual tasking differ between studies. The Muir et al. study demonstrated that the dual task costs for two different cognitive tasks, i.e., naming animals and serial subtractions of seven, were comparable between AD and MCI patients. Nevertheless, it is possible that in the present study the cognitive task was too easy for participants with MCI and future research would benefit from using various cognitive tasks with variable difficulty levels. Second, the measure used to assess gait parameters as well as the algorithms used to analyze these parameters differ between studies. When it comes to actigraphy, the position of the placed accelerometer can have an important impact on reliability and quality of the measurement. As mentioned above, research has shown that a wrist-worn accelerometer can reliably distinguish between dementia patients with apathy and aberrant motor behavior and dementia patients who do not show these neuropsychiatric symptoms [24]. However, to measure gait parameters, more accurate measurements may be obtained when attaching the accelerometer to the participant’s waist, which was the case in the study of Maquet et al. Consequently, it is possible that the accelerometer on the participants’ wrist did not pick up subtle changes in gait parameters and is therefore not sensitive enough for the specific purpose of measuring gait during the performance of a dual task. An important limitation of our study is therefore the use of a wrist-worn accelerometer. A third explanation is that gait impairments in MCI patients are too small to detect with actigraphy and that the dual-task paradigm is not sensitive enough for early MCI screening [8, 16] but rather for more advanced stages [37]. As described above, changes may become more salient and, thus easier to detect when patients progress to more severe stages of the disease. It is interesting to mention in this regard that there was a higher variation in walking speed in the MCI group than in the HC and AD groups which can be explained by heterogeneity of the MCI group. It may therefore be valuable to make a better distinction within the MCI group, e.g., between non-amnestic and amnestic MCI patients, in future research. Related to this issue is the fact that many studies on dual tasking, including the present study, have a rather small sample size which may not explain finding significant differences in gait parameters between MCI patients and healthy elderly. Additionally, some of the participants may have suffered from vascular pathology for which it was difficult to control but which may explain the changes detected in the data.
Even though we did not find significant differences in dual tasking between HC and MCI patients, we believe that the findings of the present study warrant more research on the interaction between cognitive function and motor performance as an early indicator of cognitive decline. Future research would benefit from using a waist-worn rather than a wrist-worn accelerometer. Furthermore, we believe that future research would benefit from comparing a body-worn actigraph with other technologies used for gait analyses. As recently stated in the review by Schwenk et al., no standardized “sensitive technology exists for use within routine clinical care that would objectively quantify relevant gait parameters for indicating frailty status” [37]. As stated above, a more practical and low-cost solution for gait analysis would be very valuable for clinical practice. In addition, interesting topics for further research on the link between motor function and cognitive function in elderly with cognitive impairment include the relation between dual-task performance and an individual’s ability to carry out activities of daily living as a measure with higher ecologic validity. Moreover, it would be interesting to further explore the value of using wrist-worn accelerometers in a non-controlled environment to provide continuous information about subtle changes in walking parameters that could be useful to monitor progression of cognitive decline. In non-controlled environments, wrist-worn accelerometers may be preferred as they are more practical and less stigmatizing.
Notes
Information about the MMSE complex commands subscale was only available for 46 participants.
When applying Bonferroni correction in order to account for multiple comparisons, the difference between groups for the registration subscale is no longer significant (for an alpha of 0.007).
References
Scarpini E, Scheltens P, Feldman H (2003) Treatment of Alzheimer’s disease: current status and new perspectives. Lancet Neurol 2:539–547
Nestor PJ, Scheltens P, Hodges JR (2004) Advances in the early detection of Alzheimer’s disease. Nature Rev Neurosci 10:S34–S41
Perry RJ, Hodges JR (1999) Attention and executive deficits in Alzheimer’s disease: a critical review. Brain 122:383–404
Montero-Odasso M, Oteng-Amoako A, Speechley M, Gopaul K, Beauchet O, Annweiler C, Muir-Hunter SW (2014) The motor signature of mild cognitive impairment: results from the gait and brain study. J Gerontol A Biol Sci Med Sci 69:1415–1421
DeCarli C (2003) Mild cognitive impairment: prevalence, prognosis, aetiology, and treatment. Lancet Neurol 2:15–21
Montero-Odasso M, Bergman H, Phillips NA, Wong CH, Sourial N, Chertkow H (2009) Dual-tasking and gait in people with mild cognitive impairment. The effect of working memory. BMC Geriatr 9:41
Aggarwal NT, Wilson RS, Beck TL, Bienias JL, Bennett DA (2006) Motor dysfunction in mild cognitive impairment and the risk of incident Alzheimer disease. Arch Neurol 63:1763–1769
Pettersson AF, Olsson E, Wahlund LO, (2005) Motor function in subjects with mild cognitive impairment and early Alzheimer’s disease. Dement Geriatr Cogn Disord 19:299–304
Alexander NB, Mollo JM, Giordani B, Ashton-Miller JA, Schultz AB, Grunawalt JA, Foster NL (1995) Maintenance of balance, gait patterns, and obstacle clearance in Alzheimer’s disease. Neurology 45:908–914
Allali G, Kressig RW, Assal F, Herrmann FR, Dubost V, Beauchet O (2007) Changes in gait while backward counting in demented older adults with frontal lobe dysfunction. Gait Posture 26:572–576
Verghese J, Robbins M, Holtzer R, Zimmerman M, Wang C, Xue X, Lipton RB (2008) Gait dysfunction in mild cognitive impairment syndromes. J Am Geriatr Soc 56:1244–1251
Beauchet O, Allali G, Launay C, Herrmann FR, Annweiler C (2013) Gait variability at fast-pace walking speed: a biomarker of mild cognitive impairment? J Nutr Health Aging 17:235–239
Dodge HH, Mattek NC, Austin D, Hayes TL, Kaye JA (2012) In-home walking speeds and variability trajectories associated with mild cognitive impairment. Neurology 78:1946–1952
Hauer K, Pfisterer M, Weber C, Wezler N, Kliegel M, Oster P (2003) Cognitive impairment decreases postural control during dual tasks in geriatric patients with a history of severe falls. J Am Geriatr Soc 51:1638–1644
Maquet D, Lekeu F, Warzee E, Gillain S, Wojtasik V, Salmon E, Petermans J, Croisier JL (2010) Gait analysis in elderly adult patients with mild cognitive impairment and patients with mild Alzheimer’s disease: simple versus dual task: a preliminary report. Clin Physiol Funct Imaging 30:51–56
Nascimbeni A, Caruso S, Salatino A, Carenza M, Rigano M, Raviolo A, Ricci R (2015) Dual task-related gait changes in patients with mild cognitive impairment. Funct Neurol 30:59–65
Verghese J, Buschke H, Viola L, Katz M, Hall C, Kuslansky G, Lipton R (2002) Validity of divided attention tasks in predicting falls in older individuals: a preliminary study. J Am Geriatr Soc 50:1572–1576
Beauchet O, Dubost V, Aminian K, Gonthier R, Kressig RW (2005) Dual-task-related gait changes in the elderly: does the type of cognitive task matter? J Mot Behav 37:459–464
Beauchet O, Freiberger E, Annweiler C, Kressig RW, Herrmann FR, Allali G (2011) Test–retest reliability of stride time variability while dual tasking in healthy and demented adults with frontotemporal degeneration. J Neuroeng Rehabil 8:37
Waite LM, Grayson DA, Piquet O, Creasey H, Bennett HP, Broe GA (2005) Gait slowing as a predictor of incident dementia: 6-year longitudinal data from Sydney older persons study. J Neurol Sci 229–230:89–93
Annweiler, C, Beauchet O, Bartha R, Wells JL, Borrie MJ, Hachinski V, Montero-Odasso M (2013) Motor cortex and gait in mild cognitive impairment: a magnetic resonance spectroscopy and volumetric imaging study. Brain 136:859–871.
David R, Mulin E, Friedman L, Le Duff F, Cygankiewicz E, Deschaux O, Garcia R, Yesavage JA, Robert PH, Zeitzer JM (2012) Decreased daytime motor activity associated with apathy in Alzheimer disease: an actigraphic study. Am J Geriatr Psychiatry 20:806–814
Mahlberg R, Walther S (2007) Actigraphy in agitated patients with dementia. Monitoring treatment outcomes. Z Gerontol Geriatr 40:178–184
Valembois L, Oasi C, Pariel S, Jarzebowski W, Lafuente-Lafuente C, Belmin J (2015) Wrist actigraphy: a simple way to record motor activity in elderly patients with dementia and apathy or aberrant motor behavior. J Nutr Health Aging 19:759–764
Patel S, Hyung P, Bonato P, Leighton C, Rogers M (2012) A review of wearable sensors and systems with application in rehabilitation. J Neuroeng Rehabil 9:21
Hatfield CF, Herbert J, van Someren EJ, Hodges JR, Hastings MH (2004) Disrupted daily activity/rest cycles in relation to daily cortisol rhythms of home-dwelling patients with early Alzheimer’s dementia. Brain 127:1061–1074.
Dane AV, Schachar RJ, Tannock R (2000) Does actigraphy differentiate ADHD subtypes in a clinical research setting? J Am Acad Child Adolesc Psychiatry 39:752–760
Deak M (2009) Use of actigraphy in neurological patient populations. Neurol Bull 1:17–23
König A, Crispim Jr C, Covella AGU, Bremond F, Derreumaux A, Bensadoun G, David R, Verhey F, Aalten P, Robert P (2015) Ecological assessment of autonomy in instrumental activities of daily living in dementia patients by the means of an automatic video monitoring system. Front Aging Neurosci 7:98
Dubois B, Feldman HH, Jacova C, Hampel H, Molinuevo JL, Blennow K, DeKosky ST, Gauthier S, Selkoe D, Bateman R, Cappa S, Crutch S, Engelborghs S, Frisoni GB, Fox NC, Galasko D, Habert MO, Jicha GA, Nordberg A, Pasquier F, Rabinovici G, Robert P, Rowe C, Salloway S, Sarazin M, Epelbaum S, de Souza LC, Vellas B, Visser PJ, Schneider L, Stern Y, Scheltens P, Cummings JL (2014) Advancing research diagnostic criteria for Alzheimer’s disease: the IWG-2 criteria. Lancet Neurol 13:614–629
Petersen RC, Smith GE, Waring SC, Ivnik RJ, Tangalos EG, Kokmen E (1999) Mild cognitive impairment: clinical characterization and outcome. Arch Neurol 56:303–308
Folstein M, Folstein SE, McHugh PR (1975) “Mini-Mental State”: a practical method for grading the cognitive state of patients for the clinician. J Psychiatr Res 121:189–198
Fahn S, Elton RL (1987) UPDRS program members. Unified Parkinson’s disease rating scale. In: Fahn S, Goldstein M, Calne DB (eds) Recent developments in Parkinson’s disease, M.C, Florham Park, pp 153–163
Dubois B, Slachevsky A, Litvan I, Pillon B (2000) The FAB: a frontal assessment battery at bedside. Neurology 55:1621–1626
AITB, Army Individual Test Battery (1944) Manual of directions and scoring, Adjutant General’s Office, Washington DC
Pijl MJ (2016) Tracking of human motion over time. Doctoral dissertation, Tilburg University
Schwenk M, Howe C, Saleh A, Mohler J, Grewal G, Armstrong D, Najafia B (2014) Frailty and technology: a systematic review of gait analysis in those with frailty. Gerontology 60:79–89
Muir SW, Speechley M, Wells J, Borrie M, Gopaul K, Montero-Odasso M (2012) Gait assessment in mild cognitive impairment and Alzheimer’s disease: the effect of dual-task challenges across the cognitive spectrum. Gait Posture 35:96–100
Acknowledgements
This study was supported by grants from the FP7 Dem@care project (Grant 288199), and by the Innovation Alzheimer association. The study was realized at the Cimiez hospital CIU-S platform and at the Institut Claude Pompidou, research center Edmond & Lily Safra.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
None declared.
Ethical approval
The study was approved by the local ethics committee of the geriatric hospital in Nice, and only participants with the capacity to consent to the study were included.
Informed consent
Each participant gave informed consent prior to the study.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
About this article
Cite this article
König, A., Klaming, L., Pijl, M. et al. Objective measurement of gait parameters in healthy and cognitively impaired elderly using the dual-task paradigm. Aging Clin Exp Res 29, 1181–1189 (2017). https://doi.org/10.1007/s40520-016-0703-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40520-016-0703-6