Abstract
Summary
The patients’ adherence to osteoporosis treatments is low. In our study population a history of osteoporotic fractures was associated to better compliance and persistence; however, a 12-month randomized study carried out on 816 osteoporotic women showed that providing the patients with their individual fracture risk information did not prove effective.
Purpose
Several drugs are currently available for the treatment of osteoporosis, but the patients’ compliance and persistence with these treatments are low. This study aimed to both analyze the adherence to oral osteoporosis medications among Italian osteoporotic patients (cross-sectional study) and evaluate if providing patients with their individual fracture risk information may improve compliance and persistence (prospective study).
Methods
A total of 3379 osteoporotic patients referred as outpatients for a visit 1 year after receiving a prescription of oral osteoporosis medications for the first time, were enrolled for the retrospective study. Moreover, 816 postmenopausal women receiving an oral prescription for osteoporosis for the first time, were randomized into two groups: group 1 (managed according to standard clinical practice) and group 2 (managed with greater patient involvement and information on the individual risk of major osteoporotic fractures calculated by DeFRA algorithm).
Results
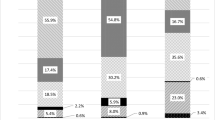
In the retrospective study, a history of osteoporotic fractures, the frequency of drug administration and a condition of being overweight/obese had a significant influence on both compliance and persistence. Of the 816 patients enrolled in the longitudinal study, 731 (374 of group 1 and 357 of group 2) attended the 1 year follow-up visit. The percentage of women with high compliance or persistence was greater in group 2 (64.2 vs. 58.1 % and 66.8 vs. 62.6 %, respectively), but without reaching any statistical significance.
Conclusions
Although providing the patients with their individual fracture risk information was not statistically effective, further studies on additional interventions able to improve the patients’ perceived risk of fracture are warranted.

Similar content being viewed by others
References
NIH consensus (2001) Development panel on osteoporosis prevention diagnosis and therapy. JAMA 285:785–795
Cooper C, Atkinson EJ, O’Fallon WM et al (1992) Incidence of clinically diagnosed vertebral fractures: a population-based study in Rochester, Minnesota, 1985–1989. J Bone Miner Res 7:221–227
Sanders KM, Nicholson GC, Ugoni AM et al (1999) Health burden of hip and other fractures in Australia beyond 2000. Projections based on the Geelong Osteoporosis Study. Med J Aust 170:467–470
Cummings SR, Melton LJ III (2002) Epidemiology and outcomes of osteoporotic fractures. Lancet 359:1761–1777
Johnell O, Kanis JA (2004) An estimate of the worldwide prevalence, mortality and disability associated with hip fracture. Osteoporos Int 15:897–902
Hernlund E, Svedbom A, Ivergård M et al (2013) Osteoporosis in the European Union: medical management, epidemiology and economic burden. A report prepared in collaboration with the International Osteoporosis Foundation (IOF) and the European Federation of Pharmaceutical Industry Associations (EFPIA). Arch Osteoporos 8:136
Kanis JA, McCloskey EV, Johansson H (2013) Scientific Advisory Board of the European Society for Clinical and Economic Aspects of Osteoporosis and Osteoarthritis (ESCEO) and the Committee of Scientific Advisors of the International Osteoporosis Foundation (IOF). European guidance for the diagnosis and management of osteoporosis in postmenopausal women. Osteoporos Int 24:23–57
Kothawala P, Badamgarav E, Ryu S et al (2007) Systematic review and meta-analysis of real-world adherence to drug therapy for osteoporosis. Mayo Clin Proc 82:1450–1493
Seeman E (2007) Unmet needs in fracture prevention: new European guidelines for the investigation and registration of therapeutic agents. Osteoporos Int 18:569–573
Hiligsmann M, Salas M, Hughes DA et al (2013) Interventions to improve osteoporosis medication adherence and persistence: a systematic review and literature appraisal by the ISPOR Medication Adherence and Persistence Special Interest Group. Osteoporos Int 24:2907–2918
Patrick AR, Brookhart MA, Losina E et al (2010) The complex relation between bisphosphonate adherence and fracture reduction. J Clin Endocrinol Metab 95:3251–3259
Silverman SL, Schousboe JT, Gold DT (2011) Oral bisphosphonate compliance and persistence: a matter of choice? Osteoporos Int 22:21–26
Rabenda V, Mertens R, Fabri V et al (2008) Adherence to bisphosphonates therapy and hip fracture risk in osteoporotic women. Osteoporos Int 19:811–818
Caro JJ, Ishak KJ, Huybrechts KF et al (2004) The impact of compliance with osteoporosis therapy on fracture rates in actual practice. Osteoporos Int 15:1003–1008
Haynes RB, Ackloo E, Sahota N et al (2008) Interventions for enhancing medication adherence. Cochrane Database Syst Rev 16:000011. doi:10.1002/14651858
Schousboe JT, Davison ML, Dowd B et al (2011) Predictors of patients’ perceived need for medication to prevent fracture. Med Care 49:273–280
Vytrisalova M, Touskova T, Ladova K et al (2015) Adherence to oral bisphosphonates: 30 more minutes in dosing instructions matter. Climacteric 24:1–9
Kanis JA, Johnell O, Oden A et al (2008) FRAX and the assessment of fracture probability in men and women from the UK. Osteoporos Int 19:385–397
Adami S, Bianchi G, Brandi ML et al (2010) Validation and further development of the WHO 10-year fracture risk assessment tool in Italian postmenopausal women: project rationale and description. Clin Exp Rheumatol 28:561–570
Morisky DE, Green LW, Levine DM (1986) Concurrent and predictive validity of a self-reported measure of medication adherence. Med Care 24:67–74
Shalansky SJ, Levy AR, Ignaszewski AP (2004) Self-reported Morisky score for identifying nonadherence with cardiovascular medications. Ann Pharmacother 38:1363–1368
Peduzzi P, Concato J, Kemper E et al (1996) A simulation study of the number of events per variable in logistic regression analysis. J Clin Epidemiol 49:1373–1379
Dales LG, Ury HK (1978) An improper use of statistical significance testing in studying covariables. Int J Epidemiol 7:373–375
Lekkekerker F, Kanis JA, Alsayed N et al (2007) Adherence to treatment of osteoporosis: a need for study. OsteoporosInt 18:1311–1317
Cramer JA, Amonkar MM, Hebborn A et al (2005) Compliance and persistence with bisphosphonate dosing regimens among women with postmenopausal osteoporosis. Curr Med Res Opin 21:1453–1460
Recker RR, Gallagher R, MacCosbe PE (2005) Effect of dosing frequency on bisphosphonate medication adherence in a large longitudinal cohort of women. Mayo Clin Proc 80:856–861
Casula M, Catapano AL, Piccinelli R et al (2014) Assessment and potential determinants of compliance and persistence to antiosteoporosis therapy in Italy. Am J Manag Care 20:e138–e145
Bianchi ML, Duca P, Vai S et al (2015) Improving adherence to and persistence with oral therapy of osteoporosis. Osteoporos Int 26:1629–1638
Lee S, Glendenning P, Inderjeeth CA (2011) Efficacy, side effects and route of administration are more important than frequency of dosing of anti-osteoporosis treatments in determining patient adherence: a critical review of published articles from 1970 to 2009. Osteoporos Int 22:741–753
van Boven JF, de Boer PT, Postma MJ et al (2013) Persistence with osteoporosis medication among newly-treated osteoporotic patients. J Bone Miner Metab 31:562–570
Bliuc D, Eisman JA, Center JR (2006) A randomized study of two different information-based interventions on the management of osteoporosis in minimal and moderate trauma fractures. Osteoporos Int 17:1309–1317
Leslie WD, Majumdar SR, Lix LM et al (2014) Can change in FRAX score be used to “treat to target”? A population-based cohort study. J Bone Miner Res 29:1074–1080
Clowes JA, Peel NF, Eastell R (2004) The impact of monitoring on adherence and persistence with antiresorptive treatment for postmenopausal osteoporosis: a randomized controlled trial. J Clin Endocrinol Metab 89:1117–1123
Delmas PD, Vrijens B, Eastell R et al (2007) Effect of monitoring bone turnover markers on persistence with risedronate treatment of postmenopausal osteoporosis. J Clin Endocrinol Metab 92:1296–1304
Curtis JR, Cai Q, Wade SW et al (2013) Osteoporosis medication adherence: physician perceptions vs. patients’ utilization. Bone 55:1–6
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
On behalf of all authors, I declare no conflict of interest.
Ethical approval
All procedures performed in this study involving human participants were in accordance with the ethical standards of the institutional and national research committee and with the 1964 Helsinki declaration. Procedures performed in this study did not involve animals.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Rights and permissions
About this article
Cite this article
Gonnelli, S., Caffarelli, C., Rossi, S. et al. How the knowledge of fracture risk might influence adherence to oral therapy of osteoporosis in Italy: the ADEOST study. Aging Clin Exp Res 28, 459–468 (2016). https://doi.org/10.1007/s40520-016-0538-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40520-016-0538-1