Abstract
Studies point to positive outcomes in a diet with reduction of carbohydrates and that the associated practice of intermittent fasting (IF) might increase weight loss. Although dieting might be related to disordered eating, little evidence is available about the role of restrictive carbohydrates diets on disordered eating. This study aimed to explore if doing low-carb (LC) diets was related to disordered eating and if IF would increase these symptoms. The sample comprised university students (n = 682), with a mean age of 22 years old and average BMI of 23.6 kg/m2 (SD = 4.3). Twenty-seven percent (n = 188) of respondents reported doing LC diet in the last three months. Of those, 31% (n = 58) reported doing LC diet combined with periods of IF. Mean scores were compared using parametric tests, and effects size and correlations between variables were calculated. Dieters showed higher levels of binge eating, food cravings, cognitive restraint, cognitive restraint toward carbohydrates when compared to non-dieters. The association of LC and IF was related to an increase in disordered eating, especially binge eating and food cravings, specifically ‘Lack of control’, ‘Thoughts or preoccupation with food,’ and ‘Guilt from cravings and/or for giving in to them’. These results provide evidence that restrictive carbohydrate diets and IF may increase cognitive restraint and, consequently, food cravings.
Level III: Evidence obtained from cohort or case-control analytic studies.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The habit of dieting, although a popular strategy for losing weight, might not be innocuous for a considerable part of the population. Recent evidence points out that it has deleterious effects, especially in developing disordered eating, defined as problematic eating behaviors used to lose or control. [1] Evidence shows that disturbed eating behaviors are more frequent in individuals with body concerns and body dissatisfaction, making them at greater risk of developing eating disorders (ED) [2].
Studies with the university population reveal a high prevalence of disordered eating behaviors among these populations. Usually, they report restrictive eating patterns (diets), binge eating, compensatory behaviors, such as fasting, use of laxatives, and self-induced vomiting [2, 3]. In addition, emotional vulnerability can be present in this population due to changes, such as training, demands, and expectations on academic performance, contributing to altered eating behaviors, such as emotional eating or decrease of quality of diet (pattern of consumption) [4, 5]. As a result, weight gain and dissatisfaction emerge, and the practice of unsupervised diets (without professional counseling) can be a way to deal with this discomfort.
A popular and highly diffused diet is the low-carbohydrate diet (low-carb, LC), where there is a restriction on the consumption of carbohydrate-rich foods. It consists of a decrease in the consumption of carbohydrates in the distribution of macronutrients during the day, usually 30–130 g of carbohydrates/day [6]. There is a great debate regarding its use [7], and the suggested mechanisms for action in weight loss are the reduction of hunger and food cravings (FC) [8], combined with the reduction of lipogenesis and the increase of lipolysis [9]. Furthermore, it is commonly associated with intermittent fasting (IF), defined as an eating pattern that cycles between periods of fasting and eating to achieve more expressive weight loss [6, 10].
Cognitive restraint is the process of mental effort applied to follow a diet. These mental processes resist physiological or non-physiological pressures to eat in normal circumstances and follow the dietary prescription. However, several studies show that restrictive eaters experience more food cravings (FC). These act like a sort of “counterforce” that creates specific food desires and can be accompanied by a sense of urgency that makes the need for these food uncontrollable [11,12,13]. There is a hypothesis that FC mediate the link between restrictive diets and binge eating [14] which is reported as barriers to dietary adherence [15, 16]. Recent studies provide evidence that LC dieters with a history of binge eating experience more food cravings toward carbohydrates-rich foods [17]. However, the literature lacks information about the effects of LC diet on eating behavior, especially the unsupervised practice is usually seen among university students.
Therefore, this study aims to assess the presence of disordered eating behaviors in individuals who practice LC diet. Specifically, we aim to evaluate the presence and intensity of FC, binge eating, cognitive restraint, and cognitive restraint directed to carbohydrates in individuals that practice LC diet versus non-dieters. In addition, we also intend to verify if the practice of IF in LC dieters influences disordered eating behaviors. The hypotheses raised were that (i) LC dieters have higher levels of FC, binge eating, cognitive restraint, and cognitive restraint directed to carbohydrates than non-dieters; and (ii) the practice of IF associated with LC aggravates the severity of binge eating symptoms, cognitive restraint, and cognitive restraint toward carbohydrates.
Materials and methods
Participants
The sample comprised university students (n = 853) of any gender that expressed consent in participating after informed about studies’ goals and procedures. Respondents were included if enrolled in the institution, and have age inferior to 60 years old. Participants who reported lifetime diagnosis of EDs were excluded from the analysis.
Measures
Health and social status. A questionnaire was provided to obtain participants’ information regarding: self-reported ethnic group; area of study; the estimated current weight (in kilograms) and height (in centimeters), to compute body mass index (BMI); type of diet (omnivore, vegetarian or vegan); frequency of tobacco consumption; frequency of alcohol consumption; pregnancy status (current or last year); presence of chronic metabolic diseases (Type 1 or Type 2 Diabetes, Hypertension, Hypercholesterolemia, Celiac disease); lifetime diagnosis of eating disorder; lifetime diagnosis of mood or anxiety disorder.
Binge Eating Scale (BES). The Binge Eating Scale is a self-report scale used to assess the presence and severity of binge eating. This instrument was developed by Gormally and colleagues [18], and was translated and validated into Brazilian Portuguese [19, 20]. The cutoff score for probable presence of binge eating disorder (BED) is 17 points [21], that can be classified in three levels: severe binge eating (scores ≥ 27), moderate binge eating (scores between 18 and 26), and no binge eating (scores ≤ 17). The Brazilian validated version revealed good psychometric characteristics (Cronbach’s Alpha = 0.89), and this cutoff score showed 97% of sensitivity to detect clinical cases of BED when compared to the Structured clinical interview [19]. Similarly, in our sample, Cronbach’s Alpha was 0.88.
Food Cravings Questionnaire Trait and State (FCQ-T; FCQ-S). These are self-report questionnaires to measure FC intensity. The Trait version (FCQ-T) assesses intense desire for food as a constitutional element and is composed of 39 statements to be classified according to a 6-point Likert frequency scale (from ‘never’ to ‘always’. The State version (FCQ-S) measures FC as a mutable element according to situations, environments, or sensations, consisting of 15 statements assessed on a 5-point Likert accordance scale (from ‘strongly disagree’ to ‘strongly agree’). The higher the scores on each scale, the more intense the experience of FC for the respondent. In the study of the Brazilian version, Cronbach’s Alpha was 0.97 for the FCQ-T and 0.91 for the FCQ-S, revealing good consistency levels in this population [22]. Reliability in this sample was 0.97 for the FCQ-T and 0.91 for the FCQ-S.
Screening questionnaire of risk behaviors for eating disorders. This simplified questionnaire assesses the frequency of inappropriate eating behaviors, such as binge eating, purging (self-induced vomiting and/or use of laxatives), and restrictive diet. The scale assesses the frequency of the behavior in the last three months as “none,” “less than once per week,” “once a week,” and “2 or more times per week.” The adapted version in Brazilian Portuguese was used, with a reliability study revealing a kappa value of 0.92, showing evidence of adequate psychometric properties [23]. This scale was used in the present study to characterize compensatory practices among participants with binge eating if they reported compensatory behavior at least one time/week in the last 3 months [17].
Cognitive Restraint Subscale, Three-Factor Eating Questionnaire (TFEQ-CR). The cognitive restraint subscale is used to assess dietary restriction to modify weight or body shape and is a subscale of The Three-Factor Eating Questionnaire (TFEQ). Brazilian translation was published [24], and later validated [25]. Cronbach’s Alpha of CR scale calculated for this sample of 0.84. With higher values indicating a higher level of cognitive restraint.
Cognitive Restraint Subscale adapted for carbohydrates. The aforementioned Cognitive Restraint subscale was adapted to include terms related to carbohydrate restriction. The process was approved in a previous communication with the author (Dr. Jan Karlsson—Örebro University). In the questionnaire heading, participants received instructions on what foods are sources of carbohydrates and were asked the same questions of the original version, but substituting the food terms with foods source of carbohydrates. The score and transformation in the total score were the same as in the original version. The adapted questions were previously published, revealing a Cronbach alpha of 0.84 [17] Cronbach’s Alpha calculated for this sample was 0.86.
Food Consumption Frequency Questionnaire. Some questions from the Food Frequency Questionnaire were used to assess the frequency of consumption of specific types of food in the last 3 months. The frequency ranges from “rarely or never” to “2 or 3 times a week” on a 7-point scale [17]. The foods chosen were chocolate, bread in slices, rice, French roll (type of bread common in Brazil), pasta, and crackers/cookies.
Practice of Low-Carb Diet and Intermittent Fasting. Participants were asked about their practice and frequency of LC diet and IF [2], using the following questions: (a) In the last three months, have you tried to be on a low-carb diet, avoiding foods that are sources of carbohydrate? (“yes”, “no” and “I do not know what a low-carb diet is”); (b) Considering the previous question, in the last three months, how many times in a week have you had intermittent fasting? (‘not applicable’, ‘1 time/ week’, ‘2 times/week’, ‘3 times/week’, ‘every day’); (c) In the last three months, how many hours did you usually fast for? (do not consider sleep period) (answer options: ‘not applicable’, ‘6 h’, ‘8 h’,’12 h’, 16 h’, and’24 h’).
Procedures
Recruitment and data collection
This study was made using a cross-sectional design with a sample of university students, assessed through an online form with measures of eating behavior. After ethical approval by University’s Ethics Board (registration number: 2.695.532), recruitment of participants was made with an invitation via institutional e-mails and publications in groups of university students on Facebook®. Students were provided a link where the goals and procedures of the study were explained and where they could provide their consent. They were then invited to answer the measures of the study. Those who completed the questionnaire and left their e-mail addresses received an invitation to share the electronic form with other colleagues from the university. Questionnaires were distributed to potential participants between July 2018 and March 2019 (pre-COVID-19 pandemic).
Data analysis
Descriptive statistics of the sample, including frequency of categorical variables, and means and standard deviations (SD) for continuous variables are provided. Cronbach’s alpha was calculated to verify reliability indexes of the scales in the studied sample. Kurtosis and skewness of data were assessed to verify data distribution and suitability to parametric analysis [26]. Next, the sample was divided into two groups: the first group (LC) was composed of participants who reported current practice of LC diet; the second group (No diet) comprised participants who reported not practicing LC diet.
Groups were compared using parametric statistical tests (Student’s t test), and Cohen’s d was used to evaluate the effect sizes of differences between groups. The false discovery rate (FDR) was used to correct the comparisons for false positives. Also, Pearson’s correlations between variables of interest (associations with FC scores for low-carb dieters) were performed, in which IF frequency and hours were transformed into dummy variables to the analysis. We considered a significance level of 5% for all tests.
Results
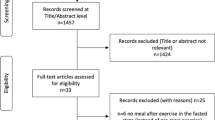
Data of 853 respondents were obtained. From those, participants that reported lifetime diagnosis of eating disorder (n = 48) were excluded. Also, participants that reported practicing IF but did not practice LC diet were excluded from the analysis (n = 123). The remaining sample (n = 682) comprised 75% of women (n = 512) with mean age of 22 years old (SD = 3.3 years). Mean BMI of the total sample was 23.5 kg/m2 (SD = 4.1 kg/m2). The whole sample was divided into two groups: the first was the LC diet group (n = 188), comprised those who answered “yes” to the question “In the last three months, have you tried to be on a low-carb diet, avoiding foods that are sources of carbohydrate?”; and the second one, the No Diet (n = 494) consisted of those who answered “no” or “I do not know what low-carb diet is” to this question.
Description of LC and No diet groups
The LC diet group consisted of 28% of the total sample (n = 159; 84% women), with mean age of 22 years old (SD = 3.2), from which 69% (n = 130) was LC dieters without IF, and 31% (n = 58) were LC dieters and reported practicing IF. The No diet group comprised those that reported not to practice LC diet nor IF in the last three months, consisted of 494 participants (71% women), with an average age of 21 years old (SD = 3.2). No differences on distribution of psychiatric disorders or chronic diseases were found between groups. The description of both groups is presented in Table 1.
LC diet and No diet groups were compared according to their total scores for BES, FCQ-T, FCQ-S, CR-TFEQ and CR-carbohydrate, and food consumption frequency of carbohydrate-rich foods, with results presented in Table 2. In the LC diet group, the average binge eating score was 15.8 (SD = 8.5; range 0–46), and according to the cutoff score of the BES, 39% had significant levels of binge eating (n = 73). Of these, 18.2% (n = 39) reported doing the diet supervised by a nutritionist. In the No diet group, mean scores on BES was 9.9 (SD = 7.0; range 0–38), and 13% had scores above the cutoff for presence of binge eating (n = 66).
Consistently, groups revealed significant differences in all disordered eating variables, with LC dieters showing significant higher levels of cognitive restraint (t = − 15.75; p < 0.001; d = − 1.4) and restraint toward carbohydrates (t = − 18.05; p < 0.001; d = − 1.5). This group also reported higher levels of FC in both scales, FCQ-T and FCQ-S, except for two subscales of FCQ-S: intense desire to eat and FC as a physiological state. When observing the frequency of consumption of carbohydrate-rich foods, LC dieters reported consuming significantly more frequently sliced bread, rice and French rolls (Cohen’s d between 0.2 and 0.7).
We compared BMI distributions among dieters and non-dieters, and found that they differed significantly (X2 = 19.689; p < 0.001), with higher rates of underweight participants among non-dieters (10 vs. 1%) and higher number of overweight in the diet group (26 vs. 18%). Among LC dieters, we compared groups of participants with and without associated IF regarding the distribution of participants’ BMI, according to types of dietary practice. Individuals that reported practicing LC diet, more than half of the individuals (61%) were in the normal weight range, and 38% were overweight or obese. For those that practice LC and IF, 76% had normal weight, and 22% were overweight or obese. Results are displayed in Table 3.
Correlations of LC diet and IF with disordered eating (LC group, n = 188)
In LC group, we found significant positive associations between weekly frequency of IF with higher scores of binge eating (r = 0.16; p < 0.05). When looking at hours of fasting, positive relationship were found with binge eating, cognitive restraint toward carbohydrates, preoccupations about food, guilty, intense desires and lack of control (r from 0.18 and 0.27, p < 0.05). Binge eating scores were moderate to strongly correlated to all FC dimensions, with effect sizes varying between 0.29 and 0.76 (p < 0.01). Regarding cognitive restraint, it was negatively associated to cues that trigger FC (r = − 0.16; p < 0.05), positively associated with guilty from craving (r = 0.28; p < 0.01), and negatively associated with physiological cravings (r = − 0.20; p < 0.01). Also, subscale of cognitive restriction adapted to carbohydrates positive and strongly correlated with its original version (r = 0.82; p < 0.001).
In relation to consumption of carbohydrate foods, positive relationship was found between binge eating scores and consumption of bread (r = 0.14; p < 0.05) and pasta (r = 0.22; p < 0.01). Cognitive restraint (and that toward carbs) was associated with decreased consumption of rice (r = − 0.43 and − 0.45; p < 0.01), French roll bread (r = − 0.23 and − 0.26; p < 0.01) and pasta (r = − 0.31 and − 0.36; p < 0.01). Inversely, higher levels of FCQT were associated with increased frequency of chocolate (r = 0.17; p < 0.05) and pasta consumption (r = 0.24; p < 0.01). Consumption of chocolate, sliced bread and pasta were also significantly correlated with increased FC state (r = 0.19 and 0.26, p < 0.05). All correlations between measures are presented in Table 4.
Discussion
Our study aimed to explore the relationship between the practice of LC diet with or without IF and the presence of disordered eating behaviors among a population sample of university students. LC dieters were compared to non-dieters to explore the association between restriction of carbohydrates and disturbed eating. The participants were primarily women, both in the LC diet group (85%) and in the group that associated it with IF (98%). We provide evidence about the significant association between cognitive restraint toward carbohydrates, FC levels, and disordered eating behaviors in LC dieters, compared to non-dieters. Also, when associated with IF, LC dieters have potentially more binge eating symptoms and FC (trait). However, higher hours of fasting were also associated with increased cognitive restriction toward carbohydrates, although effect size of this relationship was modest.
Although LC diet appears to be a successful way to lower body weight [27], our data reveal that this restrictive diet is related to worse eating attitudes. Specifically, they reported higher binge eating symptoms, cognitive restriction, and food cravings. Furthermore, individuals with disordered eating attitudes tend to disregard context, frequency, and quantity of food and their attunement with the current state of the body, making choices based on established beliefs [28]. This diet mentality is described in one of the questions of the adapted subscale of cognitive restriction toward carbohydrates: “I do not eat some food (source of carbohydrates) because they make me fat”.
For LC dieters, the ‘anticipation of relief from negative states and feelings’ was greater, indicating the possible use of food to deal with emotions [29]. However, from the behavioral point of view, the association between cognitive restraints toward carbohydrates showed negative associations with the FCQ-T ‘Anticipation of the positive reinforcement’ and ‘Cues that may trigger FC’ subscale and positive associations with subscale ‘Guilt from cravings and/or for giving in to them’. These results indicate that restrictive dietary attitudes toward food, particularly carbohydrate consumption, suppress facets of positive reinforcement and responsiveness for cues that may trigger FC, with a consequent rise of guilt, which positively correlates with cognitive restraint toward carbohydrates.
One possible mechanism by which guilt is associated with cognitive restraint in LC dieters is the role of this practice as a form of social representativeness and shared beliefs about food and health that are endorsed in this group [30]. The LC diet was highly promoted as a new lifestyle, and popular discourse mentions the Paleolithic period as a way of convincing that high fat consumption is natural and primitive [31]. New standpoints from this perspective also consider the level of food processing and quality of the diet instead of the unrestricted consumption of food sources of proteins or fats. Additionally, “nutritionism” (tendency to systematize and excessively focus on nutrients instead of food), and disturbing patterns concerning ‘pure’ food consumption may increase, with a focus on the quality of the diet as an additional combo of dietary rules [32, 33]. In that scenario, individuals who struggle to stay on the diet when episodes of overeating or binge eating occur might experience increased guilt for seeing themselves as incapable of following the ‘lifestyle’, resulting in a greater sense of isolation and self-judgment [34].
The group that associated LC with fasting reported higher binge eating and an FC compared to those who only remained on a diet. As for the BMI distribution between subgroups, LC and IF had proportionally less participants in the overweight and obesity range. Vargas and colleagues [10] demonstrated that LC promoted greater weight loss while fasting promoted a greater decrease in waist circumference and fat percentage, although there are no superior results compared to classical caloric restriction [35]. Still, those that combined LC and IF revealed increased aspects of FC, such as ‘lack of control’, ‘thoughts and concerns about food’, ‘cues that may trigger food cravings’, and ‘guilt that may be experienced due to cravings and/or giving into them’, revealing that the experience of restriction increases self-regulation disturbances and disordered eating. Considering ED, fasting is also used for weight control or as a compensatory method after consuming more than the desired or unplanned amount of food [12] which raises the hypothesis that the combination of quality and quantity restriction promoted by the association of the methods are more deleterious for eating behaviors and might increase risk of ED. However, this is yet to be investigated.
It is essential to point out that the present study has limitations. First, we used a web-recruited university sample, which might be a source of bias. It is possible that respondents with eating problems or concerns were more willing to contribute to the research. There is also an essential question about gender because the participants were mostly women that are culturally more prone to body concerns and preferential practitioners of diets. Also, due to the dissonant parameters for classifying a LC diet, a standardized assessment of food consumption would be desirable to characterize individuals with low-carbohydrate consumption.
Nonetheless, our study brings important findings that shed light on carbohydrate-restricted diets’ influence on disordered eating. When combined with intermittent fasting, LC diet increased binge eating and food craving symptoms, especially those related to self-control and guilt. Future studies should address specific factors of the diet that might contribute to this relationship, such as beliefs about food and health and the use of food for emotional regulation.
What is already known on this subject?
Previous studies reveal that practice of low-carb diet is associated with higher levels of food craving in individuals with binge eating and eating disorders.
What does this study add?
This study provides evidence about the association between low-carb diet and increase of disordered eating in individuals without eating disorders. Compared to non-dieters, those who practice LC diet have significantly higher levels of binge eating symptoms, cognitive restraint and food cravings.
References
Urquhart CS, Mihalynuk TV (2011) Disordered eating in women: implications for the obesity pandemic. Can J Diet Pract Res a Publ Dietitians Canada Rev Can La Prat La Rech En Diet Une Publ Des Diet Du Canada. 72:e115–e125. https://doi.org/10.3148/72.1.2011.50
de Oliveira J, Figueredo L, Cordás TA (2019) Prevalência de comportamentos de risco para transtornos alimentares e uso de dieta _low-carb_ em estudantes universitários. J Bras Psiquiatr 68:183–190
Trindade AP, Appolinario JC, Mattos P, Treasure J, Nazar BP (2019) Eating disorder symptoms in Brazilian university students: a systematic review and meta-analysis. Brazilian J Psychiatry 41:179–187. https://doi.org/10.1590/1516-4446-2018-0014
Nogueira-Martins LA, Nogueira- Martins MCF (2018) Saúde mental e qualidade de vida de estudantes universitários. Rev Psicol Divers e Saúde 7:334–337. https://doi.org/10.17267/2317-3394rpds.v7i3.2086
Perez PMP, de Castro IRR, FrancoAda S, Bandoni DH, Wolkoff DB (2016) Práticas alimentares de estudantes cotistas e não cotistas de uma universidade pública Brasileira. Cienc e Saude Coletiva 21:531–542. https://doi.org/10.1590/1413-81232015212.01732015
Freire R (2020) Scientific evidence of diets for weight loss: different macronutrient composition, intermittent fasting, and popular diets. Nutrition 69:110549. https://doi.org/10.1016/j.nut.2019.07.001
Astrup A, Hjorth MF (2017) Low-fat or low carb for weight loss? It depends on your glucose metabolism. EBioMedicine 22:20–21. https://doi.org/10.1016/j.ebiom.2017.07.001
Anguah KOB, Syed-Abdul MM, Hu Q, Jacome-Sosa M, Heimowitz C, Cox V et al (2020) Changes in food cravings and eating behavior after a dietary carbohydrate restriction intervention trial. Nutrients 12:7–18. https://doi.org/10.3390/nu12010052
Paoli A, Rubini A, Volek JS, Grimaldi KA (2013) Beyond weight loss: a review of the therapeutic uses of very-low-carbohydrate (ketogenic) diets. Eur J Clin Nutr 67:789–796. https://doi.org/10.1038/ejcn.2013.116
Vargas AJ, de PessoaS L, Rosa RL (2018) Jejum intermitente e dieta low carb Na composição corporal e no comportamento alimentar de mulheres praticantes de atividade física. Rev Bras Nutr Esportiva 12:483–490
Kavanagh DJ, Andrade J, May J (2005) Imaginary relish and exquisite torture: the elaborated intrusion theory of desire. Psychol Rev 112:446–467. https://doi.org/10.1037/0033-295X.112.2.446
Oliveira J, Cordás TA (2020) The body asks and the mind judges: Food cravings in eating disorders. Encephale 46:269–282. https://doi.org/10.1016/j.encep.2020.01.003
Schumacher S, Kemps E, Tiggemann M (2019) The food craving experience: Thoughts, images and resistance as predictors of craving intensity and consumption. Appetite 133:387–392. https://doi.org/10.1016/j.appet.2018.11.018
Meule A, Papies EK, Kübler A (2012) Differentiating between successful and unsuccessful dieters. Validity and reliability of the perceived self-regulatory success in dieting scale. Appetite 58:822–826. https://doi.org/10.1016/j.appet.2012.01.028
Polivy J, Coleman J, Herman CP (2005) The effect of deprivation on food cravings and eating behavior in restrained and unrestrained eaters. Int J Eat Disord 38:301–309. https://doi.org/10.1002/eat.20195
Verzijl CL, Ahlich E, Schlauch RC, Rancourt D (2018) The role of craving in emotional and uncontrolled eating. Appetite 123:146–151. https://doi.org/10.1016/j.appet.2017.12.014
de Oliveira J, Colombarolli MS, Figueredo LS, Cordás TA (2021) Cognitive restraint directed at carbohydrates in individuals on low-carb diet with binge eating: the role of guilt about food cravings. Einstein (São Paulo). https://doi.org/10.31744/einstein_journal/2021AO5599
Gormally JIM, Black S, Daston S, Rardin D (1982) The assessment of binge eating severity among obese persons. Addict Behav 7:47–55
Freitas S, Lopes CS, Coutinho W, Appolinario JC (2001) Tradução e adaptação para o português da Escala de Compulsão Alimentar Periódica Translation and adaptation into Portuguese of the Binge-Eating Scale. Rev Bras Psiquiatr 23:215–220. https://doi.org/10.1590/S1516-44462001000400008
Appolinario JC, Cordás TA, Medeiros CA (2002) Transtornos alimentares. Rev Bras Psiquiatr 24:1–2. https://doi.org/10.1590/S1516-44462002000600007
Marcus MD, Wing RR, Lamparski DM (1985) Binge eating and dietary restraint in obese patients. Addict Behav 10:163–168
Ulian MD, Sato PDM, Benatti FB, De Campos-Ferraz PL, Roble OJ, Unsain RF et al (2017) Cross-cultural adaptation of the state and trait food cravings questionnaires (FCQ-S and FCQ-T) into Portuguese. Cienc e Saude Coletiva 22:403–416. https://doi.org/10.1590/1413-81232017222.18272015
de FerreiraS JE, Veigada GV (2008) Confiabilidade (teste-reteste) de um questionário simplificado para triagem de adolescentes com comportamentos de risco para transtornos alimentares em estudos epidemiológicos. Rev Bras Epidemiol 11:393–401. https://doi.org/10.1590/S1415-790X2008000300006
Natacci LC, Júnior MF (2011) The three factor eating questionnaire-R21: tradução para o português e aplicação em mulheres brasileiras. Rev Nutr 24:383–394. https://doi.org/10.1590/S1415-52732011000300002
de Medeiros ACQ, Yamamoto ME, Pedrosa LFC, Hutz CS (2017) The Brazilian version of the three-factor eating questionnaire-R21: psychometric evaluation and scoring pattern. Eat Weight Disord 22:169–175. https://doi.org/10.1007/s40519-016-0256-x
Kim H-Y (2013) Statistical notes for clinical researchers: assessing normal distribution (2) using skewness and kurtosis. Restor Dent Endod 38:52–54. https://doi.org/10.5395/rde.2013.38.1.52
Hume DJ, Kroff J, Clamp LD, Lambert EV (2015) Compensations for weight loss in successful and unsuccessful dieters. Am J Health Behav 39:589–600. https://doi.org/10.5993/AJHB.39.5.1
Tribole E, Resch E (2020) Intuitive eating: A revolutionary anti-diet approach. St. Martin’s Essentials, New York
Rosenberg N, Bloch M, Ben Avi I, Rouach V, Schreiber S, Stern N et al (2013) Cortisol response and desire to binge following psychological stress: comparison between obese subjects with and without binge eating disorder. Psychiatry Res 208:156–161. https://doi.org/10.1016/j.psychres.2012.09.050
Polivy J, Herman CP (2017) Restrained eating and food cues: recent findings and conclusions. Curr Obes Rep 6:79–85. https://doi.org/10.1007/s13679-017-0243-1
Pitt CE (2016) Cutting through the Paleo hype: the evidence for the Palaeolithic diet. Aust Fam Physician 45:35–38
Mayes CR, Thompson DB (2015) What should we eat? biopolitics, ethics, and nutritional scientism. J Bioeth Inq 12:587–599. https://doi.org/10.1007/s11673-015-9670-4
Sanlier N, Yassibas E, Bilici S, Sahin G, Celik B (2016) Does the rise in eating disorders lead to increasing risk of orthorexia nervosa? Correlations with gender, education, and body mass index. Ecol Food Nutr 55:266–278. https://doi.org/10.1080/03670244.2016.1150276
Pellerano JA, Gimenes-Minasse MHSG (2015) “Low carb high fat”: comensalidade E sociabilidade em tempos de dietas restritivas. DEMETRA Aliment Nutr Saúde 10:493–506. https://doi.org/10.12957/demetra.2015.16108
Paoli A, Bosco G, Camporesi EM, Mangar D (2015) Ketosis, ketogenic diet and food intake control: a complex relationship. Front Psychol 6:1–9. https://doi.org/10.3389/fpsyg.2015.00027
Funding
Partial financial support was received from Coordenação de Aperfeiçoamento de Pessoal de Nível Superior of Brazil (CAPES) (Finance Code 001), Brazilian National Council for Scientific and Technological Development (CNPq), and University of Turin.
Author information
Authors and Affiliations
Contributions
MSC was responsible for methodological design, data analysis, and manuscript review. JO was responsible for data collection, data analysis, and manuscript first draft. TAC was responsible for designing the study and manuscript review. All authors reviewed and approved submitted version of the manuscript.
Corresponding author
Ethics declarations
Conflicts of interest
The authors have no competing interests to declare that are relevant to the content of this article.
Ethical approval
Data reported in this manuscript were collected and processed following the Declaration of Helsinki, with the approval of the ethics committee of the School of Medicine of the University of Sao Paulo (Registration number CAAE:88846718.7.0000.0065).
Informed consent
All participants provided informed consent prior to their participation.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Colombarolli, M.S., de Oliveira, J. & Cordás, T.A. Craving for carbs: food craving and disordered eating in low-carb dieters and its association with intermittent fasting. Eat Weight Disord 27, 3109–3117 (2022). https://doi.org/10.1007/s40519-022-01437-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40519-022-01437-z