Abstract
Purpose
Little is known about the association between dinner-to-bed time and obesity. Thus, this study was aimed to assess the relationships between dinner-to-bed and overweight/obesity in Chinese school-aged children in Ningbo, China.
Methods
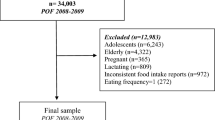
Data of this study were based on 1667 schoolchildren (14–15 years) from 14 primary schools participated in this study in China. Anthropometric measurement of height, body weight and waist circumference (WC) was performed. Information about meal duration and other lifestyle behaviors was collected using a self-administered questionnaire. Multivariable logistic regression model was performed to assess the association between dinner-to-bed time and overweight/obesity. Restricted cubic spline regression was drawn to evaluate the shape of the relation between dinner-bed-time and the odds of overweight.
Results
Among the study participants, the prevalence of overweight was 17.6%, and the mean of dinner-to-bed time was 4.26 (0.93) h. In the logistic regression analysis, participants who had dinner-to-bed time less than 3 h or 3.01 ~ ≦ 4.00 h are more likely to be overweight (OR = 1.94, 95% CI 1.10–3.42; OR = 1.65, 95% CI 1.03–2.65, respectively) or characterised by abdominal obesity (OR = 3.03, 95% CI 1.86–4.95; OR = 2.61, 95% CI 1.73–3.92, respectively) compared with dinner-to-bed time more than 5 h. In addition, long dinner-to-bed time was associated with lower risks of overweight (OR = 0.83, 95% CI 0.70–0.97) and abdominal obesity (OR = 0.63, 95% CI 0.54–0.73). The cubic spline regression analysis showed that the association between dinner-to–bed time and overweight/abdominal obesity seems to be a linear.
Conclusions
This study indicates that short dinner-to-bed time is associated with an increased likelihood of being overweight or characterised by abdominal obesity among Chinese school-aged children.
Level of evidence
Level V; cross-section descriptive study.


Similar content being viewed by others
Data availability
Additional data can on request be made available.
References
Su C, Zhang B, Wang YF, Jia XF, Xue H, Wang HJ (2015) Epidemics of overweight and obesity among growing childhood in China between 1997 and 2009: impact of family income, dietary intake, and physical activity dynamics. Chin Med J (Engl) 128(14):1879–1886. https://doi.org/10.4103/0366-6999.160648
Zhang J, Li X, Hawley N et al (2018) Trends in the prevalence of overweight and obesity among chinese school-age children and adolescents from 2010 to 2015. Child Obes 14(3):182–188. https://doi.org/10.1089/chi.2017.0309
Yatsuya H, Li Y, Hilawe EH et al (2014) Global trend in overweight and obesity and its association with cardiovascular disease incidence. Circ J 78(12):2807–2818. https://doi.org/10.1253/circj.cj-14-0850
Story M, Sallis JF, Orleans CT (2009) Adolescent obesity: towards evidence-based policy and environmental solutions. J Adolesc Health 45(3 Suppl):S1–S5. https://doi.org/10.1016/j.jadohealth.2009.06.022
Logue J, Sattar N (2010) Obesity in children and future cardiometabolic risk: are blood tests necessary? Diabetes Care 33(12):2711–2712. https://doi.org/10.2337/dc10-1748
Mora-Gonzalez J, Esteban-Cornejo I, Solis-Urra P et al (2020) Fitness, physical activity, sedentary time, inhibitory control, and neuroelectric activity in children with overweight or obesity: the ActiveBrains project. Psychophysiology 57(6):e13579. https://doi.org/10.1111/psyp.13579
Mayer EI, Reuter M, Dopfer RE, Ranke MB (2000) Energy expenditure, energy intake and prevalence of obesity after therapy for acute lymphoblastic leukemia during childhood. Horm Res 53(4):193–199. https://doi.org/10.1159/000023566
Horikawa C, Kodama S, Yachi Y et al (2011) Skipping breakfast and prevalence of overweight and obesity in Asian and Pacific regions: a meta-analysis. Prev Med 53(4–5):260–267. https://doi.org/10.1016/j.ypmed.2011.08.030
Gong QH, Li SX, Wang SJ, Wu YH, Han LY, Li H (2020) Sleep duration and overweight in Chinese adolescents: a prospective longitudinal study with 2-year follow-up. Sleep Breath 24(1):321–328. https://doi.org/10.1007/s11325-019-01979-0
McHill AW, Phillips AJ, Czeisler CA et al (2017) Later circadian timing of food intake is associated with increased body fat. Am J Clin Nutr 106(5):1213–1219. https://doi.org/10.3945/ajcn.117.161588
Hsieh SD, Muto T, Murase T, Tsuji H, Arase Y (2010) Association of short sleep duration with obesity, diabetes, fatty liver and behavioral factors in Japanese men. Intern Med 50:2499–2502. https://doi.org/10.2169/internalmedicine.50.5844
Yoshida J, Eguchi E, Nagaoka K, Ito T, Ogino K (2018) Association of night eating habits with metabolic syndrome and its components: a longitudinal study. BMC Public Health 18(1):1366. https://doi.org/10.1186/s12889-018-6262-3
Xu L, Zhang X, Lu J et al (2016) The effects of dinner-to-bed time and post-dinner walk on gastric cancer across different age groups. Medicine (Baltimore) 95(16):e3397
Fujiwara Y, Machida A, Watanabe Y et al (2005) Association between dinner-to-bed time and gastro-esophageal reflux disease. Am J Gastroenterol 100(12):2633–2636. https://doi.org/10.1111/j.1572-0241.2005.00354.x
Lin Y, Peng Y, Liang B et al (2018) Associations of dinner-to-bed time, post-dinner walk and sleep duration with colorectal cancer: a case-control study. Medicine (Baltimore) 97:e12038. https://doi.org/10.1097/MD.0000000000012038
Gong QH, Li H, Zhang XH, Zhang T, Cui J, Xu GZ (2017) Associations between sleep duration and physical activity and dietary behaviors in Chinese adolescents: results from the Youth Behavioral Risk Factor Surveys of 2015. Sleep Med 37:168–173. https://doi.org/10.1016/j.sleep.2017.06.024
Zhang J, Wang H, Wang Z et al (2018) Prevalence and stabilizing trends in overweight and obesity among children and adolescents in China, 2011–2015. BMC Public Health 18(1):571. https://doi.org/10.1186/s12889-018-5483-9
Gong QH, Li SX, Li H, Cui J, Xu GZ (2018) Insufficient sleep duration and overweight/obesity among adolescents in a Chinese population. Int J Environ Res Public Health 15(5):997. https://doi.org/10.3390/ijerph15050997
Cole TJ, Bellizzi MC, Flegal KM, Dietz WH (2000) Establishing standard definition for child overweight and obesity worldwide: international survey. BMJ 320(7244):1240–1243. https://doi.org/10.1136/bmj.320.7244.1240
Cole TJ, Flegal KM, Nicholls D, Jackson AA (2007) Body mass index cut offs to define thinness in children and adolescents: international survey. BMJ 335(7612):194. https://doi.org/10.1136/bmj.39238.399444.55
Wu LJ, Ma J, Fu LG et al (2013) Association between abdominal obesity and blood pressure among 7 to 10 years old Chinese children. Zhonghua Yu Fang Yi Xue Za Zhi (Chinese) 47(8):689–694 (Article in Chinese)
Xiao Q, Garaulet M, Scheer FAJL (2019) Meal timing and obesity: interactions with macronutrient intake and chronotype. Int J Obes (Lond) 43(9):1701–1711. https://doi.org/10.1038/s41366-018-0284-x
Berg C, Lappas G, Wolk A et al (2009) Eating patterns and portion size associated with obesity in a Swedish population. Appetite 52(1):21–26. https://doi.org/10.1016/j.appet.2008.07.008
Soreca I, Wallace ML, Hall MH, Hasler BP, Frank E, Kupfer DJ (2016) The association between meal timing and frequency with cardiometabolic profile in patients with bipolar disorder. Acta Psychiatr Scand 133(6):453–458. https://doi.org/10.1111/acps.12578
Wang JB, Patterson RE, Ang A, Emond JA, Shetty N, Arab L (2014) Timing of energy intake during the day is associated with the risk of obesity in adults. J Hum Nutr Diet 27(suppl 2):255–262. https://doi.org/10.1111/jhn.12141
Gluck ME, Venti Ca Fau-Salbe AD, Salbe Ad Fau-Krakoff J (2008) Nighttime eating: commonly observed and related to weight gain in an inpatient food intake study. Am J Clin Nutr 88(4):900–905. https://doi.org/10.1093/ajcn/88.4.900
Romon M, Edme JL, Boulenguez C, Lescroart JL, Frimat P (1993) Circadian variation of diet-induced thermogenesis. Am J Clin Nutr 57:476–480. https://doi.org/10.1093/ajcn/57.4.476
Scheer FA, Hilton MF, Mantzoros CS, Shea SA (2009) Adverse metabolic and cardiovascular consequences of circadian misalignment. Proc Natl Acad Sci USA 106(11):4453–4458. https://doi.org/10.1073/pnas.0808180106
Morgan CM, Tanofsky-Kraff M, Yanovski SZ, Jorge MR, Yanovki JA (2002) Loss of control over eating, body fat, and psychopathology in normal weight and overweight children. Int J Eat Disord 35(4):430–441. https://doi.org/10.1002/eat.10038
Heather S, Paul R, Eric S (2018) Using participant feedback to improve two selective eating disorder and obesity prevention programs. Eat Behav 30:93–97. https://doi.org/10.1016/j.eatbeh.2018.06.006
Sofer S, Stark AH, Madar Z (2015) Nutrition targeting by food timing: time-related dietary approaches to combat obesity and metabolic syndrome. Adv Nutr 6(2):214–223. https://doi.org/10.3945/an.114.007518
Bezerra IN, Sichieri R (2009) Eating out of home and obesity: a Brazilian nationwide survey. Public Health Nutr 12(11):2037–2043. https://doi.org/10.1017/S1368980009005710
Maruyama K, Sato S, Ohira T et al (2008) The joint impact on being overweight of self reported behaviours of eating quickly and eating until full: cross sectional survey. BMJ 337:a2002. https://doi.org/10.1136/bmj.a2002
Funding
This study was funded by grants from the Nature Science Foundation of Ningbo (NO. 2016A610181, 2018A610403), Ningbo Health Branding Subject Fund (PPXK2018-10). The authors greatly to the participants of the NYRBS study.
Author information
Authors and Affiliations
Contributions
HL and QHG designed the research. QHG and SJW carried out the statistical analysis and drafted the manuscript. SXL and QHG contributed to the writing of the manuscript and provided critical comments. All the authors read and approved the final manuscript submitted for publication.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This study was approved by the ethics committee of Ningbo Center for Disease Control and Prevention (201703).
Rights and permissions
About this article
Cite this article
Gong, QH., Li, SX., Wang, SJ. et al. Dinner-to-bed time is independently associated with overweight/obesity in Chinese school-aged children. Eat Weight Disord 26, 2657–2663 (2021). https://doi.org/10.1007/s40519-021-01129-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40519-021-01129-0