Abstract
Purpose
Individuals with Prader–Willi syndrome (PWS) exhibit reduced lean body mass and increased fat–lean mass ratio when compared with individuals of normal weight and obese ones. Thus, research on the association of functional limitations during gait and body composition may be of great importance from a rehabilitative viewpoint. In particular, the aim of this study was to compare the gait profile of persons with PWS to that of unaffected individuals and to see if a relationship exists between gait profile and body composition in individuals with PWS.
Methods
Eighteen individuals with PWS and 20 unaffected individuals (Healthy Group: HG) were assessed. Their gait pattern was quantified with 3D-Gait Analysis (3D-GA). Overall body weight, lean and fat masses were measured by dual-energy X-ray absorptiometry.
Results
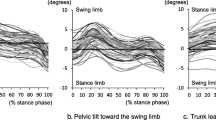
Individuals with PWS were found to be characterized by a significantly different (p < 0.05) gait pattern with respect to healthy controls in terms of both kinematic and kinetic parameters. No correlations were found between kinematic parameters and overall mass and lean/fat mass, while some parameters associated with ground reaction force were found to be significantly correlated with overall mass, lean mass and fat mass. Significant regression models were obtained, including impact and propulsive force and loading rate.
Conclusion
Our data suggest that in individuals with PWS, gait is influenced by the overall and lean body mass. Thus, therapeutic strategies should target both weight reduction and lean mass increase to optimize gait, minimize articular stress, and reduce the risk of repetitive strain on the lower limbs.
Level of evidence
Level III: Case–control analytic study.




Similar content being viewed by others
References
Cassidy SB, Schwartz S, Miller JL, Driscoll DJ (2012) Prader–Willi syndrome. Genet Med 14:10–26
Angulo MA, Butler MG, Cataletto ME (2015) Prader–Willi syndrome: a review of clinical, genetic, and endocrine findings. J Endocrinol Investig 38:1249–1263. https://doi.org/10.1007/s40618-015-0312-9
Theodoro MF, Talebizadeh Z, Butler MG (2006) Body composition and fatness patterns in Prader–Willi syndrome: comparison with simple obesity. Obesity 14:1685–1690
Tanaka Y, Abe Y, Oto Y, Itabashi H, Shiraishi M, Yoshino A, Obata K, Murakami N, Nagai T (2012) Characterization of fat distribution in Prader-Willi syndrome: relationships with adipocytokines and influence of growth hormone treatment. Am J Med Genet Part A 161:27–33. https://doi.org/10.1002/ajmg.a.35653
Bedogni G, Grugni G, Tringali G, Agosti F, Bedogni G, Grugni G, Tringali G, Agosti F, Bedogni G, Grugni G, Tringali G, Agosti F, Sartorio A (2015) Assessment of fat-free mass from bioelectrical impedance analysis in obese women with Prader–Willi syndrome assessment of fat-free mass from bioelectrical impedance analysis in obese women with Prader–Willi syndrome. Ann Hum Biol. https://doi.org/10.3109/03014460.2014.990922
Backholer K, Wong E, Freak-Poli R, Walls HL, Peeters A (2012) Increasing body weight and risk of limitations in activities of daily living: a systematic review and meta-analysis. Obes Rev 13:456–468. https://doi.org/10.1111/j.1467-789X.2011.00970.x
Richmond SA, Kang J, Emery CA (2013) Is body mass index a risk factor for sport injury in adolescents? J Sci Med Sport 16:401–405. https://doi.org/10.1016/j.jsams.2012.11.898
Cimolin V, Galli M, Grugni G, Vismara L, Albertini G, Rigoldi C, Capodaglio P (2010) Gait patterns in Prader–Willi and Down syndrome patients. J NeuroEng Rehabil. https://doi.org/10.1186/1743-0003-7-28
Vismara L, Romei M, Galli M, Montesano A, Baccalaro G, Crivellini M, Grugni G (2007) Clinical implications of gait analysis in the rehabilitation of adult patients with “Prader–Willi” syndrome: a cross-sectional comparative study (“Prader–Willi” syndrome vs matched obese patients and healthy subjects). J NeuroEng Rehabil 4:1–7. https://doi.org/10.1186/1743-0003-4-14
Cimolin V, Cau N, Galli M, Santovito C, Grugni G, Capodaglio P (2017) Gait initiation and termination strategies in patients with Prader–Willi syndrome. J NeuroEng Rehabil. https://doi.org/10.1186/s12984-017-0257-7
Capodaglio P, Menegoni F, Vismara L, Cimolin V, Grugni G, Galli M (2011) Characterisation of balance capacity in Prader–Willi patients. Res Dev Disabil. https://doi.org/10.1016/j.ridd.2010.09.002
Menegoni F, Galli M, Tacchini E, Vismara L, Cavigioli M, Capodaglio P (2009) Gender-specific effect of obesity on balance. Obesity 17:1951–1956. https://doi.org/10.1038/oby.2009.82
Galli M, Crivellini M, Sibella F, Montesano A, Bertocco PPC (2000) Sit-to-stand movement analysis in obese subjects. Int J Obes 24:1488–1492
Reus L, Pillen S, Pelzer BJ, van Alfen-van der Velden JAAEM, Hokken-Koelega ACS, Zwarts M, Otten BJ, Nijhuis-van der Sanden MWG (2014) Growth hormone therapy, muscle thickness, and motor development in Prader–Willi syndrome: an RCT. Pediatrics 134:e1619–e1627. https://doi.org/10.1542/peds.2013-3607
Reus L, Zwarts M, Van Vlimmeren LA, Willemsen MA, Otten BJ, Der Sanden MWGN (2011) Neuroscience and biobehavioral reviews motor problems in Prader–Willi syndrome: a systematic review on body composition and neuromuscular functioning. Neurosci Biobehav Rev 35:956–969. https://doi.org/10.1016/j.neubiorev.2010.10.015
Baker R, McGinley JL, Schwartz MH, Beynon S, Rozumalski A, Graham HK, Tirosh O (2009) The gait profile score and movement analysis profile. Gait Posture 30:265–269. https://doi.org/10.1016/j.gaitpost.2009.05.020
Celletti C, Galli M, Cimolin V, Castori M, Tenore N, Albertini G, Camerota F (2013) Research in developmental disabilities use of the Gait Profile Score for the evaluation of patients with joint hypermobility syndrome/Ehlers–Danlos syndrome hypermobility type. Res Dev Disabil 34:4280–4285. https://doi.org/10.1016/j.ridd.2013.09.019
McMulkin ML, MacWilliams BA (2008) Intersite variations of the Gillette Gait Index. Gait Posture 28:483–487. https://doi.org/10.1016/j.gaitpost.2008.03.002
Pau M, Corona F, Pili R, Casula C, Sors F, Bien M, Kleiner A, Pau M (2016) Effects of physical rehabilitation integrated with rhythmic auditory stimulation on spatio-temporal and kinematic parameters of gait in Parkinson’s disease. Front Neurol 7:1–12. https://doi.org/10.3389/fneur.2016.00126
Galli M, Cimolin V, De Pandis MF, Le Pera D, Sova I, Albertini G, Stocchi F, Franceschini M (2016) Robot-assisted gait training versus treadmill training in patients with Parkinson’s disease: a kinematic evaluation with gait profile score. Funct Neurol 31:1. https://doi.org/10.11138/FNeur/2016.31.3.163
Coghe G, Pau M, Mamusa E, Pisano C, Pilloni G, Porta M, Marrosu G, Frau J, Lorefice L, Fenu G, Giovanna M, Cocco E, Coghe G, Pau M, Mamusa E, Pisano C, Corona F, Pilloni G, Porta M, Marrosu G, Vannelli A, Frau J, Lorefice L, Fenu G, Marrosu MG, Cocco E (2018) Quantifying gait impairment in individuals affected by Charcot–Marie–Tooth disease: the usefulness of gait profile score and gait variable score. Disabil Rehabil. https://doi.org/10.1080/09638288.2018.1506946
Sims DT, Burden A, Payton C, Morse CI (2019) A quantitative description of self-selected walking in adults with Achondroplasia using the gait profile score. Gait Posture 68:150–154. https://doi.org/10.1016/j.gaitpost.2018.11.019
Galli M, Cimolin V, Rigoldi C, Kleiner A, Condoluci C, Albertini G (2015) Use of the gait profile score for the quantification of gait pattern in down syndrome. J Dev Phys Disabil. https://doi.org/10.1007/s10882-015-9438-0
Pau M, Coghe G, Atzeni C, Corona F, Pilloni G, Marrosu MG, Cocco E, Galli M (2014) Novel characterization of gait impairments in people with multiple sclerosis by means of the gait profile score. J Neurol Sci 345:159–163. https://doi.org/10.1016/j.jns.2014.07.032
Schreiber C, Armand S, Moissenet F (2018) Influence of normative data’ s walking speed on the computation of conventional gait indices. J Biomech 76:68–73. https://doi.org/10.1016/j.jbiomech.2018.05.022
Beynon S, Mcginley JL, Dobson F, Baker R (2010) Correlations of the gait profile score and the movement analysis profile relative to clinical judgments. Gait Posture 32:129–132. https://doi.org/10.1016/j.gaitpost.2010.01.010
Ferreira LAB, Cimolin V, Costici PF, Albertini G, Oliveira CS, Galli M (2014) Effects of gastrocnemius fascia lengthening on gait pattern in children with cerebral palsy using the gait profile score. Res Dev Disabil. https://doi.org/10.1016/j.ridd.2014.02.001
Kark L, Vickers D, McIntosh A, Simmons A (2012) Use of gait summary measures with lower limb amputees. Gait Posture 35:238–243. https://doi.org/10.1016/j.gaitpost.2011.09.013
Pamukoff DN, Lewek MD, Blackburn JT (2016) Clinical biomechanics greater vertical loading rate in obese compared to normal weight young adults. JCLB 33:61–65. https://doi.org/10.1016/j.clinbiomech.2016.02.007
Villarrasa-sapiña I, Serra-añó P, Pardo-ibáñez A, Gonzalez L, García-massó X (2017) Clinical biomechanics relationship between body composition and vertical ground reaction forces in obese children when walking. Clin Biomech 41:77–81. https://doi.org/10.1016/j.clinbiomech.2016.12.008
Mündermann A, Dyrby CO, Andriacchi TP (2005) Secondary gait changes in patients with medial compartment knee osteoarthritis: increased load at the ankle, knee, and hip during walking. Arthritis Rheum 52:2835–2844. https://doi.org/10.1002/art.21262
Neri M, Andermacher E, Spanó A, Salvioli GCC (1992) Validation study of the italian version of the Cambridge mental disorders of the elderly examination: preliminary findings. Dementia 3:70–77
Davis RB, Ounpuu S, Tyburski D, Gage JR (1991) A gait analysis data collection and reduction technique. Hum Mov Sci 10:575–597
LaRoche Dain P, Kralian RJ, Millett ED (2011) Fat mass limits lower-extremity relative strength and maximal walking performance in older women. J Electromyogr Kinesiol 21:754–761. https://doi.org/10.1016/j.jelekin.2011.07.006.Fat
Lai PPK, Leung AKL, Li ANM, Zhang M (2008) Three-dimensional gait analysis of obese adults. Clin Biomech 23:2–6. https://doi.org/10.1016/j.clinbiomech.2008.02.004
Vincent HK, Vincent KR, Lamb KM (2010) Obesity and mobility disability in the older adult. Diagn Obes Complic 1:568–579. https://doi.org/10.1111/j.1467-789X.2009.00703.x
Rolland Y, Lauwers-Cances V, Cristini C, Abellan van Kan G, Janssen I, Morley JEVB (2009) Difficulties with physical function associated with obesity, sarcopenia, and sarcopenic-obesity in community-dwelling elderly women: the EPIDOS (EPIDemiologie de l’ OSteoporose) Study 1–3. Am J Clin Nutr. https://doi.org/10.3945/ajcn.2008.26950.INTRODUCTION
Visser M, Goodpaster BH, Kritchevsky SB, Newman AB, Nevitt M, Rubin SM, Simonsick EM, Harris TB (2005) Muscle mass, muscle strength, and muscle fat infiltration as predictors of incident mobility limitations in well-functioning older persons. J Gerontol Ser A Biol Sci Med Sci 60:324–333
Visser M, Kritchevsky SB, Goodpaster BH, Newman AB, Nevitt M, Stamm E, Harris TB (2002) Leg muscle mass and composition in relation to lower extremity performance in men and women aged 70 to 79: the health, aging and body composition study. J Am Geriatr Soc 50:897–904
Beavers KM, Beavers DP, Houston DK, Harris TB, Hue TF, Koster A, Newman AB, Simonsick EM, Studenski SA, Nicklas BJ, Kritchevsky SB (2013) Associations between body composition and gait-speed decline: results from the health, aging, and body composition study. Am J Clin Nutr 1–4:552–560. https://doi.org/10.3945/ajcn.112.047860.INTRODUCTION
Verghese J, Holtzer R, Oh-park M, Derby CA, Lipton RB, Wang C (2011) Inflammatory markers and gait speed decline in older adults. J Gerontol Ser A Biomed Sci Med Sci. https://doi.org/10.1093/gerona/glr099
Lafortuna CL, Minocci A, Capodaglio P, Gondoni LA, Sartorio A, Vismara L, Rizzo G, Grugni G, Molecolare F (2014) Skeletal muscle characteristics and motor performance after 2-year growth hormone treatment in adults with Prader–Willi syndrome. J Gerontol Ser A Biomed Sci Med Sci 99:1816–1824
Murakami N, Obata K, Abe Y, Oto Y, Kido Y, Itabashi H, Tsuchiya T, Tanaka Y, Yoshino A, Nagai T (2012) Scoliosis in Prader–Willi syndrome: effect of growth hormone therapy and value of paravertebral muscle volume by CT in predicting scoliosis progression. Am J Med Genet Part A. https://doi.org/10.1002/ajmg.a.35429
Festen DAM, Van Wijngaarden RDL, Van Eekelen M, Otten BJ, Wit JM, Duivenvoorden HJ, Hokken-koelega ACS (2008) Randomized controlled GH trial: effects on anthropometry, body composition and body proportions in a large group of children with Prader–Willi syndrome. Clin Endocrinol. https://doi.org/10.1111/j.1365-2265.2008.03228.x
Acknowledgements
The authors would like to acknowledge Eng. Maria Gina Mastroianni for her valuable contribution.
Funding
Not applicable.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
There were no potential conflicts of interest.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. The study was approved by the Ethics Committees of the Istituto Auxologico Italiano, Ospedale San Giuseppe, Piancavallo (VB), Italy.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Cimolin, V., Cau, N., Galli, M. et al. Gait strategy and body composition in patients with Prader–Willi syndrome. Eat Weight Disord 26, 115–124 (2021). https://doi.org/10.1007/s40519-019-00825-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40519-019-00825-2