Abstract
Purpose
The purpose of this study was to determine the cut-off values of triglycerides and glucose (TyG) index as one of the indirect indices for metabolic syndrome (MetS) in a pediatric population.
Methods
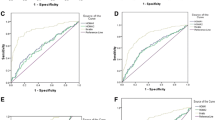
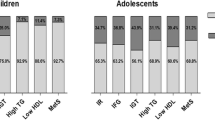
This national study was conducted in 2015 on 14400 students, aged 7–18 years. They were selected by random cluster sampling from 30 provinces of our country during the fifth survey of a national school-based surveillance program. MetS was defined based on the Adult Treatment Panel III (ATP III) criteria modified for the pediatric age group. The cut-off values of TyG index for MetS were obtained using the receiver operation characteristic (ROC) curve analysis by gender and age groups.
Results
Totally, 3843 students (52.3% boys) with mean (SD) age of 12.45 (3.04) years were assessed. The area under the ROC curve of TyG index for MetS was 0.83 in total participants. According to the ATP III criteria the cut-off values of the TyG index were 8.33 (8.21–8.45) in total students, 8.47 (8.36–8.58) in boys, and 8.33 (8.18–8.48) in girls. In the 7–12 and 13–18 years’ age groups, these values were 8.47 (8.32–8.63) and 8.34 (8.22–8.45) in total, 8.39 (8.26–8.52) and 8.47 (8.33–8.61) in boys, 8.33 (8.11–8.55) and 8.35 (8.22–8.47) in girls, respectively.
Conclusion
The findings of this study can be clinically helpful for screening MetS in children and adolescents but the effectiveness of these criteria needs to be evaluated by further longitudinal surveys.
Level of evidence
Level V, cross-sectional descriptive study (National surveillance study).

Similar content being viewed by others
References
Day C (2007) Metabolic syndrome, or what you will: definitions and epidemiology. Diabetes Vasc Dis Res 4:32–38. https://doi.org/10.3132/dvdr.2007.003
Morrison JA, Friedman LA, Wang P, Glueck CJ (2008) Metabolic syndrome in childhood predicts adult metabolic syndrome and type 2 diabetes mellitus 25 to 30 years later. J Pediatr 152:201–206. https://doi.org/10.1016/j.jpeds.2007.09.010
Ejtahed HS, Qorbani M, Motlagh ME, Angoorani P, Hasani-Ranjbar S, Ziaodini H et al (2017) Association of anthropometric indices with continuous metabolic syndrome in children and adolescents: the CASPIAN-V study. Eat Weight Disord. https://doi.org/10.1007/s40519-017-0455-0 (online)
Barbaro G, Piedimonte A, Podagrosi M, Mercurio R, Mosca A, D’Avanzo M et al (2016) Epicardial adipose tissue and signs of metabolic syndrome in children. Eat Weight Disord 21:269–286. https://doi.org/10.1007/s40519-015-0221-0
Bergman RN, Phillips LS, Cobelli C (1981) Physiologic evaluation of factors controlling glucose tolerance in man: measurement of insulin sensitivity and beta-cell glucose sensitivity from the response to intravenous glucose. J Clin Investig 68:1456–1467. https://doi.org/10.1172/JCI110398
Kelley DE, Goodpaster BH (2001) Skeletal muscle triglyceride. An aspect of regional adiposity and insulin resistance. Diabetes Care 24:933–941. https://doi.org/10.2337/diacare.24.5.933
Guerrero-Romero F, Simental-Mendia LE, Gonzalez-Ortiz M, Martinez-Abundis E, Ramos-Zavala MG, Hernandez-Gonzalez SO et al (2010) The product of triglycerides and glucose, a simple measure of insulin sensitivity. Comparison with the euglycemic–hyperinsulinemic clamp. J Clin Endocrinol Metab 95:3347–3351. https://doi.org/10.1210/jc.2010-0288
Kang B, Yang Y, Lee EY, Yang HK, Kim HS, Lim SY et al (2017) Triglycerides/glucose index is a useful surrogate marker of insulin resistance among adolescents. Int J Obes 41:789–792. https://doi.org/10.1038/ijo.2017.14
Motlagh ME, Ziaodini H, Qorbani M, Taheri M, Aminaei T, Goodarzi A et al (2017) Methodology and early findings of the fifth survey of childhood and adolescence surveillance and prevention of adult noncommunicable disease: the CASPIAN-V study. Int J Prev Med 8:4. https://doi.org/10.4103/2008-7802.198915
Organization WH (1995) Physical status: the use of and interpretation of anthropometry, Report of a WHO Expert Committee
Knowles K, Paiva L, Sanchez S, Revilla L, Lopez T, Yasuda M et al (2011) Waist circumference, body mass index, and other measures of adiposity in predicting cardiovascular disease risk factors among Peruvian adults. Int J Hypertens. https://doi.org/10.4061/2011/931402
Aswathappa J, Garg S, Kutty K, Shankar V (2013) Neck circumference as an anthropometric measure of obesity in diabetics. N Am J Med Sci 5:28. https://doi.org/10.4103/1947-2714.106188
Nyland J, Fried A, Maitra R, Johnson DL, Caborn DN (2006) Wrist circumference is related to patellar tendon thickness in healthy men and women. Clin Imaging 30:335–338. https://doi.org/10.1016/j.clinimag.2006.02.004
McNamara JR, Schaefer EJ (1987) Automated enzymatic standardized lipid analyses for plasma and lipoprotein fractions. Clin Chim Acta 166:1–8. https://doi.org/10.1016/0009-8981(87)90188-4
Zimmet P, Alberti G, Kaufman F, Tajima N, Silink M, Arslanian S et al (2007) The metabolic syndrome in children and adolescents. Lancet 369(9579):2059–2061. https://doi.org/10.1016/s0140-6736(07)60958-1
Du T, Yuan G, Zhang M, Zhou X, Sun X, Yu X (2014) Clinical usefulness of lipid ratios, visceral adiposity indicators, and the triglycerides and glucose index as risk markers of insulin resistance. Cardiovasc Diabetol 13:146. https://doi.org/10.1186/s12933-014-0146-3
Delavari A, Forouzanfar MH, Alikhani S, Sharifian A, Kelishadi R (2009) First nationwide study of the prevalence of the metabolic syndrome and optimal cutoff points of waist circumference in the Middle East. Diabetes Care 32:1092–1097. https://doi.org/10.2337/dc08-1800
Kelishadi R, Gouya MM, Adeli K, Ardalan G, Gheiratmand R, Majdzadeh R et al (2008) Factors associated with the metabolic syndrome in a national sample of youths: CASPIAN study. Nutr Metab Cardiovasc Dis 18:461–470. https://doi.org/10.1016/j.numecd.2007.02.014
Unger G, Benozzi SF, Perruzza F, Pennacchiotti GL (2014) Triglycerides and glucose index: a useful indicator of insulin resistance. Endocrinol Nutr 61:533–540. https://doi.org/10.1016/j.endonu.2014.06.009
Lee SH, Han K, Yang HK, Kim MK, Yoon KH, Kwon HS et al (2015) Identifying subgroups of obesity using the product of triglycerides and glucose: the Korea National Health and Nutrition Examination Survey, 2008–2010. Clin Endocrinol 82:213–220. https://doi.org/10.1111/cen.12502
Lee S-H, Kwon H-S, Park Y-M, Ha H-S, Jeong SH, Yang HK et al (2014) Predicting the development of diabetes using the product of triglycerides and glucose: the Chungju Metabolic Disease Cohort (CMC) study. PLoS One 9:e90430. https://doi.org/10.1371/journal.pone.0090430
Mohd Nor NS, Lee S, Bacha F, Tfayli H, Arslanian S (2016) Triglyceride glucose index as a surrogate measure of insulin sensitivity in obese adolescents with normoglycemia, prediabetes, and type 2 diabetes mellitus: comparison with the hyperinsulinemic–euglycemic clamp. Pediatr Diabetes 17:458–465. https://doi.org/10.1111/pedi.12303
Gayoso-Diz P, Otero-González A, Rodriguez-Alvarez MX, Gude F, García F, De Francisco A et al (2013) Insulin resistance (HOMA-IR) cut-off values and the metabolic syndrome in a general adult population: effect of gender and age: EPIRCE cross-sectional study. BMC Endocr Disord 13:47. https://doi.org/10.1186/1472-6823-13-47
Tomé M, Botana M, Cadarso-Suárez C, Rego-Iraeta A, Fernández-Mariño A, Mato J et al (2009) Prevalence of metabolic syndrome in Galicia (NW Spain) on four alternative definitions and association with insulin resistance. J Eendocrinol Investig 32:505. https://doi.org/10.1007/BF03346497
Esteghamati A, Ashraf H, Esteghamati A-R, Meysamie A, Khalilzadeh O, Nakhjavani M et al (2009) Optimal threshold of homeostasis model assessment for insulin resistance in an Iranian population: the implication of metabolic syndrome to detect insulin resistance. Diabetes Res Clin Pract 84:279–287. https://doi.org/10.1016/j.diabres.2009.03.005
Lee S, Choi S, Kim HJ, Chung Y-S, Lee KW, Lee HC et al (2006) Cutoff values of surrogate measures of insulin resistance for metabolic syndrome in Korean non-diabetic adults. J Korean Med Sci 21:695–700. https://doi.org/10.3346/jkms.2006.21.4.695
Kwon HC, Woo SI, Kim YK, Ahn SM, Song KE, Jung SH et al (2005) Cutoff values of surrogate measures of insulin resistance for metabolic syndrome in Korean non-diabetic adults. Korean J Obes 14:69–75. https://doi.org/10.3346/jkms.2006.21.4.695
Grzybowski M, Younger JG (1997) Statistical methodology: III. Receiver operating characteristic (ROC) curves. Acad Emerg Med 4:818–826
Faraggi D, Reiser B (2002) Estimation of the area under the ROC curve. Stat Med 21:3093–3106. https://doi.org/10.1002/sim.1228
Simental-Mendía LE, Rodríguez-Morán M, Guerrero-Romero F (2008) The product of fasting glucose and triglycerides as surrogate for identifying insulin resistance in apparently healthy subjects. Metab Syndr Relat Disord 6:299–304. https://doi.org/10.1089/met.2008.0034
Guerrero-Romero F, Simental-Mendía LE, González-Ortiz M, Martínez-Abundis E, Ramos-Zavala MG, Hernández-González SO et al (2010) The product of triglycerides and glucose, a simple measure of insulin sensitivity. Comparison with the euglycemic–hyperinsulinemic clamp. J Clin Endocrinol Metab 95:3347–3351. https://doi.org/10.1210/jc.2010-0288
Moon S, Park J-S, Ahn Y (2017) The cut-off values of triglycerides and glucose index for metabolic syndrome in American and Korean adolescents. J Korean Med Sci 32:427–433. https://doi.org/10.3346/jkms.2017.32.3.427
Kim JW, Park SH, Kim Y, Im M, Han H-S (2016) The cutoff values of indirect indices for measuring insulin resistance for metabolic syndrome in Korean children and adolescents. Ann Pediatr Endocrinol Metab 21:143–148. https://doi.org/10.6065/apem.2016.21.3.143
Vasques ACJ, Novaes FS, de Oliveira MdS, Souza JRM, Yamanaka A, Pareja JC et al (2011) TyG index performs better than HOMA in a Brazilian population: a hyperglycemic clamp validated study. Diabetes Res Clin Pract 93:e98–e100. https://doi.org/10.1016/j.diabres.2011.05.030
Mohd Nor NS, Lee S, Arslanian SA (2015) Triglyceride Glucose (TyG) Index As a surrogate measure of insulin sensitivity in obese adolescents. Nucl Pept Regul Glucose Metab Endocr Soc. https://doi.org/10.1111/pedi.12303
Rodríguez-Morán M, Simental-Mendía L, Guerrero-Romero F (2017) The triglyceride and glucose index is useful for recognising insulin resistance in children. Acta Paediatr 106:979–983. https://doi.org/10.1111/apa.13789
Acknowledgements
This study was supported by the Ministry of Health and Medical education, Ministry of Education and Training, Isfahan University of Medical Sciences, and Endocrinology and Metabolism Research Institute of Tehran University of Medical Sciences. We are indebted to the participating schools, families and students in the study for their cooperation.
Funding
This study was funded by the Ministry of Health and Medical education, Ministry of Education and Training, Isfahan University of Medical Sciences, and Endocrinology and Metabolism Research Institute of Tehran University of Medical Sciences (Grant no. 194049).
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Rights and permissions
About this article
Cite this article
Angoorani, P., Heshmat, R., Ejtahed, HS. et al. Validity of triglyceride–glucose index as an indicator for metabolic syndrome in children and adolescents: the CASPIAN-V study. Eat Weight Disord 23, 877–883 (2018). https://doi.org/10.1007/s40519-018-0488-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40519-018-0488-z