Abstract
Purpose of Review
The rapid spread of virus, severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), has turned out to be a global emergency. Symptoms of this viral infection, coronavirus disease 2019 (COVID-19), include mild infections of the upper respiratory tract, viral pneumonia, respiratory failure, multiple organ failure and death. Till date, no drugs have been discovered to treat COVID-19 patients, and therefore, a considerable amount of interest has been shown in repurposing the existing drugs.
Recent Findings
Out of these drugs, chloroquine (CQ) and hydroxychloroquine (HCQ) have demonstrated positive results indicating a potential antiviral role against SARS-CoV-2. Its mechanism of action (MOA) includes the interference in the endocytic pathway, blockade of sialic acid receptors, restriction of pH mediated spike (S) protein cleavage at the angiotensin-converting enzyme 2 (ACE2) binding site and prevention of cytokine storm. Unfortunately, its adverse effects like gastrointestinal complications, retinopathy and QT interval prolongation are evident in treated COVID-19 patients. Yet, multiple clinical trials have been employed in several countries to evaluate its ability in turning into a needed drug in this pandemic.
Summary
This review attempts to summarize the MOA of CQ/HCQ and its side effects. The existing literature hints that till date, the role of CQ/HCQ in COVID-19 may be sceptical, and further studies are warranted for obtaining a therapeutic option that could be effectively used across the world to rise out from this pandemic.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
What was then an unknown cause of respiratory ailments in the patients of Wuhan, China, the disease has now grown into a lethal threat to mankind in the form of a pandemic. The World Health Organization (WHO) had declared it as a public health emergency of international concern on 31 January 2020 [1]. Initially referred to as the 2019 novel coronavirus (2019 n-CoV) [2,3,4] and controversially the Wuhan virus [5,6,7], it was later officially named by WHO as the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) that is responsible for causing coronavirus disease 2019 (COVID-19) on 11 February 2020 [8].
The SARS-CoV-2 belongs to Betacoronavirus genera of the Coronaviridae family, which, along with the Alphacoronavirus, are known to infect mammals. In contrast, the remaining two members of the family, Gammacoronavirus and the Deltacoronavirus, infect avians [9]. They contain a positive strand of RNA with 29,903 nucleotides and 10 open reading frames where structural proteins like Spike (S) proteins, Nucleocapsid (N) proteins, Envelope (E) proteins and Membrane (M) proteins are coded by 3′ end, and polyproteins, namely, pp1a and pp1b, are coded by 5′ end [10]. The pp1a amd pp1b are cleaved into16 non-structural proteins (nsps) by two proteases namely papain like proteases and 3C like proteases [11]. The outer end of the virus structure inherits protruding spikes thus appearing like a crown-shaped virion [12••]. These spike glycoproteins are essential for the propagation of viruses into the human body through interactions with angiotensin-converting enzyme 2 (ACE2) to mediate viral pathogenicity [13].
SARS-CoV-2 is known to have an incubation period of about 2–14 days in humans [14]. It could transmit to individuals via respiratory droplets formed when symptomatic patients cough and sneeze [15]. Depending on the severity of infection, the infected individuals present symptoms including systemic disorders like dry cough, tiredness, headache, dyspnoea, lymphopenia and respiratory ailments like bilateral pneumonia, ground-glass opacity (GGO), sneezing and rhinorrhoea [16]. Certain patients are reported to have diarrhoea that could hint the effect of SARS-CoV-2 in the gastrointestinal tract and also increased transaminases and prothrombin times and reduced protein levels in blood indicating hepatic injury [17]. Severe cases in SARS-CoV-2 affected geriatric population showed acute respiratory distress syndrome (ARDS) that leads to septic shock. Computed tomography scans (CT scans) showed larger and denser lesions with prominent damage to the lungs [18]. Respiratory failure, cardiogenic shock and other multiple organ failures have been attributed to the deaths of infected patients [19]. Interestingly, it was seen that females were less susceptible to COVID-19 due to oestrogen that played an essential role in immunity [20]. The WHO has reported more than 2.5 lakh deaths and more than 3.5 million confirmed cases across the globe till date, and the development of effective therapeutics are need of the hour [21].
Currently, there are no specific treatments available for COVID-19 [22•]. With the clocks ticking and the fast-spreading nature of COVID-19, looking out for therapies through the repurposing of available drugs could be a quicker alternative. The antimalarial drugs chloroquine (CQ) and hydroxychloroquine (HCQ) have shown promising potential in clinical setups to combat COVID-19. Looking at the possibility of CQ/HCQ, in silico studies have been employed with molecules having scaffold similar to CQ [23] and repurposing of CQ for evaluating its effectiveness [24•]. HCQ is preferred due to its higher water solubility, lower toxicity and also feasibility for prolonged use with increased tolerance [25, 26]. HCQ is speculated to provide better treatment outcomes than CQ [27]. These drugs have shown interference in the endocytic pathway, blockade of sialic acid receptors, restriction of pH mediated S protein cleavage at the ACE2 binding site and prevention of cytokine storm. With these actions, they also have shown adverse events like gastrointestinal problems, retinopathy and QT prolongation. Having said this, the quick search for the COVID-19 therapy has pushed CQ/HCQ into the rapid deployment of its clinical trials to evaluate the safety and effectiveness. Given the fact that morbidity and mortality due to COVID-19 increase exponentially, there is a need to explore the evidence from the clinical trials. Thus, the present review describes the MOA, side effects and various clinical trials undergoing across the world using HCQ to target COVID-19.
Inhibitory Effects of CQ and HCQ on the Potential Sites of SARS-CoV-2 Entry and Pathophysiology in Host Cells
CQ obtained from the bark of Cinchona trees has been widely used for a long time as an antimalarial agent [28]. In recent times, its hydroxyl derivative, HCQ, has proven to be safer than CQ due to the decreased renal and ocular toxicity and is being used as a substitute for CQ [29]. CQ/HCQ has shown its potential to destroy SARS-CoV-2 in the following ways.
Inhibition Through Interference in the Endocytic Pathway
SARS-CoV-2 facilitates their entry into the host cells through different ways via endocytic pathways. The nasal epithelium expresses dynamin, a GTPase that is essential for endocytosis mediated through clathrin-layered vesicles. Pneumocytes express CtBP1&2 and Pak1 proteins which are essential in micropinocytosis that forms an essential mediator in the pneumocyte endocytic pathway [30••]. CQ gathers in the endosomes and lysosomes and leads to pH neutralization that leads to hindrance on the effects of proteases, thus preventing S protein cleavage and, ultimately, the process of viral access into a host organism [31]. CQ inhibits fusion of lysosomes with autophagosomes due to dysregulation of syntaxin 17 (STX17) as shown in Fig. 1. Further, it hampers Golgi functioning and blocks transportation of material into lysosomes [32••]. HCQ also prevents the movement of SARS-CoV-2 from early endosomes to early lysosomes that are important for viral genome release [33••] as shown in Fig. 1. The rise in pH of lysosomes and endosomes mediated by HCQ further leads to formation of autophagosomes that break the S protein preventing the membrane fusion [34].
Inhibition Through Blockade of Sialic Acid Receptors
Recently, it has been identified that the N terminal of S protein in SARS-CoV-2 is similar to the region where sialic acid receptor binding occurs in MERS-CoV [35]. Therefore, SARS-CoV-2 may mediate its entry via these sialic acid receptors in the upper respiratory pathway and the previously known ACE2 receptor. Another study has also identified a novel binding site for the binding of gangliosides in the SARS-CoV-2 S protein N-terminal domain (NTD). Both CQ/HCQ were efficient in inhibiting the sialic acids, especialy the 9-O-SIA variant, however HCQ showed a better potency [36••]. The SARS-CoV-2 is also speculated to enter through binding with α 2–6-linkage and α 2–3-linkage sialic acid receptors. The 2–6-linkage is highly expressed in the epithelia of the conjunctiva and cornea, whereas the nasolacrimal region possesses both these receptors [37]. Therefore, the incident entry of viral particles into the eye or the respiratory passage via duct of nasolacrimal system may lead to its successful entry into the host cells.
Inhibition Through Restriction of pH Mediated S Protein Cleavage at the ACE2 Binding Site
The S proteins mediate the association and entry of viral particles in host cells [38]. It has two components, namely, the S1 subunit and S2 subunit [39•]. The S1 subunit is responsible for mediating entry into the host cells through attachment at the ACE2 receptor. Following this, the cellular proteases like transmembrane serine protease II (TMPRSS2) facilitate the S priming, which leads to cleavage of S1/S2 and S2’. Interestingly, it was reported that splice alterations occurring in the genome of TMPRSS2 due to single-nucleotide polymorphism could alter its expression levels, thus affecting rate of SARS-CoV-2 infection in patients [40]. Upon cleavage of the S2 domain, it releases fusion peptide [41]. This allows the viral membrane to fuse with the cellular membrane promoted by S2 subunit [42••]. A recent in silico study reported that SARS-CoV-2 spikes bound with a higher affinity to a truncated ACE2 as compared with full-length ACE2. This truncated ACE2 possessed the same conserved N-terminal region as that of full-length ACE2 [43]. Another study reported the critical amino acid residues that are responsible for enhanced affinity of spike binding to ACE2 [44•]. The ACE2 undergoes glycosylation for it to convert to an active form. Therefore, when SARS-CoV-2 S protein binds to it, the ACE2 receptor undergoes glycosylation and gets activated. In this case, CQ/HCQ plays an essential role where it prevents the glycosylation of ACE2 receptors, thus preventing entry of SARS-CoV-2 into the host organisms [45••] as shown in Fig. 1.
Inhibition Through Prevention of Cytokine Storm
Recently, a striking feature was observed in severely ill patients in China whose plasma profiles showed elevated levels of cytokines [2]. Therefore, it would not be wrong to associate such an increase in levels of cytokines, termed as a cytokine storm, to grade how severe the disease is progressing. In the antigen-presenting cells (APC), HCQ inhibits the antigen processing and presentation of autoantigen mediated by the major histocompatibility complex (MHC) class II to T cells. Due to this, the levels of activated T cells decline, causing a reduction in the production of cytokines generated by T cells and the B cells [46, 47]. The changes in pH caused by HCQ also affects the toll-like receptor (TLR) functioning. Synergistically, HCQ can also associate with nucleic acids to block TLR9 binding and RNA facilitated activation of TLR 7 processing, therefore, reducing the production of cytokines [48], as shown in Fig. 2. The cyclic GMP-AMP (cGAMP) synthase (cGAS) upon binding to DNA leads to the formation of cGAMP. This cGAMP upon associating with stimulator of interferon gene protein (STING) leads to the generation of interferon 1 (IFN I) via the interferon regulatory transcription factor (IRF). HCQ inhibits the DNA binding at cGAS, thus preventing cytokine production and ultimately controlling cytokine storm [49] as shown in Fig. 3.
Side Effects of CQ/HCQ
The use of CQ/HCQ in COVID-19 patients has been owed to its immunomodulatory and antiviral properties but unfortunately still lacks the proof of their effectiveness. The use of HCQ does come with a set of adverse effects that cannot be waved off. The most commonly seen side effects of CQ/HCQ are gastrointestinal (GI) upset along with nausea and vomiting [50, 51]. GI symptoms basically include dyspepsia, dysgeusia, abdominal cramps, etc. Along with these, cases of rashes, itching, headaches and even tinnitus have been surfaced [52]. The severe side effects of CQ/HCQ include retinopathy [53, 54] and QT interval prolongation [55,56,57]. In the epithelia of the retinal pigment, the lysosomal deterioration of outer components of the photoreceptor by CQ/HCQ leads to retinal toxicity [58]. Ocular pigmentation could be possibly due to binding of these drugs to melanin that could damage ciliary bodies along with the cornea and the retina as well [59]. The use of CQ/HCQ has also been linked to pigmentation in patients, especially skin, ear and nose cartilage, trachea and joint tissue [60]. Conditions like eruptive toxic epidermal necrolysis, acute generalized exanthematous pustulosis, erythema multiforme and toxic epidermal necrolysis are seen in CQ/HCQ patients [61]. Cutaneous eruptions observed could be due to an imbalance in the immune system in CQ/HCQ-treated patients [62]. A summary of CQ/HCQ side effects is shown in Fig. 4.
Clinical trials using HCQ as a treatment for COVID-19
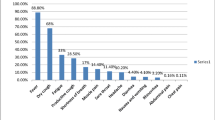
Currently, a total of about 242 studies have been registered under clinicaltrial.gov that involve HCQ either as a single regimen or a combination regimen with other drugs. Approximately about 70 studies have not yet started recruiting subjects. A total of 18 studies are fully active but not yet recruiting, while 107 studies are recruiting the required subjects. Out of the 107 studies, 96 studies are of interventional design, while 11 are observational in nature. Some studies employ only HCQ (NCT04340544, NCT04351620, NCT04466540, NCT04435808), while some compare the efficacy of HCQ with other interventions like azithromycin (NCT04334382), ivermectin (NCT04391127), tocilizumab (NCT04332094) and favipiravir (NCT04411433). Further, a combination of drugs with HCQ is also included like HCQ + favipiravir (NCT04392973) and HCQ + azithromycin (NCT04336332). A total of 19 studies have been completed out of which one involves the use of convalescent plasma (NCT04441424). These studies have been mainly focused on the safety and efficacy of HCQ (NCT04321278), (NCT04261517) and (NCT04358068). It is worth noting that 14 studies have either been terminated or suspended. Few studies like NCT04323631, NCT04371926 and NCT04347512 were withdrawn mainly due to a rise in concerns of HCQ adverse events and on the advice of health authorities.
Conflicting Reports of the Use of CQ/HCQ in Management of COVID-19
HCQ is looked upon as the wonder drug or miracle drug that showed antiviral property to aid in management of COVID-19 patients. CQ reduces fever and lung lesions and prolongs the progression of the disease, while HCQ in combination with azithromycin can reduce viral load in COVID-19 patients [63••]. Azithromycin enhances the capacity of HCQ in lowering viral load [63••]. CQ also reduces pneumonia exacerbations and duration of symptoms [64]. Even though the MOA of CQ and HCQ is the same, HCQ is more effective over CQ [65]. Nevertheless, contradictory data has also been published on HCQ that discourages its use as a potential therapeutic candidate in COVID-19 primarily owed to its multiple side effects as mentioned before in this article. HCQ also failed to show a beneficial result in an observational study [66]. Another report also claims that HCQ was not able to manage even mild cases of COVID-19 [67].
NIH and WHO Verdict on the Usage of HCQ for treating COVID-19
In India, the Indian Council of Medical Research (ICMR) has approved the use of HCQ for prophylaxis of COVID-19 in asymptomatic healthcare workers and asymptomatic household contacts of confirmed cases [68]. Later, ICMR issued another advisory that permitted use of HCQ even for asymptomatic frontline non-healthcare workers [69], even though the US FDA has cautioned against the use of HCQ in COVID-19 patients owing to its side effects [70].
Similarly, the National Institute of Health (NIH) recently put a check on a study involving the efficacy of HCQ in COVID-19 patients with a note that even though it does not cause any harm, it did not provide additional benefits either [71]. These views bring a lot of conflicts that bring us to a position where we are still unable to conclude whether HCQ could be the game changer for COVID-19. As every coin has two sides, it becomes essential for us to understand both aspects of this drug. NIH conducted a study through the National Heart, Lung and Blood Institute to ascertain the effect of HCQ as compared with control hypothesizing beneficial role of HCQ (NCT04332991) in improving clinical conditions of patients in 15 days. It was a multicentre, blinded, placebo-controlled, randomized clinical trial. It had about 479 participants with a parallel assignment of two interventions, namely, HCQ 400 mg twice daily on day 1 followed by HCQ 200 mg on days 2–5 oral and placebo twice daily for 5 days. Primarily death, hospitalization on invasive mechanical ventilation and non-invasive ventilation were assessed. Ultimately due to the absence of any benefits for COVID-19 patients, NIH decided to stop the study.
Similarly, the WHO had set up a solidarity trial for finding an effective therapy for COVID-19 using HCQ and lopinavir/ritonavir drug interventions. It was concluded that very less or almost no reduction in death rates of COVID-19 patients were seen due to which it was stopped. Interestingly, it was also concluded that other studies involving HCQ could be continued, while this check was only applicable to the solidarity trial using HCQ [72].
Conclusion
The COVID-19 pandemic has quickly grown to become one of the biggest threats that mankind has faced since the Influenza outbreak in the last century and is now being regarded as a ‘global healthcare emergency’. As the pandemic has grown stronger, it has called for quick and effective therapies where-in the role of efficient clinical trials is crucial for the search of the ‘game changer’ in therapeutics of COVID-19. As we have seen how CQ/HCQ can interfere in endocytic pathway, prevent ACE2 glycosylation, promote blockade of sialic acid receptors and reduce cytokine storm, this could have been attributed to its promising preliminary results in managing the viral symptoms. But it is seen that even though it is weighed down by its adverse effects like gastrointestinal indications, QT prolongation and retinopathy, it has been extensively employed in clinical trials across the globe. Results from a lot of recently initiated studies in some countries have shown positive outcome measures; however, the data is still not conclusive enough to establish this drug as the first-line therapy for treating/preventing COVID-19 infection, and more definitive results are still awaited.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
World Health Organization. Coronavirus disease 2019 (COVID-19) situation report – 11. Published 2020. Accessed May 6, 2020. https://www.who.int/docs/default-source/coronaviruse/situation-reports/20200131-sitrep-11-ncov.pdf?sfvrsn=de7c0f7_4
Huang C, Wang Y, Li X, Ren L, Zhao J, Hu Y, et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet. 2020;395:497–506. https://doi.org/10.1016/S0140-6736(20)30183-5.
Wax RS, Christian MD. Practical recommendations for critical care and anesthesiology teams caring for novel coronavirus (2019-nCoV) patients. Can J Anesth. 2020;67:568–76. https://doi.org/10.1007/s12630-020-01591-x.
Han Q, Lin Q, Jin S, You L. Coronavirus 2019-nCoV: a brief perspective from the front line. J Inf Secur. 2020;80:373–7. https://doi.org/10.1016/j.jinf.2020.02.010.
Liu SL, Saif L. Emerging viruses without borders: the Wuhan coronavirus. Viruses. 2020;12:E130. https://doi.org/10.3390/v12020130.
Riou J, Althaus CL. Pattern of early human-to-human transmission of Wuhan 2019 novel coronavirus (2019-nCoV), December 2019 to January 2020. Eurosurveillance. 2020;25:1–5. https://doi.org/10.2807/1560-7917.ES.2020.25.4.2000058.
Ralph R, Lew J, Zeng T, Francis M, Xue B, Roux M, et al. 2019-nCoV (Wuhan virus), a novel coronavirus: human-to-human transmission, travel-related cases, and vaccine readiness. J Infect Dev Ctries. 2020;14:3–17. https://doi.org/10.3855/jidc.12425.
Gorbalenya AE, Baker SC, Baric RS, de Groot RJ, Drosten C, Gulyaeva AA, et al. The species severe acute respiratory syndrome-related coronavirus: classifying 2019-nCoV and naming it SARS-CoV-2. Nat Microbiol. 2020;5:536–44. https://doi.org/10.1038/s41564-020-0695-z.
Guo Y-R, Cao Q-D, Hong Z-S, Tan Y-Y, Chen S-D, Jin H-J, et al. The origin, transmission and clinical therapies on coronavirus disease 2019 (COVID-19) outbreak - an update on the status. Mil Med Res. 2020;7:11. https://doi.org/10.1186/s40779-020-00240-0.
Khan SA, Zia K, Ashraf S, Uddin R, Ul-Haq Z. Identification of chymotrypsin-like protease inhibitors of SARS-CoV-2 via integrated computational approach. J Biomol Struct Dyn Published online. 2020:1–10. https://doi.org/10.1080/07391102.2020.1751298.
Lobo-Galo N, Terrazas-López M, Martínez-Martínez A, Díaz-Sánchez ÁG. FDA-approved thiol-reacting drugs that potentially bind into the SARS-CoV-2 main protease, essential for viral replication. J Biomol Struct Dyn Published online. 2020:1–9. https://doi.org/10.1080/07391102.2020.1764393.
•• Ashour HM, Elkhatib WF, Rahman MM, Elshabrawy HA. Insights into the recent 2019 novel coronavirus (Sars-coV-2) in light of past human coronavirus outbreaks. Pathogens. 2020;9:1–15. https://doi.org/10.3390/pathogens9030186Explains the interaction of SARS-Cov-2 with host cells giving special emphasis on genome organisation and structure.
Kai H, Kai M. Interactions of coronaviruses with ACE2, angiotensin II, and RAS inhibitors—lessons from available evidence and insights into COVID-19. Hypertens Res Published online. 2020;43:1–7. https://doi.org/10.1038/s41440-020-0455-8.
Prajapati S, Sharma M, Kumar A, Gupta P, Narasimha Kumar GV. An update on novel COVID-19 pandemic: a battle between humans and virus. Eur Rev Med Pharmacol Sci. 2020;24:5819–29. https://doi.org/10.26355/eurrev_202005_21377.
Wan DY, Luo XY, Dong W, Zhang ZW. Current practice and potential strategy in diagnosing COVID-19. Eur Rev Med Pharmacol Sci. 2020;24:4548–53. https://doi.org/10.26355/eurrev_202004_21039.
Law S, Leung AW, Xu C. Severe acute respiratory syndrome (SARS) and coronavirus disease-2019 (COVID-19): from causes to preventions in Hong Kong. Int J Infect Dis. 2020;94:156–63. https://doi.org/10.1016/j.ijid.2020.03.059.
Kotfis K, Skonieczna-Żydecka K. COVID-19: gastrointestinal symptoms and potential sources of 2019-nCoV transmission. Anesthesiol Intensive Ther. 2020;52:1–2. https://doi.org/10.1056/NEJ.
Li Y, Peng S, Li L, Wang Q, Ping W, Zhang N, et al. Clinical and transmission characteristics of COVID-19 – a retrospective study of 25 cases from a single thoracic surgery department. Curr Med Sci. 2020;40:295–300. https://doi.org/10.1007/s11596-020-2176-2 Current Medical Science 40(2):2020 40(2):295–300,2020.
Vincent JL, Taccone FS. Understanding pathways to death in patients with COVID-19. Lancet Respir Med. 2020;8:430–2. https://doi.org/10.1016/S2213-2600(20)30165-X.
Xu P, Sun GD, Li ZZ. Clinical characteristics of two human-to-human transmitted coronaviruses: corona virus disease 2019 vs. Middle East respiratory syndrome coronavirus. Eur Rev Med Pharmacol Sci. 2020;24:5797–809. https://doi.org/10.26355/eurrev_202005_21374.
World Health Organization. Coronavirus disease (COVID-19) situation report-108. https://doi.org/10.1001/jama.2020.2633
• Keni R, Alexander A, Nayak PG, Mudgal J, Nandakumar K. COVID-19: emergence, spread, possible treatments, and global burden. Front Public Heal. 2020;8:216. https://doi.org/10.3389/FPUBH.2020.00216This paper explains the possible treatments available against COVID-19.
Beura S, Prabhakar C. In-silico strategies for probing chloroquine based inhibitors against SARS-CoV-2. J Biomol Struct Dyn Published online. 2020:1–25. https://doi.org/10.1080/07391102.2020.1772111.
• Adeoye AO, Oso BJ, Olaoye IF, Tijjani H, Adebayo AI. Repurposing of chloroquine and some clinically approved antiviral drugs as effective therapeutics to prevent cellular entry and replication of coronavirus. J Biomol Struct Dyn Published online 15 May 2020: 1-11. https://doi.org/10.1080/07391102.2020.1765876. This is a docking study which investigated the inhibitory potential of several drugs including chloroquine.
Devaux CA, Rolain JM, Colson P, Raoult D. New insights on the antiviral effects of chloroquine against coronavirus: what to expect for COVID-19? Int J Antimicrob Agents. 2020;55:19–20. https://doi.org/10.1016/j.ijantimicag.2020.105938.
Sahraei Z, Shabani M, Shokouhi S, Saffaei A. Aminoquinolines against coronavirus disease 2019 (COVID-19): chloroquine or hydroxychloroquine. Int J Antimicrob Agents. 2020;55:1–3. https://doi.org/10.1016/j.ijantimicag.2020.105945.
Gevers S, Kwa MSG, Wijnans E, van Nieuwkoop C. Safety considerations for chloroquine and hydroxychloroquine in the treatment of COVID-19. Clin Microbiol Infect Published online. 2020:4539–47. https://doi.org/10.1016/j.cmi.2020.05.006.
Abolghasemi E, Moosa-Kazemi SH, Davoudi M, Reisi A, Satvat MT. Comparative study of chloroquine and quinine on malaria rodents and their effects on the mouse testis. Asian Pac J Trop Biomed. 2012;2:311–4. https://doi.org/10.1016/S2221-1691(12)60030-6.
Sinha N, Balayla G. Hydroxychloroquine and covid-19. Postgrad Med J Published online. 2020:1–6. https://doi.org/10.1136/postgradmedj-2020-137785.
•• Glebov O. Understanding the cell biology of SARS-CoV-2 endocytosis for COVID-19 drug repurposing : looking beyond chloroquine. OSF Prepr Published online 2020. https://doi.org/10.31219/osf.io/xhz29. Article explains the evidences for interaction of chloroquine in endocytic pathway.
Yang N, Shen HM. Targeting the endocytic pathway and autophagy process as a novel therapeutic strategy in COVID-19. Int J Biol Sci. 2020;16:1724–31. https://doi.org/10.7150/ijbs.45498.
•• Mauthe M, Orhon I, Rocchi C, Zhou X, Luhr M, Hijlkema KJ, et al. Chloroquine inhibits autophagic flux by decreasing autophagosome-lysosome fusion. Autophagy. 2018;14:1435–55. https://doi.org/10.1080/15548627.2018.1474314Studies in cell lines and mice to explain the effect of CQ in autophagy. Further, it explains the several cellular changes caused by CQ.
•• Liu J, Cao R, Xu M, Wang X, Zhang H, Hu H, et al. Hydroxychloroquine, a less toxic derivative of chloroquine, is effective in inhibiting SARS-CoV-2 infection in vitro. Cell Discov. 2020;6:6–9. https://doi.org/10.1038/s41421-020-0156-0Evaluated the effectiveness of less toxic derivative of chloroquine, HCQ against SARS-CoV-2.
Singh AK, Singh A, Shaikh A, Singh R, Misra A. Chloroquine and hydroxychloroquine in the treatment of COVID-19 with or without diabetes: a systematic search and a narrative review with a special reference to India and other developing countries. Diabetes Metab Syndr Clin Res Rev. 2020;14:241–6. https://doi.org/10.1016/j.dsx.2020.03.011 Systematic review.
Milanetti E, Miotto M, Di Rienzo L, Monti M, Gosti G, Ruocco G. In-silico evidence for two receptors based strategy of SARS-CoV-2. bioRxiv Prepr Published online 2020: 1–10. https://doi.org/10.1101/2020.03.24.006197.
•• Fantini J, Di Scala C, Chahinian H, Yahi N. Structural and molecular modelling studies reveal a new mechanism of action of chloroquine and hydroxychloroquine against SARS-CoV-2 infection. Int J Antimicrob Agents Published online. 2020:1–8. https://doi.org/10.1016/j.ijantimicag.2020.105960Evaluates novel mechanism supporting the use of HCQ in COVID-19.
de Gonzague DML, Rabetafika DRRT, Rindra DR, Mihaja RN, Cyris DHJ, Léa PR. Beware of 2019-nCoV transmission through the ocular surface. EC Opthalmology Spec Issue. 2020:1–4 https://www.ecronicon.com/ecop/si/ECOP-02-SI-0014.pdf.
Shereen MA, Khan S, Kazmi A, Bashir N, Siddique R. COVID-19 infection: origin, transmission, and characteristics of human coronaviruses. J Adv Res. 2020;24:91–8. https://doi.org/10.1016/j.jare.2020.03.005.
• Satarker S, Nampoothiri M. Structural proteins in severe acute respiratory syndrome coronavirus-2. Arch Med Res Published online. 2020. https://doi.org/10.1016/j.arcmed.2020.05.012Describes how structural proteins of SARS-CoV-2 are organised and its interaction with host cell.
Paniri A, Hosseini MM, Akhavan-Niaki H. First comprehensive computational analysis of functional consequences of TMPRSS2 SNPs in susceptibility to SARS-CoV-2 among different populations. J Biomol Struct Dyn Published online. 2020:1–18. https://doi.org/10.1080/07391102.2020.1767690.
Boopathi S, Poma AB, Kolandaivel P. Novel 2019 coronavirus structure, mechanism of action, antiviral drug promises and rule out against its treatment. J Biomol Struct Dyn Published online. 2020:1–14. https://doi.org/10.1080/07391102.2020.1758788.
•• Hoffmann M, Kleine-Weber H, Schroeder S, Krüger N, Herrler T, Erichsen S, et al. SARS-CoV-2 cell entry depends on ACE2 and TMPRSS2 and is blocked by a clinically proven protease inhibitor. Cell. 2020;181:271–280.e8. https://doi.org/10.1016/j.cell.2020.02.052This study explains that entry of SARS-CoV-2 to the host cell is mediated through ACE2 receptor and also shows the importance of TMPRSS2.
Basit A, Ali T, Rehman SU. Truncated human angiotensin converting enzyme 2; a potential inhibitor of SARS-CoV-2 spike glycoprotein and potent COVID-19 therapeutic agent. J Biomol Struct Dyn Published online. 2020:1–17. https://doi.org/10.1080/07391102.2020.1768150.
• Veeramachaneni GK, Thunuguntla VBSC, JR B, Bondili JS. Structural and simulation analysis of hot spot residues interactions of SARS-CoV 2 with human ACE2 receptor. J Biomol Struct Dyn Published online. 2020:1–16. https://doi.org/10.1080/07391102.2020.1773318Simulation studies explaining the molecular interaction of SARS-CoV 2 with ACE2 receptor.
•• Pahan P, Pahan K. Smooth or risky revisit of an old malaria drug for COVID-19? J Neuroimmune Pharmacol 2020; 19. https://doi.org/10.1007/s11481-020-09923-w. Discuss why we should take caution in the usage of HCQ..
Zhou D, Dai SM, Tong Q. COVID-19: a recommendation to examine the effect of hydroxychloroquine in preventing infection and progression. J Antimicrob Chemother. 2020;75:4–7. https://doi.org/10.1093/jac/dkaa114.
Sahu P, Mudgal J, Arora D, Kinra M, Mallik SB, Rao CM, et al. Cannabinoid receptor 2 activation mitigates lipopolysaccharide-induced neuroinflammation and sickness behavior in mice. Psychopharmacol. 2019;236(6):1829–38.
Schrezenmeier E, Dörner T. Mechanisms of action of hydroxychloroquine and chloroquine: implications for rheumatology. Nat Rev Rheumatol. 2020;16:155–66. https://doi.org/10.1038/s41584-020-0372-x.
An J, Woodward JJ, Lai W, Minie M, Sun X, Tanaka L, et al. Inhibition of cyclic GMP-AMP synthase using a novel antimalarial drug derivative in Trex1-deficient mice. Arthritis Rheumatol. 2018;70:1807–19. https://doi.org/10.1002/art.40559.
Meyerowitz EA, Vannier AGL, Friesen MGN, Schoenfeld S, Gelfand JA, Callahan MV, et al. Rethinking the role of hydroxychloroquine in the treatment of COVID-19. FASEB J. 2020;34:6027–37. https://doi.org/10.1096/fj.202000919.
Pastick KA, Okafor EC, Wang F, Lofgren SM, Skipper CP, Nicol MR, et al. Review: hydroxychloroquine and chloroquine for treatment of SARS-CoV-2 (COVID-19). Open Forum Infect Dis. 2020;7:1–9. https://doi.org/10.1093/ofid/ofaa130.
Srinivasa A, Tosounidou S, Gordon C. Increased incidence of gastrointestinal side effects in patients taking hydroxychloroquine: a brand-related issue? J Rheumatol. 2017;44:368–39398. https://doi.org/10.3899/jrheum.161063.
Yusuf IH, Sharma S, Luqmani R, Downes SM. Hydroxychloroquine retinopathy. Eye. 2017;31:828–45. https://doi.org/10.1038/eye.2016.298.
Melles RB, Marmor MF. The risk of toxic retinopathy in patients on long-term hydroxychloroquine therapy. JAMA Ophthalmol. 2014;132:1453–60. https://doi.org/10.1001/jamaophthalmol.2014.3459.
•• Jankelson L, Karam G, Becker ML, Chinitz LA, Tsai M-C. QT prolongation, torsades de pointes, and sudden death with short courses of chloroquine or hydroxychloroquine as used in COVID-19: a systematic review. Hear Rhythm. 2020:1–8. https://doi.org/10.1016/j.hrthm.2020.05.008Systematic review points out the arrhythmogenic potential of HCQ in COVID-19 patients.
Sounderajah V, Ashrafian H, Aggarwal R, De Fauw J, Denniston AK, Greaves F, et al. Developing specific reporting guidelines for diagnostic accuracy studies assessing AI interventions: the STARD-AI steering group. Nat Med. 2020;26:1–2. https://doi.org/10.1038/s41591-020-0941-1.
O’Laughlin JP, Mehta PH, Wong BC. Life threatening severe QTc prolongation in patient with systemic lupus erythematosus due to hydroxychloroquine. Case Reports Cardiol. 2016;2016:1–4. https://doi.org/10.1155/2016/4626279.
Jorge A, Ung C, Young LH, Melles RB, Choi HK. Hydroxychloroquine retinopathy — implications of research advances for rheumatology care. Nat Rev Rheumatol. 2018;14:693–703. https://doi.org/10.1038/s41584-018-0111-8.
Hashem AM, Alghamdi BS, Algaissi AA, Alshehri FS, Bukhari A, Alfaleh MA, et al. Therapeutic use of chloroquine and hydroxychloroquine in COVID-19 and other viral infections: a narrative review. Travel Med Infect Dis. 2020;101735:101735. https://doi.org/10.1016/j.tmaid.2020.101735.
Jallouli M, Francès C, Piette JC, Huong DLT, Moguelet P, Factor C, et al. Hydroxychloroquine-induced pigmentation in patients with systemic lupus erythematosus a case-control study. JAMA Dermatology. 2013;149:935–40. https://doi.org/10.1001/jamadermatol.2013.709.
Abou Assalie N, Durcan R, Durcan L, Petri MA. Hydroxychloroquine-induced erythema multiforme. J Clin Rheumatol. 2017;23:127–8. https://doi.org/10.1097/RHU.0000000000000417.
Matsuda T, Ly NTM, Kambe N, Nguyen CTH, Ueda-Hayakawa I, Son Y, et al. Early cutaneous eruptions after oral hydroxychloroquine in a lupus erythematosus patient: a case report and review of the published work. J Dermatol. 2018;45:344–8. https://doi.org/10.1111/1346-8138.14156.
•• Gautret P, Lagier J-C, Parola P, Hoang VT, Meddeb L, Mailhe M, et al. Hydroxychloroquine and azithromycin as a treatment of COVID-19: results of an open-label non-randomized clinical trial. Int J Antimicrob Agents. 2020;(January):105949. https://doi.org/10.1016/j.ijantimicag.2020.105949Clinical trial favouring use of HCQ with azithromycin in COVID-19 patients.
Colson P, Rolain JM, Lagier JC, Brouqui P, Raoult D. Chloroquine and hydroxychloroquine as available weapons to fight COVID-19. Int J Antimicrob Agents. 2020;55:1–3. https://doi.org/10.1016/j.ijantimicag.2020.105932.
Sinha N, Balayla G. Hydroxychloroquine and covid-19. Postgrad Med J. 2020:1–6. https://doi.org/10.1136/postgradmedj-2020-137785.
Geleris J, Sun Y, Platt J, Zucker J, Baldwin M, Hripcsak G, et al. Observational study of hydroxychloroquine in hospitalized patients with COVID-19. N Engl J Med. 2020;382(25):2411–8. https://doi.org/10.1056/NEJMoa2012410.
Skipper CP, Pastick KA, Engen NW, Bangdiwala AS, Abassi M, Lofgren SM, et al. Hydroxychloroquine in nonhospitalized adults with early COVID-19. Ann Intern Med. 2020:M20–4207. https://doi.org/10.7326/M20-4207. Accessed 22 July 2020.
ICMR Advisory COVID-19. 2020; 1–4. https://www.mohfw.gov.in/pdf/AdvisoryontheuseofHydroxychloroquinasprophylaxisforSARSCoV2infection.pdf. Accessed 22 July 2020.
Revised advisory on the use of hydroxychloroquine (HCQ) as prophylaxis for SARS-CoV-2 infection. 2020. https://www.icmr.gov.in/pdf/covid/techdoc/V5_Revised_advisory_on_the_use_of_HCQ_SARS_CoV2_infection.pdf. Accessed 22 July 2020.
FDA cautions against use of hydroxychloroquine or chloroquine for COVID-19 outside of the hospital setting or a clinical trial due to risk of heart rhythm problems. 2020: https://www.fda.gov/drugs/drug-safety-and-availability/fda-cautions-against-use-hydroxychloroquine-or-chloroquine-covid-19-outside-hospital-setting-o. Accessed 21 July 2020.
NIH halts clinical trial of hydroxychloroquine | National Institutes of Health (NIH). National Institutes of Health. 2020: https://www.nih.gov/news-events/news-releases/nih-halts-clinical-trial-hydroxychloroquine. Accessed 21 July 2020.
WHO discontinues hydroxychloroquine and lopinavir/ritonavir treatment arms for COVID-19. 2020 : https://www.who.int/news-room/detail/04-07-2020-who-discontinues-hydroxychloroquine-and-lopinavir-ritonavir-treatment-arms-for-covid-19. Accessed 21 July 2020.
Acknowledgements
We thank the Manipal Academy of Higher Education, Manipal, India.
Funding
Open access funding provided by Manipal Academy of Higher Education, Manipal.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they have no conflict of interests.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human and animal subjects performed by any of the author0073.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Covid-19
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Satarker, S., Ahuja, T., Banerjee, M. et al. Hydroxychloroquine in COVID-19: Potential Mechanism of Action Against SARS-CoV-2. Curr Pharmacol Rep 6, 203–211 (2020). https://doi.org/10.1007/s40495-020-00231-8
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40495-020-00231-8