Abstract
Purpose
The primary aim was to investigate if treatment guided by serial ultrasound of the inferior vena cava-collapsibility index (IVC-CI) and B-lines on lung ultrasound (LUS) could reduce mortality, readmissions, and length of stay (LOS) in acutely dyspneic patients admitted to a hospital, compared to standard monitoring. The secondary aim was to determine how the changes of B-lines and IVC-CI are correlated to vitals and symptoms.
Methods
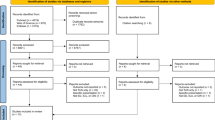
A systematic search was conducted on PubMed, Embase, Cochrane, Google Scholar, Web of Science, Scopus, OpenGrey, ProQuest, and databases for ongoing trials. The risk of bias was assessed according to study design.
Results
Of the 8258 studies identified, 50 were selected for full-text screening, and 24 studies were chosen for data extraction (19 pre–post-, two non-randomized controlled-, two randomized controlled-, and one retrospective cohort study), covering 2040 patients. Most studies were single-center and had small study populations with only heart failure patients. The risk of bias was high. No studies evaluated how the difference between two ultrasound measurements correlated with the primary outcomes. Seven studies reported that a decline in either B-lines or IVC size, or an increased IVC-CI reduced mortality, readmissions, and LOS when correlated to a single ultrasound measurement. All studies showed changes in the IVC-CI and B-lines, but these were not related to vitals or symptoms.
Conclusion
B-lines and IVC-CI are dynamic variables that change over time and with treatment. A single ultrasound measurement can influence prognostic outcomes, but it remains uncertain if repeated scans can have the same impact.
Graphical abstract




Similar content being viewed by others
Data availability
All data generated or analyzed during this study are included in this published article and its supplementary information files.
Code availability
Coding is available upon request.
References
Mockel M, Searle J, Muller R, Slagman A, Storchmann H, Oestereich P et al (2013) Chief complaints in medical emergencies: do they relate to underlying disease and outcome? The Charité Emergency Medicine Study (CHARITEM). Eur J Emerg Med 20:103–108. https://doi.org/10.1097/MEJ.0b013e328351e609
Kelly AM, Keijzers G, Klim S, Graham CA, Craig S, Kuan WS et al (2017) An observational study of dyspnea in emergency departments: the Asia, Australia, and New Zealand Dyspnea in Emergency Departments Study (AANZDEM). Acad Emerg Med 24:328–336. https://doi.org/10.1111/acem.13118
Lindskou TA, Pilgaard L, Søvsø MB, Kløjgård TA, Larsen TM, Jensen FB et al (2019) Symptom, diagnosis and mortality among respiratory emergency medical service patients. PLoS One. https://doi.org/10.1371/journal.pone.0213145
Ray P, Birolleau S, Lefort Y, Becquemin M-H, Beigelman C, Isnard R et al (2006) Acute respiratory failure in the elderly: etiology, emergency diagnosis and prognosis. Crit Care 10:R82. https://doi.org/10.1186/cc4926
Hayen A, Herigstad M, Pattinson KTS (2013) Understanding dyspnea as a complex individual experience. Maturitas 76:45–50. https://doi.org/10.1016/j.maturitas.2013.06.005
Oxberry SG, Bland JM, Clark AL, Cleland JGF, Johnson MJ (2012) Minimally clinically important difference in chronic breathlessness: Every little helps. Am Heart J 164:229–235. https://doi.org/10.1016/j.ahj.2012.05.003
Vicent L, Nuñez Olarte JM, Puente-Maestu L, Oliva A, López JC, Postigo A et al (2017) Degree of dyspnoea at admission and discharge in patients with heart failure and respiratory diseases. BMC Palliat Care. https://doi.org/10.1186/s12904-017-0208-x
Kelly N, Esteve R, Papadimos TJ, Sharpe RP, Keeney SA, DeQuevedo R et al (2015) Clinician-performed ultrasound in hemodynamic and cardiac assessment: a synopsis of current indications and limitations. Eur J Trauma Emerg Surg 41:469–480. https://doi.org/10.1007/s00068-014-0492-6
Gaskamp M, Blubaugh M, McCarthy LH, Scheid DC (2016) Can bedside ultrasound inferior vena cava measurements accurately diagnose congestive heart failure in the emergency department? A Clin-IQ. J Patient Centered Res Rev 3:230–234
Volpicelli G, Elbarbary M, Blaivas M, Lichtenstein DA, Mathis G, Kirkpatrick AW et al (2012) International evidence-based recommendations for point-of-care lung ultrasound. Intensive Care Med 38:577–591. https://doi.org/10.1007/s00134-012-2513-4
Asahi T, Nakata M, Higa N, Manita M, Tabata K, Shimabukuro M (2016) Respiratory collapse of the inferior vena cava reflects volume shift and subsequent fluid refill in acute heart failure syndrome. Circ J 80:1171–1177. https://doi.org/10.1253/circj.CJ-15-1374
Yavasi O, Unluer EE, Kayayurt K, Ekinci S, Saglam C, Surum N et al (2014) Monitoring the response to treatment of acute heart failure patients by ultrasonographic inferior vena cava collapsibility index. Am J Emerg Med 32:403–407. https://doi.org/10.1016/j.ajem.2013.12.046
Strnad M, Prosen G, Borovnik LV (2016) Bedside lung ultrasound for monitoring the effectiveness of prehospital treatment with continuous positive airway pressure in acute decompensated heart failure. Eur J Emerg Med 23:50–55. https://doi.org/10.1097/MEJ.0000000000000205
Via G, Storti E, Gulati G, Neri L, Mojoli F, Braschi A (2012) Lung ultrasound in the ICU: from diagnostic instrument to respiratory monitoring tool. Minerva Anestesiol 78:1282–1296
Spevack R, Al Shukairi M, Jayaraman D, Dankoff J, Rudski L, Lipes J (2017) Serial lung and IVC ultrasound in the assessment of congestive heart failure. Crit Ultrasound J 9:1–7. https://doi.org/10.1186/s13089-017-0062-3
Tufanaru C, Munn Z, Aromataris E et al (2020) Chapter 3: systematic reviews of effectiveness. In: Aromataris E, Munn Z (eds) JBI manual for evidence synthesis. JBI. https://synthesismanual.jbi.global
Shamseer L, Moher D, Clarke M, Ghersi D, Liberati A, Petticrew M et al (2015) Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015: elaboration and explanation. BMJ 349:g7647. https://doi.org/10.1136/bmj.g7647
Moher D, Shamseer L, Clarke M, Ghersi D, Liberati A, Petticrew M et al (2015) Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015 statement. Syst Rev 4:1. https://doi.org/10.1186/2046-4053-4-1
Arvig MD, Laursen CB, Jacobsen N, Gæde PH, Lassen AT (2019) Effectiveness of serial focused ultrasound of the lungs and inferior vena cava for monitoring patients with acute dyspnea: a systematic review protocol. JBI Database Syst Rev Implement Rep 17:2317. https://doi.org/10.11124/JBISRIR-D-19-00027
Via G, Hussain A, Wells M, Reardon R, ElBarbary M, Noble VE et al (2014) International evidence-based recommendations for focused cardiac ultrasound. J Am Soc Echocardiogr 27(683):e1-683.e33. https://doi.org/10.1016/j.echo.2014.05.001
Schünemann H, Brożek J, Guyatt G et al (eds) (2013) GRADE handbook for grading quality of evidence and strength of recommendations. Updated October 2013. The GRADE Working Group. http://guidelinedevelopment.org/handbook
Chuen M, Lip GYH, MacFadyen RJ (2009) Performing repeated noninvasive bedside measures of volume response to intravenous furosemide in acute pulmonary edema: a feasibility assessment. Cardiovasc Ther 27:89–95. https://doi.org/10.1111/j.1755-5922.2009.00080.x
Cubo-Romano P, Torres-Macho J, Soni NJ, Reyes LF, Rodríguez-Almodóvar A, Fernández-Alonso JM et al (2016) Admission inferior vena cava measurements are associated with mortality after hospitalization for acute decompensated heart failure: IVC and Mortality in ADHF. J Hosp Med 11:778–784. https://doi.org/10.1002/jhm.2620
Fawzi S, Rafla SM, El Atroush H, Farouk K, Wilson C (2012) Clinical significance of inferior vena cava index in monitoring patients in acute exacerbation of chronic heart failure. Eur Heart J Cardiovasc Imaging. https://doi.org/10.1093/ehjci/jes264
Goonewardena SN, Gemignani A, Ronan A, Vasaiwala S, Blair J, Brennan JM et al (2008) Comparison of hand-carried ultrasound assessment of the inferior vena cava and N-terminal pro-brain natriuretic peptide for predicting readmission after hospitalization for acute decompensated heart failure. JACC Cardiovasc Imaging 1:595–601. https://doi.org/10.1016/j.jcmg.2008.06.005
Guiotto G, Masarone M, Paladino F, Ruggiero E, Scott S, Verde S et al (2010) Inferior vena cava collapsibility to guide fluid removal in slow continuous ultrafiltration: a pilot study. Intensive Care Med 36:692–696. https://doi.org/10.1007/s00134-009-1745-4
Patnaik S, Davila C, Lu M, Alhamshari Y, Banerji S, Pressman G (2016) Correlates of serial ultrasound guided volume assessments in patients with acute decompensated heart failure using the Vscan system. J Card Fail 22:S56
Tchernodrinski S, Lucas BP, Athavale A, Candotti C, Margeta B, Katz A et al (2014) Inferior vena cava diameter change after intravenous furosemide in patients diagnosed with acute decompensated heart failure. J Clin Ultrasound 43:187–193. https://doi.org/10.1002/jcu.22173
Cortellaro F, Ceriani E, Spinelli M, Campanella C, Bossi I, Coen D et al (2017) Lung ultrasound for monitoring cardiogenic pulmonary edema. Intern Emerg Med 12:1011–1017. https://doi.org/10.1007/s11739-016-1510-y
Daskalov I, Petrova V (2016) Reliability of B lines in follow up of patients with acute decompensated left side heart failure. Eur Heart J Acute Cardiovasc Care 5:40. https://doi.org/10.1177/2048872616663431
Facchini C, Malfatto G, Giglio A, Facchini M, Parati G, Branzi G (2016) Lung ultrasound and transthoracic impedance for noninvasive evaluation of pulmonary congestion in heart failure. J Cardiovasc Med 17:510–517. https://doi.org/10.2459/JCM.0000000000000226
Gargani L, Pang PS, Frassi F, Miglioranza MH, Dini FL, Landi P et al (2015) Persistent pulmonary congestion before discharge predicts rehospitalization in heart failure: a lung ultrasound study. Cardiovasc Ultrasound. https://doi.org/10.1186/s12947-015-0033-4
Martindale JL, Secko M, Kilpatrick JF, deSouza IS, Paladino L, Aherne A et al (2018) Serial sonographic assessment of pulmonary edema in patients with hypertensive acute heart failure. J Ultrasound Med 37:337–345. https://doi.org/10.1002/jum.14336
Palazzuoli A, Ruocco G, Beltrami M, Nuti R, Cleland JG (2018) Combined use of lung ultrasound, B-type natriuretic peptide, and echocardiography for outcome prediction in patients with acute HFrEF and HFpEF. Clin Res Cardiol 107:586–596. https://doi.org/10.1007/s00392-018-1221-7
Platz E, Campbell RT, Claggett B, Lewis EF, Groarke JD, Docherty KF et al (2019) Lung ultrasound in acute heart failure: prevalence of pulmonary congestion and short- and long-term outcomes. JACC Heart Fail 7:849–858. https://doi.org/10.1016/j.jchf.2019.07.008
Vitturi N, Soattin M, Allemand E, Simoni F, Realdi G (2011) Thoracic ultrasonography: a new method for the work-up of patients with dyspnea. J Ultrasound 14:147–151. https://doi.org/10.1016/j.jus.2011.06.009
Volpicelli G, Caramello V, Cardinale L, Mussa A, Bar F, Frascisco MF (2008) Bedside ultrasound of the lung for the monitoring of acute decompensated heart failure. Am J Emerg Med 26:585–591. https://doi.org/10.1016/j.ajem.2007.09.014
Öhman J, Harjola V-P, Karjalainen P, Lassus J (2018) Assessment of early treatment response by rapid cardiothoracic ultrasound in acute heart failure: cardiac filling pressures, pulmonary congestion and mortality. Eur Heart J Acute Cardiovasc Care 7:311–320. https://doi.org/10.1177/2048872617708974
Öhman J, Harjola VP, Karjalainen P, Lassus J (2018) Focused echocardiography and lung ultrasound protocol for guiding treatment in acute heart failure. Esc Heart Fail 5:120–128. https://doi.org/10.1002/ehf2.12208
Mozzini C, Di Dio PM, Pesce G, Garbin U, Fratta Pasini AM, Ticinesi A et al (2018) Lung ultrasound in internal medicine efficiently drives the management of patients with heart failure and speeds up the discharge time. Intern Emerg Med 13:27–33. https://doi.org/10.1007/s11739-017-1738-1
De Vecchis R, Ariano C, Fusco A, Ciccarelli A, Cioppa C, Giasi A et al (2012) Ultrasound evaluation of the inferior vena cava collapsibility index in congestive heart failure patients treated with intravenous diuretics: new insights about its relationship with renal function: an observational study. Anatol J Cardiol 12:391–400. https://doi.org/10.5152/akd.2012.121
Zhang Z, Xu X, Ye S, Xu L (2014) Ultrasonographic measurement of the respiratory variation in the inferior vena cava diameter is predictive of fluid responsiveness in critically ill patients: systematic review and meta-analysis. Ultrasound Med Biol 40:845–853. https://doi.org/10.1016/j.ultrasmedbio.2013.12.010
Long E, Oakley E, Duke T, Babl F (2017) Does respiratory variation in inferior vena cava diameter predict fluid responsiveness: a systematic review and meta-analysis. Shock 47:550–559. https://doi.org/10.1097/SHK.0000000000000801
Darwish OS, Mahayni A, Kataria S, Zuniga E, Zhang L, Amin A (2020) Diagnosis of acute heart failure using inferior vena cava ultrasound: systematic review and meta-analysis. J Ultrasound Med 39:1367–1378. https://doi.org/10.1002/jum.15231
Platz E, Merz AA, Jhund PS, Vazir A, Campbell R, McMurray JJ (2017) Dynamic changes and prognostic value of pulmonary congestion by lung ultrasound in acute and chronic heart failure: a systematic review. Eur J Heart Fail 19:1154–1163. https://doi.org/10.1002/ejhf.839
Miger KC, Fabricius-Bjerre A, Maschmann CP, Wamberg J, Winkler Wille MM, Abild-Nielsen AG et al (2019) Clinical applicability of lung ultrasound methods in the emergency department to detect pulmonary congestion on computed tomography. Ultraschall Med Eur J Ultrasound. https://doi.org/10.1055/a-1021-1470
Laursen CB, Sloth E, Lassen AT, Christensen RD, Lambrechtsen J, Madsen PH et al (2014) Point-of-care ultrasonography in patients admitted with respiratory symptoms: a single-blind, randomised controlled trial. Lancet Respir Med 2:638–646. https://doi.org/10.1016/S2213-2600(14)70135-3
Arvig MD, Lassen AT, Gæde PH, Laursen CB (2020) Monitoring patients with acute dyspnoea with a serial focused ultrasound of the heart and the lungs (MODUS): a protocol for a multicentre, randomised, open-label, pragmatic and controlled trial. BMJ Open 10:e034373. https://doi.org/10.1136/bmjopen-2019-034373
Frederiksen CA, Juhl-Olsen P, Andersen NH, Sloth E (2013) Assessment of cardiac pathology by point-of-care ultrasonography performed by a novice examiner is comparable to the gold standard. Scand J Trauma Resusc Emerg Med 21:87. https://doi.org/10.1186/1757-7241-21-87
Swamy V, Brainin P, Biering-Sørensen T, Platz E (2019) Ability of non-physicians to perform and interpret lung ultrasound: a systematic review. Eur J Cardiovasc Nurs 18:474–483. https://doi.org/10.1177/1474515119845972
Zeng X, Zhang Y, Kwong JSW, Zhang C, Li S, Sun F et al (2015) The methodological quality assessment tools for preclinical and clinical studies, systematic review and meta-analysis, and clinical practice guideline: a systematic review. J Evid Based Med 8:2–10. https://doi.org/10.1111/jebm.12141
Acknowledgements
The authors acknowledge Anne Faber Hansen, research librarian, MSci, PhD, from the University Library of Southern Denmark, who contributed to designing the search strategy. We thank Claire Gudex, MD, PhD, from the University of Southern Denmark, for editing the manuscript.
Funding
The study is supported by the Department of Emergency Medicine at Slagelse Hospital and grants from the Naestved, Slagelse, and Ringsted Hospitals’ Research Fund (Grant Number 111.2219) and by a 1-year scholarship from the University of Southern Denmark. The funders have no role in the study’s design, in the collection, analysis, or interpretation of data, in the writing of manuscripts, or in decisions to publish results.
Author information
Authors and Affiliations
Contributions
MDA has conceived the study and received inputs and feedback from ATL, NJ, PHG, and CBL. MDA developed the search strategy in cooperation with AFH. MDA and NJ screened the included studies and independently assessed the quality and extracted the data. MDA drafted the manuscript. All co-authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
Not applicable.
Consent to participate
Not applicable.
Consent for publication
Not applicable.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Arvig, M.D., Laursen, C.B., Jacobsen, N. et al. Monitoring patients with acute dyspnea with serial point-of-care ultrasound of the inferior vena cava (IVC) and the lungs (LUS): a systematic review. J Ultrasound 25, 547–561 (2022). https://doi.org/10.1007/s40477-021-00622-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40477-021-00622-7