Abstract
Purpose of Review
Review of US medical and recreational marijuana laws (MML and RML), their effects on cannabis potency, prevalence of non-medical cannabis use and cannabis use disorder (CUD) in adolescents and adults, and implications for neuroscience research, given what is known about the relationship of cannabis to neurocognitive impairments and underlying brain functioning.
Recent Findings
Cannabis potency may be increasing faster in states with MML or RML than in other states. MML and RML have not impacted prevalence in adolescents but have consistently been shown to increase rates of adult non-medical use and CUD.
Summary
Recent neurocognitive or neuroimaging studies may be more impacted by cannabis than studies conducted when MML and RML were less common. Neurocognitive or neuroimaging studies conducted in MML or RML states should carefully test potential participants for recent cannabis use. More research is needed on cannabis and cognition in medical marijuana patients.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Cannabis has been used in the United States since the 1800s, with public attitudes towards its acceptability and potential harmfulness varying considerably over time [1]. In 1970, only 12% of U.S. adults favored legalizing cannabis use [2], and the Federal Drug Enforcement Agency (DEA) defined cannabis as a Schedule 1 substance, i.e., no accepted medical use and high abuse potential [3]. Since then, legalization has steadily gained favor and many state marijuana laws have changed and become more permissive. Additionally, public perception of cannabis as a harmful substance has declined substantially among adolescents [4] and adults [5]. Consideration of the potential impact of these changes in laws and attitudes on behavioral neuroscience studies is warranted. In this review, we briefly consider the relationship of cannabis use to key areas of neurocognitive and brain functioning and describe medical and recreational cannabis laws. We then consider how changes in these laws have impacted cannabis potency, cannabis use patterns in adolescents and adults, and the increasing prevalence of people who use medical cannabis. In each of these areas, we consider the implications of the changes in the laws, and the resulting changes on cannabis characteristics and patterns for behavioral neuroscience studies.
Legalization of cannabis would not be relevant to considerations in behavioral neuroscience research if cannabis were unrelated to neurocognitive functioning. However, extensive research over the past 50 years, including hundreds of individual studies and many reviews and meta-analyses suggests that cannabis use is related to cognitive impairments and underlying brain functioning. Many debates remain in this area, including the causal nature of the relationships and reasons for some of the inconsistences in the literature. Nevertheless, broad agreement exists that acute, persistent, and heavy cannabis use affects cognition in many domains, e.g., memory, attention, and executive functioning.
Impaired attention is a key feature of acute cannabis intoxication [6•]. Whether such impairment persists following abstinence from cannabis is less clear. In the US adult general population, controlling for demographic characteristics, frequency of cannabis use in the past year predicted lower scores on an attention functioning self-report scale [7], while among those age 50 or older, people who were both current and former users (abstinent at least a year) had lower scores on attention than people who were never-users [8]. Many laboratory studies using objective attention measures have found post-abstinent deficits in attention that persist up to 30 days [6•, 9]. For example, comparing adolescents who were cannabis users and non-users [10, 11], deficits in attention were found in the adolescents who were users after 3–4 weeks of abstinence. Among participants age 16–26 with ADHD [12], cannabis use predicted attentional deficits 3 weeks post-abstinence, but ADHD symptoms did not. This study illustrates how cognitive impairment could be attributed to a psychiatric disorder if information on cannabis use was not also incorporated.
Memory is the cognitive domain most consistently reported as impaired by cannabis, with such effects found in adolescents, adults, and older adults [6•, 13•, 14,15,16]. Among adults, acute and chronic cannabis use has frequently been found to be associated with verbal and working memory impairments. These impairments are related to the duration, frequency, dose, and age of onset of cannabis use [15]. The most extensive evidence for impairment is within verbal learning and memory [14]. The effects of cannabis on working memory are less clear, perhaps because of the wide variety of working memory tasks that have been used to assess this domain [6•, 14, 15]. An open question in this area is the persistence of memory deficits post-abstinence. A recent review and meta-analysis found that overall, effects sizes for the relationship of cannabis use to cognitive deficits were diminished in studies with cognitive testing done after longer periods of abstinence in both adolescents and adults [13•]. However, this review did not address the issue of post-abstinence persistency by cognitive domain, leaving the issue unclear regarding memory. Earlier studies [17], including an earlier review [9], showed that chronic cannabis use was related to sustained post-abstinence deficits in memory function, so further research will be needed to better understand the persistence of memory deficits after cessation of cannabis use.
Executive functioning involves tasks of planning, reasoning, interference control, decision-making, and problem solving. In the US adult general population, frequency of cannabis use in the past year predicted lower scores on an executive functioning self-report scale [7], and among those age 50 and older, people who were former cannabis users (abstinent at least a year) had worse scores on executive functioning than people who were never-users [8]. Using neuropsychological test batteries in the laboratory to measure executive functioning, many although not all studies found relationships between cannabis use and impaired aspects of executive functions [6•, 13•, 18]. An example of one of these areas is inhibitory control/impulsivity, examined prospectively over several years [19], and through neuroimaging studies [20, 21]. However, due to heterogeneity of findings, reviews were inconsistent on whether cannabis use was more strongly related to impairments in executive functioning in adults in their mid-30s and older than in adolescents or young adults [6•] or among adolescents when compared with adults [22•].
A recent review of structural and functional neuroimaging studies compiled considerable information from positron emission tomography (PET) and magnetic resonance imaging (MRI) studies about brain structure and functioning related to cannabis use [23]. PET studies show that CB1 receptors are downregulated in people who were cannabis users, especially shortly after use. These changes are mainly located in the neocortex and limbic cortices, which regulate cognition, and in the ventral striatum, which is involved in reward and goal-directed behavior. Reduction of CB1 receptors in cannabis-dependent subjects returns to normal ~2 to 28 days after abstinence, although among those with chronic heavy use, the reduction in CB1 receptors may impact downstream systems that maintain changes underlying later behavioral characteristics of cannabis use disorder. Although evidence is somewhat conflicting, acute THC administration appears to cause increased dopamine release and neuronal activity, whereas long-term cannabis use is associated with blunting of the dopamine system [24], which is related to inattention. In cannabis-dependent individuals, PET studies of dopamine transporters (necessary for presynaptic dopamine reuptake) also show reduced availability in multiple brain areas, including the striatum. Glutamate also plays a role in mediating inhibitory control. Glutamatergic transmission is regulated through presynaptic terminal CB1 receptors that reduce glutamate release and are sensitive to THC. In the limited research in humans, chronic cannabis use appears to reduce levels of glutamate-derived metabolites in cortical and subcortical brain areas, while animal studies indicate that THC depresses glutamate synaptic transmission via CB1 receptor activation [25].
Human structural magnetic resonance imaging (MRI) studies show alterations in corticolimbic structures in those with CUD, e.g., prefrontal cortex (PFC), hippocampus and amygdala. The integrity of the orbitofrontal cortex (OFC within the PFC), which contributes to cognitive flexibility and decision-making, is often impaired in SUD and related to problem use. A similar sensitivity is evident in the hippocampus, a region central to learning and memory. An additional recent review and meta-analysis also showed smaller volume of the hippocampus and orbitofrontal cortex in people who were regular cannabis users compared with controls [26].
Functional magnetic resonance imaging (fMRI) studies of differences in brain functional alterations in people who were cannabis users and non-users while performing memory tasks showed that functional brain activation during the tasks was altered in the people who were cannabis users. The results suggested that the altered brain activation drove the deficits in memory performance [27]. More specifically, fMRI studies showed differential brain activity in people who were heavy cannabis users during neurocognitive tasks e.g., cost–benefit decision-making conditions, including reduced activity of the OFC and dorsolateral PFC but also increased cerebellar activity. Despite the well-documented negative cognitive impact of acute THC on working memory in drug-naïve individuals and people who were infrequent cannabis users, people who were experienced users often have normal working memory performance. However, neural networks associated with such cognitive function are not normal: people who were chronic heavy users had hyperactivation of frontal regions and networks underlying working memory. Collectively, these modifications suggest overcompensation of neural networks in people who were heavy users to achieve apparent normal executive function when cognitive demand is required.
Medical Marijuana Laws
In 1996, California became the first U.S. state to pass a medical marijuana law (MML) legalizing the use of cannabis for medical purposes. As of this writing, 34 states have MML, covering 67% of the US population (Fig. 1). State medical marijuana laws share the common feature that they permit legal use of cannabis to treat medical conditions if the person who used cannabis obtained medical authorization. However, the specific provisions of MML vary considerably [28] across states, and within states. For example, states can change the range and specificity of the permitted medical conditions and the permitted distribution outlets (e.g., dispensaries), permitted amounts per patient, etc. The restrictiveness or “medicalization” [29, 30] of MML varies as well. Concerns about MML have included their potential to increase problematic use of cannabis in the general population through several mechanisms, e.g., reducing perceived harmfulness, normalizing use [28, 31], and increasing availability via dispensaries and home cultivation [28, 31].
Recreational Marijuana Laws
In 2012, Washington and Colorado became the first states to pass laws permitting legal use of marijuana for recreational purposes (RML). Eleven states now have such laws (all of which previously had MML), covering 28% of the US population, and several additional states are considering the passage of such laws (Fig. 1). Recreational marijuana laws (RML) permit legal sale and use of cannabis without the need for medical involvement. Potential benefits of such laws include reduction of discriminatory marijuana arrests of disadvantaged minorities [32, 33] and expansion of business opportunities, jobs, and tax revenues [34,35,36]. Cannabis is now a multi-billion-dollar-a-year business [37, 38]. Since RMLs have been expected to increase availability, advertising, and accepting attitudes towards cannabis use, an increase in people who are users and thus increases in population rates of adverse health or psychosocial consequences of cannabis use has been expected as well.
Effects of Marijuana Laws: Trends in Cannabis Potency
The primary psychoactive component in cannabis is delta-9-tetrahydrocannabinol (THC). THC directly targets the body’s natural endogenous endocannabinoid system, including the receptors that mediate the direct actions of cannabinoids [23]. Cannabinoid CB1 receptors, which mediate the action of THC, are particularly concentrated in brain regions such as the hippocampus and amygdala, basal ganglia, anterior cingulate cortex, and prefrontal cortex [39]. These brain regions are associated with memory, attention, psychomotor (related to driving), inhibitory control, and higher executive functions. Cannabis potency is generally defined as the percent of THC per volume amount of the marijuana product.
In samples of illegal cannabis seized by law enforcement between 1990 and 2010 [40], mean THC potency was higher in states that passed MML (9.1%) than in other states (5.6%). Potency of cannabis products has increased since then. In Washington (where RML was first legalized in 2012), the average THC potency of marijuana for one Seattle-based retailer in 2015 was 21.2% [41]. Colorado also first passed RML in 2012. There, the THC potency of legally marketed cannabis can range considerably, with some strains having potencies of 28–32% [42]. Further, while smoking remains the most common route of administration, other routes of administration are increasingly common [43,44,45], including edibles, vaping (inhaled vapor of heated e-liquids analogous to e-cigarettes), and dabbing (inhaled vapor from heating highly-concentrated forms of cannabis or hashish). These routes offer higher THC doses than typically smoked plant marijuana in joints [43]. A recent study of online cannabis advertising showed that the mean potency of medical and recreational marijuana products was similar, 19.2 and 21.5%, respectively [46]. Because cannabis potency is related to effects on cognition, the generally stronger potency of available cannabis products may be increasingly harmful in both acute and chronic use and persist longer in abstinence. Future studies on this are needed. In the meantime, given the overall increases in potency since the 1990s accompanying changing laws and attitudes, recent neurocognitive or neuroimaging studies that include people who are cannabis users may be more impacted by cannabis than studies conducted many years ago, which should be taken into account in interpreting the results of studies done during different periods, e.g., during the 1990s vs very recent years. This issue clearly applies to groups or conditions where people who are cannabis users are the main group of interest. However, studies with other groups or conditions of primary interest may also be impacted by the increases in potency if participants are not carefully tested for recent cannabis use and excluded if they show signs of recent use.
Effects of Marijuana Laws: Trends in Adolescents Who Use Cannabis
Concerns that MML would increase adolescent cannabis use emerged about 10 years ago [47, 48], based on the possibility that MML would conveying a message that marijuana is acceptable or lacks negative consequences [49•]. An early study of national data showed that adolescent cannabis use was associated with residing in states with MML, which appeared to confirm the fears about MML effects on teens [50]. However, as Wall et al. stated in the paper, cross-sectional associations do not indicate causality. Therefore, subsequent studies of national data used difference-in-difference (DiD) methods to examine changes in state rates before and after MML passage compared with contemporaneous changes in states that did not change their marijuana laws [51,52,53,54]. Of 17 large surveys using DiD methods spanning different states, periods, and specifications, 16 indicated no MML effects on adolescent use [28, 31, 47, 55,56,57,58,59,60]. Thus, despite methodological differences between the studies, their findings were very consistent: rates of adolescent cannabis use did not increase post-MML compared with pre-MML or to national trends in non-MML states during the corresponding years.
To our knowledge, only one study to date used national data to examine the effects of recreational marijuana laws (RML) on adolescent marijuana use that analyzed data appropriate for this purpose [61•]. This study found no effects of RML on adolescent past-year use or frequent use and a weak effect on the risk of cannabis use disorder that was not robust in sensitivity analyses. A different study suggested decreases in adolescent use post-RML [62]. However, the methods of this study have been disputed [63,64,65,66]. Taken as a whole, the current literature does not indicate that increasingly permissive state marijuana laws, either medical marijuana or recreational laws, increase the prevalence of marijuana use in adolescents. Therefore, these laws appear not to have current implications for behavioral neuroscience studies of adolescents. However, continued studies and monitoring of the literature on cannabis laws and adolescents is important to determine if MML or RML effects on teen cannabis use begin to emerge.
Effects of Marijuana Laws: Adult Cannabis Use and Cannabis Use Disorders
In contrast to the relatively large literature on adolescents and MML effects, fewer studies investigated the relationship of MML or RML to adult cannabis use or related outcomes. A cross-sectional analysis of national 2004–2005 data showed higher rates of adult cannabis use and cannabis disorders in MML than in non-MML states [67]. However, studies using DiD tests were needed to examine causality. Indirectly, a study suggested MML effects on adult cannabis use by showing a 15–20% post-MML increase in urban adult marijuana possession arrests [68] and a 20% post-MML increase in first-time adult marijuana treatment admissions [68]. Using 2004–2013 data from the National Survey on Drug Use and Health (NSDUH) at a point when 10 states had passed MMLs, DiD tests indicated significant post-MML increases for adult cannabis use, daily or near-daily use, and 1- and 2-year lagged effects on CUD [31]. For cannabis use, this effect was confirmed in adults age 26 and older [56]. Using three national survey datasets from 1991 to 1992 to 2012–2013 to compare 15 MML states to other states, post-MML increases were found for adult cannabis use (Fig. 2a and CUD (Fig. 2b) [69•]. Using the same three datasets (1991–1992 to 2012–2013), post-MML increases were found in driving under the influence of cannabis [70] but not alcohol, indicating that the MML effects were substance-specific.
A study of RML effects on adults in yearly national surveys from 2008 to 2016 found no effects in young adults age 18–25 [61•]. However, among adults age 26 and older, post-RML increases were found for past-year cannabis use, frequent use, and cannabis use disorders. Thus, while the adult research base is not extensive, existing studies are consistent in showing post-MML and post-RML increases in adult cannabis-related outcomes.
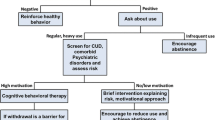
The findings on the post-MML and -RML increases in cannabis use and cannabis use disorders indicate that increasingly permissive state marijuana laws do have implications for behavioral neuroscience studies of adults, particularly those age 26 and older. Potential participants in studies conducted in states with MML and particularly RML are more likely to be people who are cannabis users and frequent users than participants in other states. For studies comparing people who are cannabis users or those with cannabis use disorders to cannabis-naïve controls, this may only affect feasibility since the pool of cannabis-naïve participants that can potentially be recruited will be smaller. However, the scientific findings of studies focused on other groups or conditions of interest may be impacted in a more serious way if participants are not carefully tested for recent cannabis use and excluded if they test positive. This may particularly affect studies of neurocognitive or brain functioning studies of depression or anxiety disorders. Cannabis withdrawal syndrome as defined in the Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-5) consists of at least 3 of the following symptoms developing within 7 days of reduced cannabis use: (1) irritability, anger, or aggression; (2) nervousness or anxiety; (3) sleep disturbance; (4) appetite or weight disturbance; (5) restlessness; (6) depressed mood; and (7) somatic symptoms, such as headaches, sweating, nausea, vomiting, or abdominal pain. The duration of this syndrome post-abstinence is unclear, but about half of people who are regular cannabis users experience cannabis withdrawal syndrome [71]. Because many cannabis withdrawal symptoms overlap with symptoms of depressive or anxiety disorders, many people who are regular cannabis users may continue using cannabis in an effort at self-medication of these depression or anxiety symptoms, unaware that this use could perpetuate a longer-term withdrawal problem [49]. In such users, if the cannabis use history is not known, cannabis withdrawal could easily be confused with depressive or anxiety disorders by clinicians or research investigators, leading to results and inferences that are unclear or potentially incorrect.
People Who Are Medical Cannabis Users Vs. People Who Are Recreational Cannabis Users
Studies of the relationship of marijuana to neurocognition and neurofunctioning have largely focused on samples of people who are recreational marijuana users. However, over two-thirds of US states now permit legal use of marijuana for medical purposes, raising issues about potential implications of medical marijuana use for neuroscience research. These include questions about whether people who are medical users are different from people who are recreational users, and whether cannabis may differentially affect people who are medical users. Several early studies from California, the first state to pass MML, showed that people who were medical and recreational users had similar characteristics and that people who were medical users often had histories of recreational use [72,73,74,75,76]. These studies suggested that in these early days of medical marijuana, the medical authorizations were often obtained by people who were recreational users. However, recent reports on medical marijuana users from national surveys provide more current, representative information. In data from the National Survey on Drug Use and Health (NSDUH), among participants who were cannabis users from MML states, those who were medical users were less likely than those who were recreational users to have good health or substance use disorders (Lin, et al. 2016). In another NSDUH study of all states, those who were medical cannabis users had poorer health, worse rdisability, older age, and late initiation of cannabis use than others [77].
Behaviors such as use and misuse of illicit substances often cluster empirically within the externalizing domain of psychopathology [78,79,80,81], typically with early onset, common etiology, and traits including sensation-seeking and impulsivity [82,83,84]. People who are recreational cannabis users seeking the sensation of feeling high are likely to differ from people who are medical patients [85, 86] seeking marijuana for relief of pain or other symptoms and who are not typically characterized by externalizing traits [87, 88]. People who are medical marijuana users may therefore differ in numerous ways from people who are recreational users in whom cognitive effects have mainly been studied to date, including later onset of use and complicating medical problems. They may also have a different set of heritable personality traits that will be reflected in results of neurocognitive and imaging studies. Studies of cannabis and cognition in people who are medical marijuana users are needed [85, 86] to determine whether marijuana effects on cognition and brain functioning differ in such users from the people who are recreational users who have been studied more extensively. In the end, such studies may provide a broader, richer understanding of the relationship of cannabis to neurofunctioning.
Conclusions
In summary and conclusion, the population prevalence of people who are regular or heavy use of cannabis among US adults has increased over the last 20 years, medical marijuana use is now largely permitted across the USA, and adult residents of states that have legalized cannabis are more likely to be people who use cannabis recreationally and to have cannabis use disorders. Therefore, when evaluating participant eligibility for studies of neurocognitive or brain functioning, carefully evaluating a history of recent use (recreational or medical) via interviewing and biological tests will be increasingly important to avoid misleading results or simply reduce error variance in such studies. Additionally, for clinical care, careful histories about marijuana use at the beginning of treatment could avoid diagnostic confusion and provide a better basis for treatment planning, monitored by periodic check-ins on marijuana use as treatment proceeds.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance
Musto DF. Opium, cocaine and marijuana in American history. Sci Am. 1991;265(1):40–7.
Jones JM. U.S. Support for Legal Marijuana Steady in Past Year. Gallup News. October 23 2019.
U.S. Department of Justice, Drug Enforcement Administration. Controlled substance schedules. 2017. https://www.deadiversion.usdoj.gov/schedules/. Accessed March 15 2017.
Sarvet AL, Wall MM, Keyes KM, Cerda M, Schulenberg JE, O'Malley PM, et al. Recent rapid decrease in adolescents' perception that marijuana is harmful, but no concurrent increase in use. Drug Alcohol Depend. 2018;186:68–74. https://doi.org/10.1016/j.drugalcdep.2017.12.041.
Compton WM, Han B, Jones CM, Blanco C, Hughes A. Marijuana use and use disorders in adults in the USA, 2002-14: analysis of annual cross-sectional surveys. Lancet Psychiatry. 2016;3(10):954–64. https://doi.org/10.1016/S2215-0366(16)30208-5.
• Broyd SJ, van Hell HH, Beale C, Yucel M, Solowij N. Acute and chronic effects of cannabinoids on human cognition-a systematic review. Biol Psychiatry. 2016;79(7):557–67. https://doi.org/10.1016/j.biopsych.2015.12.002This review provides a comprehensive synthesis of research findings published in the past decade on acute and chronic effects of cannabis on cognitive functioning across a range of domains.
Aharonovich E, Shmulewitz D, Wall MM, Grant BF, Hasin DS. Self-reported cognitive scales in a US National Survey: reliability, validity, and preliminary evidence for associations with alcohol and drug use. Addiction. 2017;112(12):2132–43. https://doi.org/10.1111/add.13911.
Benitez A, Lauzon S, Nietert PJ, McRae-Clark A, Sherman BJ. Self-reported cognition and marijuana use in older adults: results from the national epidemiologic survey on alcohol and related conditions-III. Addict Behav. 2020;108:106437. https://doi.org/10.1016/j.addbeh.2020.106437.
Ganzer F, Broning S, Kraft S, Sack PM, Thomasius R. Weighing the evidence: a systematic review on long-term neurocognitive effects of Cannabis use in abstinent adolescents and adults. Neuropsychol Rev. 2016;26(2):186–222. https://doi.org/10.1007/s11065-016-9316-2.
Hanson KL, Winward JL, Schweinsburg AD, Medina KL, Brown SA, Tapert SF. Longitudinal study of cognition among adolescent marijuana users over three weeks of abstinence. Addict Behav. 2010;35(11):970–6. https://doi.org/10.1016/j.addbeh.2010.06.012.
Medina KL, Hanson KL, Schweinsburg AD, Cohen-Zion M, Nagel BJ, Tapert SF. Neuropsychological functioning in adolescent marijuana users: subtle deficits detectable after a month of abstinence. J Int Neuropsychol Soc. 2007;13(5):807–20. https://doi.org/10.1017/S1355617707071032.
Wallace AL, Wade NE, Hatcher KF, Lisdahl KM. Effects of Cannabis use and subclinical ADHD symptomology on attention based tasks in adolescents and young adults. Arch Clin Neuropsychol. 2019;34(5):700–5. https://doi.org/10.1093/arclin/acy080.
• Scott JC, Slomiak ST, Jones JD, Rosen AFG, Moore TM, Gur RC. Association of cannabis with cognitive functioning in adolescents and young adults: a systematic review and meta-analysis. JAMA Psychiatry. 2018;75(6):585–95. https://doi.org/10.1001/jamapsychiatry.2018.0335This review provides an extensive description of the cannabis effects on cognitive functions in adolescents and young adults.
Schweinsburg AD, Brown SA, Tapert SF. The influence of marijuana use on neurocognitive functioning in adolescents. Curr Drug Abuse Rev. 2008;1(1):99–111. https://doi.org/10.2174/1874473710801010099.
Solowij N, Battisti R. The chronic effects of cannabis on memory in humans: a review. Curr Drug Abuse Rev. 2008;1(1):81–98. https://doi.org/10.2174/1874473710801010081.
Sagar KA, Gruber SA. Interactions between recreational cannabis use and cognitive function: lessons from functional magnetic resonance imaging. Ann N Y Acad Sci. 2019;1451(1):42–70. https://doi.org/10.1111/nyas.13990.
Meier MH, Caspi A, Ambler A, Harrington H, Houts R, Keefe RS, et al. Persistent cannabis users show neuropsychological decline from childhood to midlife. Proc Natl Acad Sci U S A. 2012;109(40):E2657–64. https://doi.org/10.1073/pnas.1206820109.
Crean RD, Crane NA, Mason BJ. An evidence based review of acute and long-term effects of cannabis use on executive cognitive functions. J Addict Med. 2011;5(1):1–8. https://doi.org/10.1097/ADM.0b013e31820c23fa.
Paige KJ, Colder CR. Long-term effects of early adolescent marijuana use on attentional and inhibitory control. J Stud Alcohol Drugs. 2020;81(2):164–72.
Wrege J, Schmidt A, Walter A, Smieskova R, Bendfeldt K, Radue EW, et al. Effects of cannabis on impulsivity: a systematic review of neuroimaging findings. Curr Pharm Des. 2014;20(13):2126–37. https://doi.org/10.2174/13816128113199990428.
Ramaekers JG, van Wel JH, Spronk D, Franke B, Kenis G, Toennes SW, et al. Cannabis and cocaine decrease cognitive impulse control and functional corticostriatal connectivity in drug users with low activity DBH genotypes. Brain Imaging Behav. 2016;10(4):1254–63. https://doi.org/10.1007/s11682-015-9488-z.
• Gorey C, Kuhns L, Smaragdi E, Kroon E, Cousijn J. Age-related differences in the impact of cannabis use on the brain and cognition: a systematic review. Eur Arch Psychiatry Clin Neurosci. 2019;269(1):37–58. https://doi.org/10.1007/s00406-019-00981-7This review critically examines the moderating role of age on the relationship between cannabis use and cognition.
Ferland JN, Hurd YL. Deconstructing the neurobiology of cannabis use disorder. Nat Neurosci. 2020;23(5):600–10. https://doi.org/10.1038/s41593-020-0611-0.
Bloomfield MA, Ashok AH, Volkow ND, Howes OD. The effects of Delta(9)-tetrahydrocannabinol on the dopamine system. Nature. 2016;539(7629):369–77. https://doi.org/10.1038/nature20153.
Colizzi M, McGuire P, Pertwee RG, Bhattacharyya S. Effect of cannabis on glutamate signalling in the brain: a systematic review of human and animal evidence. Neurosci Biobehav Rev. 2016;64:359–81. https://doi.org/10.1016/j.neubiorev.2016.03.010.
Lorenzetti V, Chye Y, Silva P, Solowij N, Roberts CA. Does regular cannabis use affect neuroanatomy? An updated systematic review and meta-analysis of structural neuroimaging studies. Eur Arch Psychiatry Clin Neurosci. 2019;269(1):59–71. https://doi.org/10.1007/s00406-019-00979-1.
Blest-Hopley G, Giampietro V, Bhattacharyya S. A systematic review of human neuroimaging evidence of memory-related functional alterations associated with cannabis use complemented with preclinical and human evidence of memory performance alterations. Brain Sci. 2020;10(2). https://doi.org/10.3390/brainsci10020102.
Pacula RL, Powell D, Heaton P, Sevigny EL. Assessing the effects of medical marijuana laws on marijuana use: the devil is in the details. J Policy Anal Manage. 2015;34(1):7–31.
Williams AR, Santaella-Tenorio J, Mauro CM, Levin FR, Martins SS. Loose regulation of medical marijuana programs associated with higher rates of adult marijuana use but not cannabis use disorder. Addiction. 2017;112:1985–91. https://doi.org/10.1111/add.13904.
Williams AR, Olfson M, Kim JH, Martins SS, Kleber HD. Older, less regulated medical marijuana programs have much greater enrollment rates than newer ‘medicalized’ programs. Health Aff (Millwood). 2016;35(3):480–8. https://doi.org/10.1377/hlthaff.2015.0528.
Wen H, Hockenberry JM, Cummings JR. The effect of medical marijuana laws on adolescent and adult use of marijuana, alcohol, and other substances. J Health Econ. 2015;42:64–80. https://doi.org/10.1016/j.jhealeco.2015.03.007.
Palamar JJ, Ompad DC, Petkova E. Correlates of intentions to use cannabis among US high school seniors in the case of cannabis legalization. Int J Drug Policy. 2014;25(3):424–35. https://doi.org/10.1016/j.drugpo.2014.01.017.
Hall W, Lynskey M. Evaluating the public health impacts of legalizing recreational cannabis use in the United States. Addiction. 2016;111(10):1764–73. https://doi.org/10.1111/add.13428.
McGinty EE, Samples H, Bandara SN, Saloner B, Bachhuber MA, Barry CL. The emerging public discourse on state legalization of marijuana for recreational use in the US: analysis of news media coverage, 2010-2014. Prev Med. 2016;90:114–20. https://doi.org/10.1016/j.ypmed.2016.06.040.
McGinty EE, Niederdeppe J, Heley K, Barry CL. Public perceptions of arguments supporting and opposing recreational marijuana legalization. Prev Med. 2017;99:80–6. https://doi.org/10.1016/j.ypmed.2017.01.024.
Forbes. $1 Billion In Marijuana Taxes Is Addictive To State Governors. 2017. https://www.forbes.com/sites/debraborchardt/2017/04/11/1-billion-in-marijuana-taxes-is-addicting-to-state-governors/#5b20042d2c3b. Accessed June 30 2017.
Wang GS, Hall K, Vigil D, Banerji S, Monte A, VanDyke M. Marijuana and acute health care contacts in Colorado. Prev Med. 2017;104:24–30. https://doi.org/10.1016/j.ypmed.2017.03.022.
Dorbian I. New Cannabis Report Predicts Legal Sales To Reach Nearly $30 Billion By 2025. Forbes. September 24, 2019.
Burns HD, Van Laere K, Sanabria-Bohorquez S, Hamill TG, Bormans G, Eng WS, et al. [18F]MK-9470, a positron emission tomography (PET) tracer for in vivo human PET brain imaging of the cannabinoid-1 receptor. Proc Natl Acad Sci U S A. 2007;104(23):9800–5. https://doi.org/10.1073/pnas.0703472104.
Sevigny EL, Pacula RL, Heaton P. The effects of medical marijuana laws on potency. Int J Drug Policy. 2014;25(2):308–19. https://doi.org/10.1016/j.drugpo.2014.01.003.
Washington State Marijuana Impact Report. Seattle, WA. 2016. http://www.riag.ri.gov/documents/NWHIDTAMarijuanaImpactReportVolume1.pdf. Accessed July 2 2017.
CNN. Colorado marijuana's potency getting 'higher'. 2016. http://www.cnn.com/2016/10/21/health/colorado-marijuana-potency-above-national-average/index.html?_sm_au_=iVVwFVZDW6Q7kD46. Accessed July 2 2017.
Hall W, Renström M, Poznyak V. The health and social effects of nonmedical cannabis use. Management of substance abuse. Geneva: World Health Organization; 2016.
Knapp AA, Lee DC, Borodovsky JT, Auty SG, Gabrielli J, Budney AJ. Emerging trends in Cannabis administration among adolescent Cannabis users. J Adolesc Health. 2019;64(4):487–93. https://doi.org/10.1016/j.jadohealth.2018.07.012.
Borodovsky JT, Lee DC, Crosier BS, Gabrielli JL, Sargent JD, Budney AJ. U.S. cannabis legalization and use of vaping and edible products among youth. Drug Alcohol Depend. 2017;177:299–306. https://doi.org/10.1016/j.drugalcdep.2017.02.017.
Cash MC, Cunnane K, Fan C, Romero-Sandoval EA. Mapping cannabis potency in medical and recreational programs in the United States. PLoS One. 2020;15(3):e0230167. https://doi.org/10.1371/journal.pone.0230167.
Hasin DS, Wall M, Keyes KM, Cerda M, Schulenberg J, O'Malley PM, et al. Medical marijuana laws and adolescent marijuana use in the USA from 1991 to 2014: results from annual, repeated cross-sectional surveys. Lancet Psychiatry. 2015;2(7):601–8. https://doi.org/10.1016/S2215-0366(15)00217-5.
Medical Marijuana Policy Research: Exploring trends and impacts (R01). National Institutes of Health; 2011. https://grants.nih.gov/grants/guide/rfa-files/rfa-da-11-008.html.
• Hasin DS. US epidemiology of Cannabis use and associated problems. Neuropsychopharmacology. 2018;43(1):195–212. https://doi.org/10.1038/npp.2017.198This study provides a comprehensive review of the epidemiology of cannabis use in the US.
Wall MM, Poh E, Cerda M, Keyes KM, Galea S, Hasin DS. Adolescent marijuana use from 2002 to 2008: higher in states with medical marijuana laws, cause still unclear. Ann Epidemiol. 2011;21(9):714–6. https://doi.org/10.1016/j.annepidem.2011.06.001.
Imbens GW, Wooldridge JM. Recent developments in the econometrics of program evaluation. J Econ Lit. 2009;47(1):5–86.
Angrist JD, Pischke JS. Mostly harmless econometrics: an empiricist’s companion. Princeton; 2009.
Hunt PE, Miles J. The impact of legalizing and regulating weed: issues with study design and emerging findings in the USA. Curr Top Behav Neurosci. 2015. https://doi.org/10.1007/7854_2015_423.
Angrist J, Krueger AB. Empirical strategies in labor economics. Handbook of labor economics. Amsterdam: Elsevier; 1999.
Choi A. The impact of medical marijuana laws on marijuana use and other risky health behaviors. The American Society of Health Economists: Los Angeles; 2014.
Martins SS, Mauro CM, Santaella-Tenorio J, Kim JH, Cerda M, Keyes KM, et al. State-level medical marijuana laws, marijuana use and perceived availability of marijuana among the general U.S. population. Drug Alcohol Depend. 2016;169:26–32. https://doi.org/10.1016/j.drugalcdep.2016.10.004.
Keyes KM, Wall M, Cerda M, Schulenberg J, O'Malley PM, Galea S, et al. How does state marijuana policy affect US youth? Medical marijuana laws, marijuana use and perceived harmfulness: 1991-2014. Addiction. 2016;111(12):2187–95. https://doi.org/10.1111/add.13523.
Anderson DM, Hansen B, Rees DI. Medical Marijuana Laws and Teen Marijuana Use. Am Law Econ Rev. 2015;17(2):495–528. https://doi.org/10.1093/aler/ahv002.
Smart R. The kids aren’t alright but older adults are just fine: effects of medical marijuana market growth on substance use and abuse. 2015.
Sarvet A, Wall M, Fink DS, Greene E, Le A, Boustead AE et al. Medical marijuana laws and adolescent marijuana use: a systematic review. Under Review.
• Cerda M, Mauro C, Hamilton A, Levy NS, Santaella-Tenorio J, Hasin D, et al. Association between recreational marijuana legalization in the United States and changes in marijuana use and Cannabis use disorder from 2008 to 2016. JAMA Psychiatry. 2019. https://doi.org/10.1001/jamapsychiatry.2019.3254This study shows national effects of changing recreational marijuana laws on adolescent and adult marijuana and cannabis use disorder.
Anderson DM, Hansen B, Rees DI, Sabia JJ. Association of marijuana laws with teen marijuana use: new estimates from the youth risk behavior surveys. JAMA Pediatr. 2019;173:879. https://doi.org/10.1001/jamapediatrics.2019.1720.
Jones CM, Underwood JM, Volkow ND. Challenging the association of marijuana Laws with teen marijuana use. JAMA Pediatr. 2019;174:99. https://doi.org/10.1001/jamapediatrics.2019.4235.
Kamer R. Challenging the association of marijuana laws with teen Marijuana use. JAMA Pediatr. 2019;174:97. https://doi.org/10.1001/jamapediatrics.2019.4229.
Rapoport E, Keim SA, Adesman A. Challenging the association of marijuana laws with teen marijuana use. JAMA Pediatr. 2019;174:98. https://doi.org/10.1001/jamapediatrics.2019.4250.
Miller CL. Challenging the association of marijuana laws with teen marijuana use. JAMA Pediatr. 2019;174:96. https://doi.org/10.1001/jamapediatrics.2019.4232.
Cerda M, Wall M, Keyes KM, Galea S, Hasin D. Medical marijuana laws in 50 states: investigating the relationship between state legalization of medical marijuana and marijuana use, abuse and dependence. Drug Alcohol Depend. 2012;120(1–3):22–7. https://doi.org/10.1016/j.drugalcdep.2011.06.011.
Chu YW. The effects of medical marijuana laws on illegal marijuana use. J Health Econ. 2014;38:43–61. https://doi.org/10.1016/j.jhealeco.2014.07.003.
• Hasin DS, Sarvet AL, Cerda M, Keyes KM, Stohl M, Galea S, et al. US adult illicit cannabis use, cannabis use disorder, and medical marijuana Laws: 1991-1992 to 2012-2013. JAMA Psychiatry. 2017;74(6):579–88. https://doi.org/10.1001/jamapsychiatry.2017.0724This study shows national effects of changing medical marijuana laws on adult marijuana and cannabis use disorder.
Fink DS, Stohl M, Sarvet AL, Cerda M, Keyes KM, Hasin DS. Medical marijuana laws and driving under the influence of marijuana and alcohol. Addiction. 2020;115:1944–53. https://doi.org/10.1111/add.15031.
Bahji A, Stephenson C, Tyo R, Hawken ER, Seitz DP. Prevalence of Cannabis withdrawal symptoms among people with regular or dependent use of cannabinoids: a systematic review and meta-analysis. JAMA Netw Open. 2020;3(4):e202370. https://doi.org/10.1001/jamanetworkopen.2020.2370.
Haug NA, Padula CB, Sottile JE, Vandrey R, Heinz AJ, Bonn-Miller MO. Cannabis use patterns and motives: a comparison of younger, middle-aged, and older medical cannabis dispensary patients. Addict Behav. 2017;72:14–20. https://doi.org/10.1016/j.addbeh.2017.03.006.
Reinarman C, Nunberg H, Lanthier F, Heddleston T. Who are medical marijuana patients? Population characteristics from nine California assessment clinics. J Psychoactive Drugs. 2011;43(2):128–35. https://doi.org/10.1080/02791072.2011.587700.
Harris D, Jones RT, Shank R, Nath R, Fernandez E, Goldstein K, et al. Self-reported marijuana effects and characteristics of 100 San Francisco medical marijuana club members. J Addict Dis. 2000;19(3):89–103. https://doi.org/10.1300/J069v19n03_07.
Walsh Z, Callaway R, Belle-Isle L, Capler R, Kay R, Lucas P, et al. Cannabis for therapeutic purposes: patient characteristics, access, and reasons for use. Int J Drug Policy. 2013;24(6):511–6. https://doi.org/10.1016/j.drugpo.2013.08.010.
O'Connell TJ, Bou-Matar CB. Long term marijuana users seeking medical cannabis in California (2001-2007): demographics, social characteristics, patterns of cannabis and other drug use of 4117 applicants. Harm Reduct J. 2007;4:16. https://doi.org/10.1186/1477-7517-4-16.
Compton WM, Han B, Hughes A, Jones CM, Blanco C. Use of marijuana for medical purposes among adults in the United States. JAMA. 2017;317(2):209–11. https://doi.org/10.1001/jama.2016.18900.
Eaton NR, Rodriguez-Seijas C, Carragher N, Krueger RF. Transdiagnostic factors of psychopathology and substance use disorders: a review. Soc Psychiatry Psychiatr Epidemiol. 2015;50(2):171–82. https://doi.org/10.1007/s00127-014-1001-2.
Kotov R, Ruggero CJ, Krueger RF, Watson D, Yuan Q, Zimmerman M. New dimensions in the quantitative classification of mental illness. Arch Gen Psychiatry. 2011;68(10):1003–11. https://doi.org/10.1001/archgenpsychiatry.2011.107.
Vrieze SI, Perlman G, Krueger RF, Iacono WG. Is the continuity of externalizing psychopathology the same in adolescents and middle-aged adults? A test of the externalizing spectrum’s developmental coherence. J Abnorm Child Psychol. 2012;40(3):459–70. https://doi.org/10.1007/s10802-011-9571-x.
Keyes KM, Eaton NR, Krueger RF, Skodol AE, Wall MM, Grant B, et al. Thought disorder in the meta-structure of psychopathology. Psychol Med. 2013;43(8):1673–83. https://doi.org/10.1017/S0033291712002292.
Barr PB, Dick DM. The genetics of externalizing problems. Curr Top Behav Neurosci. 2019. https://doi.org/10.1007/7854_2019_120.
Gustavson DE, Franz CE, Panizzon MS, Lyons MJ, Kremen WS. Internalizing and externalizing psychopathology in middle age: genetic and environmental architecture and stability of symptoms over 15 to 20 years. Psychol Med. 2019;50:1–9. https://doi.org/10.1017/S0033291719001533.
Krueger RF. The structure of common mental disorders. Arch Gen Psychiatry. 1999;56(10):921–6. https://doi.org/10.1001/archpsyc.56.10.921.
Sagar KA, Gruber SA. Marijuana matters: reviewing the impact of marijuana on cognition, brain structure and function, & exploring policy implications and barriers to research. Int Rev Psychiatry. 2018;30(3):251–67. https://doi.org/10.1080/09540261.2018.1460334.
Burggren AC, Shirazi A, Ginder N, London ED. Cannabis effects on brain structure, function, and cognition: considerations for medical uses of cannabis and its derivatives. Am J Drug Alcohol Abuse. 2019;45(6):563–79. https://doi.org/10.1080/00952990.2019.1634086.
Krueger RF, Chentsova-Dutton YE, Markon KE, Goldberg D, Ormel J. A cross-cultural study of the structure of comorbidity among common psychopathological syndromes in the general health care setting. J Abnorm Psychol. 2003;112(3):437–47. https://doi.org/10.1037/0021-843x.112.3.437.
Krueger RF, Tackett JL, Markon KE. Structural models of comorbidity among common mental disorders: connections to chronic pain. Adv Psychosom Med. 2004;25:63–77. https://doi.org/10.1159/000079058.
Author information
Authors and Affiliations
Corresponding author
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Support: R01DA048860, the New York State Psychiatric Institute
This article is part of the Topical Collection on Addictions
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Hasin, D.S., Aharonovich, E. Implications of Medical and Recreational Marijuana Laws for Neuroscience Research: a Review. Curr Behav Neurosci Rep 7, 258–266 (2020). https://doi.org/10.1007/s40473-020-00222-5
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40473-020-00222-5