Abstract
Purpose of Review
This review summarizes empirical research on trust in BPD, including three primary areas: the prevalence of paranoia, trustworthiness appraisals, and trust-related behaviors in economic exchange paradigms. Connections to the largely theoretical study of epistemic trust in BPD are highlighted.
Recent Findings
In trust appraisal paradigms, people with BPD have a bias to rate others as untrustworthy. In behavioral exchange games, they report lower trust in partners and are more likely to rupture cooperation. Recent research has suggested potential explanations for these findings, including differences in affective processing, aberrant social norms and expectations, and difficulty attending to and incorporating social cues.
Summary
People with BPD commonly experience paranoia, generally regard others as untrustworthy, and act accordingly. Further research is needed to understand the mechanisms of altered trust processing and to integrate empirical research with recent theoretical research on epistemic trust.
Similar content being viewed by others
References
Papers of particular interest, published recently, have been highlighted as: • Of importance
Rousseau DM, Sitkin SB, Burt RS, Camerer C. Introduction to special topic forum. Not so different after all: a cross-discipline view of trust. Acad Manag Rev. 1998;23:393–404.
Simpson JA. Psychological foundations of trust. Curr Dir Psychol Sci. 2007;16:264–8. https://doi.org/10.1111/j.1467-8721.2007.00517.x.
Fitzpatrick J, Lafontaine M-F. Attachment, trust, and satisfaction in relationships: investigating actor, partner, and mediating effects. Pers Relatsh. 2017;24:640–62. https://doi.org/10.1111/pere.12203.
Campbell L, Simpson JA, Boldry JG, Rubin H. Trust, variability in relationship evaluations, and relationship processes. J Pers Soc Psychol. 2010;99:14–31. https://doi.org/10.1037/a0019714.
Kim JS, Weisberg YJ, Simpson JA, Oriña MM, Farrell AK, Johnson WF. Ruining it for both of us: the disruptive role of low-trust partners on conflict resolution in romantic relationships. Soc Cogn. 2015;33:520–42. https://doi.org/10.1521/soco.2015.33.5.520.
American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 5th ed. Washington DC: 2013.
Trull TJ, Widiger TA. Dimensional models of personality: the five-factor model and the DSM-5. Dialogues Clin Neurosci. 2013;15:135–46.
Bateman A, Campbell C, Luyten P, Fonagy P. A mentalization-based approach to common factors in the treatment of borderline personality disorder. Curr Opin Psychol. 2018;21:44–9. https://doi.org/10.1016/j.copsyc.2017.09.005.
Bo S, Sharp C, Fonagy P, Kongerslev M. Hypermentalizing, attachment, and epistemic trust in adolescent BPD: clinical illustrations. Personal Disord. 2017;8:172–82. https://doi.org/10.1037/per0000161.
Botsford J, Schulze L, Bohländer J, Renneberg B. Interpersonal trust: development and validation of a self-report inventory and clinical application in patients with borderline personality disorder. J Personal Disord. 2019:1–22. https://doi.org/10.1521/pedi_2019_33_462.
Fallon P. Travelling through the system: the lived experience of people with borderline personality disorder in contact with psychiatric services. J Psychiatr Ment Health Nurs. 2003;10:393–400. https://doi.org/10.1046/j.1365-2850.2003.00617.x.
Hirsh JB, Quilty LC, Bagby RM, McMain SF. The relationship between agreeableness and the development of the working alliance in patients with borderline personality disorder. J Personal Disord. 2012;26:616–27. https://doi.org/10.1521/pedi.2012.26.4.616.
Katsakou C, Pistrang N, Barnicot K, White H, Priebe S. Processes of recovery through routine or specialist treatment for borderline personality disorder (BPD): a qualitative study. J Ment Health. 2019;28:604–12. https://doi.org/10.1080/09638237.2017.1340631.
Langley GC, Klopper H. Trust as a foundation for the therapeutic intervention for patients with borderline personality disorder. J Psychiatr Ment Health Nurs. 2005;12:23–32. https://doi.org/10.1111/j.1365-2850.2004.00774.x.
Orme W, Bowersox L, Vanwoerden S, Fonagy P, Sharp C. The relation between epistemic trust and borderline pathology in an adolescent inpatient sample. Borderline Personal Disord Emot Dysregul. 2019;6:13. https://doi.org/10.1186/s40479-019-0110-7.
Romeu-Labayen M, Rigol Cuadra MA, Galbany-Estragués P, Blanco Corbal S, Giralt Palou RM, Tort-Nasarre G. Borderline personality disorder in a community setting: service users’ experiences of the therapeutic relationship with mental health nurses. Int J Ment Health Nurs. 2020. https://doi.org/10.1111/inm.12720.
Stern A. Psychoanalytic investigation of and therapy in the border line group of neuroses. Psychoanal Q. 1938;7:467–89.
Zanarini MC, Gunderson JG, Frankenburg FR, Chauncey DL. Discriminating borderline personality disorder from other axis II disorders. Am J Psychiatry. 1990;147:161–7. https://doi.org/10.1176/ajp.147.2.161.
Oliva F, Dalmotto M, Pirfo E, Furlan PM, Picci RL. A comparison of thought and perception disorders in borderline personality disorder and schizophrenia: psychotic experiences as a reaction to impaired social functioning. BMC Psychiatry. 2014;14. https://doi.org/10.1186/s12888-014-0239-2.
Zanarini MC, Frankenburg FR, Wedig MM, Fitzmaurice GM. Cognitive experiences reported by patients with borderline personality disorder and axis II comparison subjects: a 16-year prospective follow-up study. Am J Psychiatry. 2013;170:671–9. https://doi.org/10.1176/appi.ajp.2013.13010055.
Allen B, Cramer RJ, Harris PB, Rufino KA. Borderline personality symptomatology as a mediator of the link between child maltreatment and adult suicide potential. Arch Suicide Res. 2013;17:41–51. https://doi.org/10.1080/13811118.2013.748413.
Muñoz-Negro JE, Prudent C, Gutiérrez B, Cervilla JA. Paranoia and risk of personality disorder in the general population. Personal Ment Health. 2019;13:107–16. https://doi.org/10.1002/pmh.1443.
Snyder S, Pitts WM. Characterizing paranoia in the DSM-III borderline personality disorder. Acta Psychiatr Scand. 1986;73:500–5. https://doi.org/10.1111/j.1600-0447.1986.tb02716.x.
Glaser J-P, Van Os J, Thewissen V, Myin-Germeys I. Psychotic reactivity in borderline personality disorder. Acta Psychiatr Scand. 2010;121:125–34. https://doi.org/10.1111/j.1600-0447.2009.01427.x.
Bhar SS, Brown GK, Beck AT. Dysfunctional beliefs and psychopathology in borderline personality disorder. J Personal Disord. 2008;22:165–77. https://doi.org/10.1521/pedi.2008.22.2.165.
Bach B, Farrell JM. Schemas and modes in borderline personality disorder: the mistrustful, shameful, angry, impulsive, and unhappy child. Psychiatry Res. 2018;259:323–9. https://doi.org/10.1016/j.psychres.2017.10.039.
Bach B, Lobbestael J. Elucidating DSM-5 and ICD-11 diagnostic features of borderline personality disorder using schemas and modes. Psychopathology. 2018;51:400–7. https://doi.org/10.1159/000495845.
Frías Á, Navarro S, Palma C, Farriols N, Aliaga F, Salvador A, et al. Early maladaptive schemas associated with dimensional and categorical psychopathology in patients with borderline personality disorder. Clin Psychol Psychother. 2018;25:30–41. https://doi.org/10.1002/cpp.2123.
Butler AC, Brown GK, Beck AT, Grisham JR. Assessment of dysfunctional beliefs in borderline personality disorder. Behav Res Ther. 2002;40:1231–40. https://doi.org/10.1016/s0005-7967(02)00031-1.
Hallquist MN, Pilkonis PA. Refining the phenotype of borderline personality disorder: diagnostic criteria and beyond. Personal Disord. 2012;3:228–46. https://doi.org/10.1037/a0027953.
Fertuck EA, Grinband J, Stanley B. Facial trust appraisal negatively biased in borderline personality disorder. Psychiatry Res. 2013;207:195–202. https://doi.org/10.1016/j.psychres.2013.01.004.
• Masland SR, Hooley JM. When trust does not come easily: negative emotional information unduly influences trustworthiness appraisals for individuals with borderline personality features. J Pers Disord. 2019:1–16. https://doi.org/10.1521/pedi_2019_33_404Replicates the finding that people with BPD have a bias to rate others as untrustworthy. Found that negative affective context may augment this bias, which suggests potential affective mechanisms.
Miano A, Fertuck EA, Arntz A, Stanley B. Rejection sensitivity is a mediator between borderline personality disorder features and facial trust appraisal. J Personal Disord. 2013;27:442–56. https://doi.org/10.1521/pedi_2013_27_096.
• Miano A, Fertuck EA, Roepke S, Dziobek I. Romantic relationship dysfunction in borderline personality disorder—a naturalistic approach to trustworthiness perception. Personal Disord. 2017;8:281–6. https://doi.org/10.1037/per0000196A rare exception to significant issues with ecological validity in this body of research. This study considers how people with BPD consider the trustworthiness of their real relationship partners, and suggests, like Masland & Hooley (2019) and Richetin et al. (2018), that negative affective processes may provide clues to the mechanisms underlying trust bias.
Nicol K, Pope M, Sprengelmeyer R, Young AW, Hall J. Social judgement in borderline personality disorder. PLoS One. 2013;8. https://doi.org/10.1371/journal.pone.0073440.
• Richetin J, Poggi A, Ricciardelli P, Fertuck EA, Preti E. The emotional components of rejection sensitivity as a mediator between borderline personality disorder and biased appraisal of trust in faces. Clin Neuropsychiatry J Treat Eval. 2018;15:200–5 Shows that affective, but not cognitive, components of rejection sensitivity mediate the association between borderline personality traits and biased trustworthiness appraisal. This is important for moving toward an understanding of the mechanisms underlying trust bias.
• Fineberg SK, Leavitt J, Stahl DS, Kronemer S, Landry CD, Alexander-Bloch A, et al. Differential valuation and learning from social and nonsocial cues in borderline personality disorder. Biol Psychiatry. 2018;84:838–45. https://doi.org/10.1016/j.biopsych.2018.05.020People with BPD are less sensitive to partner volatility. Suggests that people with BPD expect partner betrayal, and are so used to real or perceived signs of partner betrayal that they may fail to notice and respond to these signs.
Franzen N, Hagenhoff M, Baer N, Schmidt A, Mier D, Sammer G, et al. Superior ‘theory of mind’ in borderline personality disorder: an analysis of interaction behavior in a virtual trust game. Psychiatry Res. 2011;187:224–33. https://doi.org/10.1016/j.psychres.2010.11.012.
Hepp J, Störkel LM, Kieslich PJ, Schmahl C, Niedtfeld I. Negative evaluation of individuals with borderline personality disorder at zero acquaintance. Behav Res Ther. 2018;111:84–91. https://doi.org/10.1016/j.brat.2018.09.009.
• Hula A, Vilares I, Lohrenz T, Dayan P, Montague PR. A model of risk and mental state shifts during social interaction. PLoS Comput Biol. 2018;14. https://doi.org/10.1371/journal.pcbi.1005935This is a computational re-analysis of a seminal trust game study (King-Casas et al., 2008). Shows that people with BPD are less likely to attend to cues that their game partner is irritable, and therefore less likely to alter their behavior to repair trust ruptures.
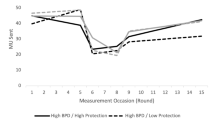
• King-Casas B, Sharp C, Lomax-Bream L, Lohrenz T, Fonagy P, Montague PR. The rupture and repair of cooperation in borderline personality disorder. Science. 2008;321:806–10. https://doi.org/10.1126/science.1156902Despite its age, this is a seminal study in this area. This was the first use of a behavioral exchange paradigm to study trust processing in BPD, and includes behavioral and neural measures.
• Liebke L, Koppe G, Bungert M, Thome J, Hauschild S, Defiebre N, et al. Difficulties with being socially accepted: an experimental study in borderline personality disorder. J Abnorm Psychol. 2018;127:670–82. https://doi.org/10.1037/abn0000373Suggests that people with BPD are sensitive to and able to use experiences of partner rejection to adjust their behavior and expectations, but that they react to partner acceptance paradoxically, with less trust and cooperation.
Preuss N, Brändle LS, Hager OM, Haynes M, Fischbacher U, Hasler G. Inconsistency and social decision making in patients with borderline personality disorder. Psychiatry Res. 2016;243:115–22. https://doi.org/10.1016/j.psychres.2016.06.017.
Thielmann I, Hilbig BE, Niedtfeld I. Willing to give but not to forgive: borderline personality features and cooperative behavior. J Personal Disord. 2014;28:778–95. https://doi.org/10.1521/pedi_2014_28_135.
Unoka Z, Seres I, Áspán N, Bódi N, Kéri S. Trust game reveals restricted interpersonal transactions in patients with borderline personality disorder. J Personal Disord. 2009;23:399–409. https://doi.org/10.1521/pedi.2009.23.4.399.
• Bartz J, Simeon D, Hamilton H, Kim S, Crystal S, Braun A, et al. Oxytocin can hinder trust and cooperation in borderline personality disorder. Soc Cogn Affect Neurosci. 2011;6:556–63. https://doi.org/10.1093/scan/nsq085Despite its age, this study remains highly relevant to our understanding of how OXT influences trust process in BPD. Shows that the effect of OXT depends on attachment.
• Ebert A, Kolb M, Heller J, Edel M-A, Roser P, Brüne M. Modulation of interpersonal trust in borderline personality disorder by intranasal oxytocin and childhood trauma. Soc Neurosci. 2013;8:305–13. https://doi.org/10.1080/17470919.2013.807301Despite its age, this study remains highly relevant to our understanding of how OXT influences trust process in BPD. Shows not only that OXT can negatively alter trust in BPD but also that this depends in part on childhood trauma. Also suggests that people with BPD may be using different social cues (i.e., partner attractiveness) to determine trust, which is echoed in more recent work on alterations in social cue responsiveness.
Roberts ID, Krajbich I, Cheavens JS, Campo JV, Way BM. Acetaminophen reduces distrust in individuals with borderline personality disorder features. Clin Psychol Sci. 2018;6:145–54. https://doi.org/10.1177/2167702617731374.
Arntz A, Veen G. Evaluations of Others by Borderline Patients. J Nerv Ment Dis. 2001;189:513–21. https://doi.org/10.1097/00005053-200108000-00004.
Barnow S, Stopsack M, Grabe HJ, Meinke C, Spitzer C, Kronmüller K, et al. Interpersonal evaluation bias in borderline personality disorder. Behav Res Ther. 2009;47:359–65. https://doi.org/10.1016/j.brat.2009.02.003.
Arntz A, Dietzel R, Dreessen L. Assumptions in borderline personality disorder: specificity, stability and relationship with etiological factors. Behav Res Ther. 1999;37:545–57. https://doi.org/10.1016/s0005-7967(98)00152-1.
Downey G, Feldman SI. Implications of rejection sensitivity for intimate relationships. J Pers Soc Psycho. 1996;70:1327–43.
Arntz A, Dreessen L, Schouten E, Weertman A. Beliefs in personality disorders: a test with the personality disorder belief questionnaire. Behav Res Ther. 2004;42:1215–25. https://doi.org/10.1016/j.brat.2003.08.004.
Ayduk Ö, Zayas V, Downey G, Cole AB, Shoda Y, Mischel W. Rejection sensitivity and executive control: joint predictors of borderline personality features. J Res Pers. 2008;42:151–68. https://doi.org/10.1016/j.jrp.2007.04.002.
De Panfilis C, Riva P, Preti E, Cabrino C, Marchesi C. When social inclusion is not enough: implicit expectations of extreme inclusion in borderline personality disorder. Personal Disord. 2015;6:301–9. https://doi.org/10.1037/per0000132.
Fonagy P, Luyten P. A developmental, mentalization-based approach to the understanding and treatment of borderline personality disorder. Dev Psychopathol. 2009;21:1355–81. https://doi.org/10.1017/S0954579409990198.
Meyer-Lindenberg A. Trust me on this. Science. 2008;321:778–80. https://doi.org/10.1126/science.1162908.
Lönnqvist J-E, Verkasalo M, Wichardt PC, Walkowitz G. Personality disorder categories as combinations of dimensions: translating cooperative behavior into the five-factor framework. J Personal Disord. 2012;26:298–304. https://doi.org/10.1521/pedi.2012.26.2.298.
De Dreu CKW, Kret ME. Oxytocin conditions intergroup relations through upregulated in-group empathy, cooperation, conformity, and defense. Biol Psychiatry. 2016;79:165–73. https://doi.org/10.1016/j.biopsych.2015.03.020.
Kosfeld M, Heinrichs M, Zak PJ, Fischbacher U, Fehr E. Oxytocin increases trust in humans. Nature. 2005;435:673–6. https://doi.org/10.1038/nature03701.
Mikolajczak M, Pinon N, Lane A, de Timary P, Luminet O. Oxytocin not only increases trust when money is at stake, but also when confidential information is in the balance. Biol Psychol. 2010;85:182–4. https://doi.org/10.1016/j.biopsycho.2010.05.010.
Clifton A, Pilkonis PA, McCarty C. Social network in borderline personality disorder. J Personal Disord. 2007;21:434–41. https://doi.org/10.1521/pedi.2007.21.4.434.
• Fonagy P, Luyten P, Allison E, Campbell C. What we have changed our minds about: Part 2. Borderline personality disorder, epistemic trust and the developmental significance of social communication. Borderline Personal Disord Emot Dysregul. 2017;4:9. https://doi.org/10.1186/s40479-017-0062-8Discusses the importance of epistemic trust for understanding BPD’s development and potential treatments. Conceptualizes BPD as a disorder of social communication and low resilience. Describes how epistemic trust develops normally and abnormally. Although this work uses different language than the empirical studies, there is significant overlap and potential for integration.
Fonagy P, Luyten P, Allison E. Epistemic petrification and the restoration of epistemic trust: a new conceptualization of borderline personality disorder and its psychosocial treatment. J Personal Disord. 2015;29:575–609. https://doi.org/10.1521/pedi.2015.29.5.575.
Fonagy P, Luyten P, Allison E, Campbell C. What we have changed our minds about: part 1. Borderline personality disorder as a limitation of resilience. Borderline Personal Disord Emot Dysregul. 2017;4:11. https://doi.org/10.1186/s40479-017-0061-9.
Csibra G, Gergely G. Natural pedagogy. Trends Cogn Sci. 2009;13:148–53. https://doi.org/10.1016/j.tics.2009.01.005.
Sperber D, Clément F, Heintz C, Mascaro O, Mercier H, Origgi G, et al. Epistemic vigilance. Mind Lang. 2010;25:359–93. https://doi.org/10.1111/j.1468-0017.2010.01394.x.
Fonagy P, Allison E. The role of mentalizing and epistemic trust in the therapeutic relationship. Psychotherapy. 2014;51:372–80. https://doi.org/10.1037/a0036505.
Luyten P, Campbell C, Fonagy P. Borderline personality disorder, complex trauma, and problems with self and identity: a social-communicative approach. J Pers. 2019;88:88–105. https://doi.org/10.1111/jopy.12483.
Bo S, Sharp C, Beck E, Pedersen J, Gondan M, Simonsen E. First empirical evaluation of outcomes for mentalization-based group therapy for adolescents with BPD. Pers Disord. 2017;8:396–401. https://doi.org/10.1037/per0000210.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
All reported studies/experiments with human or animal subjects performed by the authors have been previously published and complied with all applicable ethical standards (including the Helsinki declaration and its amendments, institutional/national research committee standards, and international/national/institutional guidelines).
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Personality and Impulse Control Disorders
Rights and permissions
About this article
Cite this article
Masland, S.R., Schnell, S.E. & Shah, T.V. Trust Beliefs, Biases, and Behaviors in Borderline Personality Disorder: Empirical Findings and Relevance to Epistemic Trust. Curr Behav Neurosci Rep 7, 239–249 (2020). https://doi.org/10.1007/s40473-020-00220-7
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40473-020-00220-7