Abstract
Purpose
To evaluate the diagnostic accuracy of Gallium-68 prostate-specific membrane antigen positron emission tomography-computed tomography (68Ga-PSMA PET/CT) compared with multiparametric magnetic resonance imaging (mpMRI) for detection of metastatic lymph nodes in intermediate to high-risk prostate cancer (PCa).
Methods
PRISMA-compliant systematic review updated to September 2020 was performed to identify studies that evaluated the diagnostic performance of 68Ga-PSMA PET/CT and mpMRI for detection of metastatic lymph nodes in the same cohort of PCa patients using histopathologic examination as a reference standard. The quality of each study was assessed using the Quality Assessment of Diagnostic Accuracy Studies-2 (QUADAS-2) instrument. STATA version 16.0 was used to obtain the pooled estimates of diagnostic accuracy for per-patient and per-lesion analyses. Heterogeneity in the accuracy estimates was explored by reviewing the generated forest plots, summary receiver operator characteristic (SROC) curves, hierarchical SROC plots, chi-squared test, heterogeneity index, and Spearman’s correlation coefficients.
Results
Six studies, which included 476 patients, met the eligibility criteria for per-patient analysis and four of these studies, reporting data from 4859 dissected lymph nodes, were included in the per-lesion analysis. In the per-patient analysis (N = 6), the pooled sensitivity and specificity for 68Ga-PSMA PET/CT were 0.69 and 0.93, and for mpMRI the pooled sensitivity and specificity were 0.37 and 0.95. In the per-lesion analysis (N = 4), the pooled sensitivity and specificity for 68Ga-PSMA PET/CT were 0.58 and 0.99, and for mpMRI the pooled sensitivity and specificity were 0.44 and 0.99. There was high heterogeneity and a threshold effect in outcomes. A sensitivity analysis demonstrated that the pooled estimates were stable when excluding studies with patient selection concerns, whereas the variances of the pooled estimates became significant, and the characteristics of heterogeneity changed when excluding studies with concerns about index imaging tests.
Conclusion
Both imaging techniques have high specificity for the detection of nodal metastases of PCa. 68Ga-PSMA PET/CT has the advantage of being more sensitive and making it possible to detect distant metastases during the same examination. These modalities may play a complementary role in the diagnosis of PCa. Given the paucity of data and methodological limitations of the included studies, large scale trials are necessary to confirm their clinical values.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Prostate cancer (PCa) is the second most prevalent cancer and the fifth leading cause of cancer death in men worldwide, representing approximately 1.3 million new cases in 2018 [1]. Radical prostatectomy is usually a definitive treatment for PCa with intermediate to high risk [2]. Despite treatment, a significant portion of patients may subsequently suffer from biochemical recurrence due to insufficient identification and localization of metastatic lymph nodes at the time of primary staging using conventional imaging such as computed tomography (CT) and magnetic resonance imaging (MRI). Lymph node status is one of the most important prognostic factors in patients with newly diagnosed PCa. Therefore, there is considerable interest in developing a more PCa-specific and reliable imaging technique with improved utility for detecting metastatic lymph nodes in PCa patients.
In recent updates, clinical guidelines on prostate cancer have recognized the role of multiparametric MRI (mpMRI) in primary staging and biochemical recurrence staging, especially its superior soft-tissue image resolution for primary tumor and lymph node status assessment [3, 4]. However, there is limited recognition of Gallium-68 prostate-specific membrane antigen positron emission tomography computed tomography (68Ga-PSMA PET/CT) despite its potential to improve the diagnostic accuracy for preoperative lymph node staging. PSMA is a transmembrane protein expressed on the surface of prostatic cells. It is selectively overexpressed in PCa lesions, metastatic lymph nodes and bone metastases, and PSMA expression increases with increasing tumor grade and stage [5, 6], and when PCa cells become androgen-independent [7]. Therefore, PSMA has become an invaluable PET imaging biomarker.
A number of studies have shown that 68Ga-PSMA PET/CT is a promising imaging technology not only for lymph node staging but also for early detection of PCa, evaluation of biochemical recurrence, and staging of metastases [8,9,10], which may positively affect clinical decision making and improve patient management in approximately half of the patients [11]. If lymph node metastasis detection rate with 68Ga-PSMA PET/CT can meet current clinical standards, this imaging technique may potentially serve as a tool to both assess the characteristics of the local PCa and test for lymph node metastasis during a single examination. The aim of this study is to conduct a systematic review and meta-analysis to evaluate the diagnostic accuracy of 68Ga-PSMA PET/CT compared with guideline-recommended mpMRI for detection of metastatic lymph nodes in the same cohort of PCa patients.
Methods
Search strategy
This systematic review and meta-analysis followed the Preferred Reporting Items for Systematic Reviews and Meta-Analysis (PRISMA) guidelines [12]. It included original research studies of primary lymph node staging with 68Ga-PSMA PET/CT and mpMRI identified in four electronic databases: MEDLINE, EMBASE, CINAHL, and Cochrane. The combination of subject headings and terms used for querying the databases is in the appendices. Titles and abstracts of the selected original research articles were screened independently by two reviewers. The lists of references of all retrieved studies were also extensively cross-checked.
Eligibility criteria
The study included studies on patients with intermediate to high risk of PCa receiving both 68Ga-PSMA PET/CT and mpMRI for initial lymph node staging of PCa prior to extended pelvic lymph node dissection and definitive histopathologic examination. Both retrospective and prospective observational studies with full-text reports published in English were included. There were no restrictions on the age and ethnicity of patients and the definition of positive lymph nodes in 68Ga-PSMA PET/CT and mpMRI. Duplicate articles, animal studies, cell studies as well as letters, narrative reviews, and conference abstracts were excluded. Studies using alternative PSMA-bound radiotracers (e.g., F-18), using conventional or anatomical MRI, without sufficient raw data to construct a 2 × 2 table or with less than 10 subjects were also excluded.
Data extraction
A study-specific data-extraction spreadsheet was created to record the following data from eligible studies: the name of the first author, country, year of publication, sample size, methods of patient selection, patients’ demographic characteristics, imaging protocols, criteria for detection of positive lymph nodes in index tests, the time interval between index tests and histopathologic examination, and performance characteristics of index tests.
Quality assessment
The quality of the included studies was assessed using QUADAS-2 instrument [13]. The following data were also extracted in the data-extraction spreadsheet: (1) clinical characteristics of the study participants; (2) patient selection (consecutive or not); (3) study type (prospective or retrospective); (3) blinding (blinded or not); (5) verification (e.g. whether all patients or lesions were confirmed by histopathologic examination).
Data synthesis and analysis
Diagnostic accuracy
For each study, binary diagnostic accuracy data were extracted and a 2 × 2 table was constructed to classify patients and lymph nodes into one of four groups: true positives, true negatives, false positives and false negatives. The numbers of positive and negative values were extracted either directly or through a calculation based on reported measures of accuracy. Using 2 × 2 tables, sensitivity and specificity of 68Ga-PSMA PET/CT and mpMRI for per-patient analysis and per-lesion analysis were calculated, respectively. Bivariate meta-analysis methods were applied to generate paired forest plots of sensitivity and specificity with corresponding 95% confidence intervals (CI) using random-effect models to obtain a general overview of the diagnostic accuracy estimates before the interpretation of the pooled results. Summary receiver operating characteristic (SROC) curves were constructed to generate pooled estimates of sensitivity and specificity. To further verify the accuracy of the results, a hierarchical SROC (HSROC) model was used to produce HSROC plots with corresponding 95% confidence regions and prediction regions. HSROC model is currently the most statically rigorous and recommended approach for dealing with a threshold effect while HSROC curves can overcome some of the deficiencies of traditional ROC curves [14,15,16,17,18]. The pooled positive likelihood ratio (PLR), negative likelihood ratio (NLR) and diagnostic odds ratio (DOR) were also calculated.
Heterogeneity investigation
Heterogeneity due to variation between studies or the threshold effect was investigated. For the heterogeneity due to variation between studies, each imaging method was assessed by (1) visual inspection of the paired forest plots for deviation of sensitivity and specificity of each study from the vertical line corresponding to the pooled estimates, (2) visual inspection of HSROC plots for the variability of study estimates, (3) Cochrane’s Q test and chi-squared p values, and (4) the heterogeneity index (I2) with the following cut-off points: 25–50% low heterogeneity; 51–75% moderate heterogeneity; > 75%: high heterogeneity [19].
The heterogeneity due to threshold effect was assessed by (1) visual inspection of SROC plots [14, 20], and (2) the Spearman’s correlation coefficients between sensitivity (logit of the true positive rate) and specificity (logit of the false positive rate) [21].
Sensitivity analysis
Using the QUADAS-2 assessments, each study was classified as high concern if either the risk of bias or the concerns regarding applicability was high or if both of them were considered unclear. Studies were categorized as with or without concerns regarding patients’ selection and reliability of index imaging tests. The pooled estimates of the diagnostic accuracy between 68Ga-PSMA PET/CT and mpMRI were recalculated after excluding studies with concern.
Publication bias
Publication bias was assessed using Deek’s funnel plot asymmetry test. An asymmetric distribution of data points with a p value < 0.05 suggested the presence of publication bias [22].
Statistical software
All statistical analyses were carried out using STATA 16.0 (StataCorp, College Station, TX, USA).
Results
Study selection
In total, 460 studies were identified in the searched databases, including MEDLINE, EMBASE, CINAHL and Cochrane Library. The study identification and reasons for exclusion are summarized in Fig. 1. After removing duplicates, 365 articles were screened using titles and abstracts. Overall, 323 publications were excluded; 250 because they were not related to the subject of the review (e.g. ineligible patients, using different index tests or reference standards) or due to the ineligible publication type. The full-text versions of 42 articles were reviewed, but further 36 papers were excluded, leaving six studies for the meta-analysis [23,24,25,26,27,28].
PRISMA flow diagram. Unreliable data [29]—the reported diagnostic accuracy dose not correspond to the calculated values based on the extracted data
The meta-analysis included six studies, which included 476 patients, for per-patient analysis, and four studies, including in total 4859 dissected lymph nodes, for per-lesion analysis. A summary of the description of the included studies and extracted data is in Tables 1 and 2.
Methodological quality of eligible studies
All include studies were assessed using QUADAS-2 analysis. Figure 2 summarizes the evaluation of the six included studies regarding risk of bias and applicability concerns.
Diagnostic performance of 68Ga-PSMA PET/CT and mpMRI
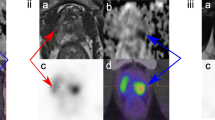
68 Ga-PSMA PET/CT
68Ga-PSMA PET/CT detected 161 (3.3%) positive lymph nodes in 113 (23.7%) patients in six included studies. For per-patient analysis, the pooled sensitivity, pooled specificity, and AUC were 0.69 (95% CI 0.45–0.86), 0.93 (95% CI 0.87–0.96) and 0.94, respectively. For per-lesion analysis, the pooled sensitivity, pooled specificity and AUC were 0.58 (95% CI 0.17–0.9), 0.99 (95% CI 0.98–1) and 0.99, respectively.
In the forest plots, there was large deviation from the pooled estimate for sensitivity, whereas the deviation from the pooled estimate for specificity was small in both analyses (Figs. 3, 4). In the HSROC plots, three studies were outside both confidence and prediction regions in per-patient analysis and the SROC curve was not consistent with each study estimates while no significant outlier point was detected in per-lesion analysis. However, both HSROC plots showed wide confidence and prediction regions (Fig. 5). A heterogeneity test of sensitivity and specificity showed Q = 25.03 (p = 0), I2 = 80.02% and Q = 14.62 (p = 0.01), I2 = 65.79%, respectively, for per-patient analysis and Q = 85.54 (p = 0), I2 = 96.49% and Q = 31.5 (p = 0), I2 = 90.48%, respectively, for per-lesion analysis.
mpMRI
mpMRI detected 125 (2.6%) positive lymph nodes in 57 (12.1%) patients. For per-patient analysis, the pooled sensitivity, pooled specificity and AUC were 0.37 (95% CI 0.15–0.66), 0.95 (95% CI 0.91–0.97) and 0.93, respectively. For per-lesion analysis, the pooled sensitivity, pooled specificity and AUC were 0.44 (95% CI 0.1–0.85), 0.99 (95% CI 0.98–1) and 0.99, respectively.
In the forest plots, there was large deviation from the pooled estimates for sensitivity whereas the deviation from the pooled estimate for specificity was also small in both analyses (Figs. 3, 4). On the HSROC plots, three studies were observed outside confidence region in per-patient analysis and the SROC curve was not consistent with each study estimates while no significant outlier point was detected in per-lesion analysis. However, both HSROC plots also showed wide confidence and prediction regions (Fig. 5). A heterogeneity test of sensitivity and specificity showed Q = 39.31 (p = 0), I2 = 87.28% and Q = 18.79 (p = 0), I2 = 73.39%, respectively, for per-patient analysis and Q = 100.23 (p = 0), I2 = 97.01% and Q = 34.5 (p = 0), I2 = 91.3%, respectively, for per-lesion analysis.
Comparison between two imaging techniques
68Ga-PSMA PET/CT had higher overall detection rate than mpMRI for primary lymph node staging of intermediate to high risk of PCa. The pooled sensitivity was higher in 68Ga-PSMA PET/CT than mpMRI for both per-patient and per-lesion analyses, while the pooled specificity was slightly higher in mpMRI than 68Ga-PSMA PET/CT for per-patient analysis. The reported sensitivities and specificities for both imaging techniques varied across studies; however, the specificities were less variable than the sensitivities.
Overall, there was deviation from the pooled sensitivities and specificities in the forest plots for both 68Ga-PSMA PET/CT and mpMRI. The deviation was larger for sensitivity than specificity. The study estimates for both 68Ga-PSMA PET/CT and mpMRI were scattered in the HSROC plots and the confidence and prediction regions were wide due to insufficient data. Based on the patterns of confidence and prediction regions in HSROC plots and CIs of the summary estimates, the uncertainty in the pooled specificities of both imaging tests was significantly lower than the uncertainty in the pooled sensitivities. The I2 values were either moderate or high and Q test p values were generally low for both sensitivity and specificity of two imaging tests. Notable heterogeneities were present and higher heterogeneity was observed for sensitivity than specificity.
Threshold effect
The patterns of the study estimates in the SROC space did not show a “shoulder arm” shape. The data were, however, insufficient and sparse for visual inspection of threshold effect on the SROC space. Thus, the power to detect threshold effect was low (Appendix II).
The Spearman’s correlation coefficients and p values of 68Ga-PSMA PET/CT and mpMRI for both per-patient and per-lesion analysis were presented in Table 3. Per-patient analysis of mpMRI had a significant and strong positive correlation coefficient of threshold effect.
Sensitivity analysis
The results of sensitivity analysis demonstrated that the pooled estimates were stable after excluding studies with patient selection concerns, whereas the variances of the pooled estimates became significant and the heterogeneity improved after excluding studies with concerns about index imaging tests (Appendix III).
Publication bias
The funnel plots in Fig. 6 showed that the studies were distributed symmetrically with corresponding p values > 0.05 indicating no evidence of publication bias. The number of studies included in the meta-analysis was, however, small with high heterogeneity so the power to detect bias was low (Table 4).
Discussion
Main findings
This review indicated that 68Ga-PSMA PET/CT had a better overall diagnostic performance than mpMRI with a comparable and high specificity but an especially notable superiority of sensitivity. The uncertainty in the diagnostic performance was also lower in 68Ga-PSMA PET/CT than mpMRI. However, the identified studies were heterogeneous and higher heterogeneity was observed in sensitivity than specificity. The sensitivity analysis showed that the lack of blinding regarding the imaging tests might lead to inflated measures of the diagnostic accuracy.
Comparison with previous findings
The results of this meta-analysis are in line with the earlier publications [10, 30]. Our meta-analysis showed that 68Ga-PSMA PET/CT had a higher sensitivity but slightly lower specificity than the earlier review [30]. Several differences between two reviews were noted. Wu et al. combined conventional MRI and mpMRI to produce the pooled estimates, stratified risk of PCa solely based on biopsy results and included studies comparing two imaging techniques in a different cohort of patients. Nevertheless, both of our reviews had significant heterogeneity that we could not determine the sources explicitly. The diagnostic accuracy of 68Ga-PSMA PET/CT for lymph node staging was also found to be similar in the recent and statistically powered meta-analysis with a specificity of 97 and 99% for per-patient and per-lesion analysis, respectively [10].
Strengths and limitations of this review
This study provides a comprehensive review of the current evidence identified through a systematic search on the diagnostic accuracy of 68Ga-PSMA PET/CT and mpMRI for detection of metastatic lymph nodes in the same cohort of PCa patients.
One limitation of this review was the small number of included studies with the few data in the analysis that limited the power of statistical tests. Another limitation was the suboptimal quality of eligible studies, including a suboptimal design regarding reporting of patient selection criteria, independence of test interpretation and reporting of time intervals between individual tests. These are known as review biases that may lead to an overestimation of test accuracy. Furthermore, there might be misclassification of PCa risk since different risk stratification approaches were used in included studies. However, clinical characteristics of patients provided in the studies were incomplete for us to reclassify them and analyses were limited to the use of aggregate data.
Cochrane’s Q test and I2 statistic alone do not account for threshold effect; therefore, we incorporated several approaches to explore heterogeneity in this review. The issue of pre-test probability has been considered especially relevant when conducting tests with an implicit threshold in response to the perception of increased prevalence [31, 32]. In addition, physicians set the level of subjective threshold potentially in response to prior test results. These might also lead to inflated measures of diagnostic accuracy. Hence, the importance of patient selection and the reliability of imaging tests were considered in the sensitivity analysis. The sources of heterogeneity could also be caused by scanner-related issues and imaging protocols applied in different institutions based on their own equipment, capacity and expertise. The included studies using ‘time-of-flight’ advanced technology obtained higher sensitivity than the study using older PET/CT scanners without technical refinements [25,26,27,28]. The variability in diffusion gradient factor b used in DWI sequences of mpMRI made the ranges of ADC values difficult to interpret although the earlier meta-analysis reported no significant differences between electric field strengths (1.5 or 3.0 T) in mpMRI diagnostic performance [30]. The data in the included studies was, however, insufficient to examine those potential sources of heterogeneity for this review.
Given our data limitations and substantial heterogeneity between studies, we cannot ensure the generalizability of the findings to settings with different imaging protocols for PCa patients which might result in different sensitivity and specificity.
Implications for clinical practice
The high specificity of 68Ga-PSMA PET/CT and mpMRI may prove their use as imaging tests to rule in metastatic lymph nodes for PCa patients and avoid over-diagnosis and invasive investigation. However, inadequate sensitivity may limit their use as a screening test for asymptomatic populations. As the findings indicated that the diagnostic accuracy for lymph node staging with 68Ga-PSMA PET/CT meets current clinical standards, it may be reasonable to consider the recommendations for staging and prognosis of PCa to favor 68Ga-PSMA PET/CT as a single whole-body imaging examination.
PSMA provides an excellent target for theranostic application and has become a unique biomarker for both imaging and radionuclide treatment. A number of studies showed promising treatment response of Lutetium-177 PSMA in metastatic castration-resistant PCa patients [33,34,35,36]. Pretreatment selection and therapeutic response are mainly assessed by 68Ga-PSMA PET/CT. Therefore, 68Ga-PSMA PET/CT certainly has an important role in diagnosis, staging as well as treatment of PCa in the near future.
Development of PSMA PET/CT and mpMRI and implications for future researches
Recently, 18Fluorine (18F)-labeled PSMA PET/CT has demonstrated good imaging quality potentially outperforming current imaging modalities with several principle advantages such as minimal radiotracer accumulation in the bladder [37,38,39]. mpMRI for lymph node staging with ultrasmall superparamagnetic iron oxide (USPIO) has also shown promising diagnostic performance in depicting PCa metastatic lymph nodes [40, 41]. However, USPIO is currently not widely available worldwide due to the withdrawal of its license in many regions where its use is limited to research purpose [42]. A sufficient number of high-quality studies regarding 18F-PSMA PET/CT and USPIO-enhanced MRI are warranted to further define the accuracy, capabilities and role in the management of PCa in the future.
Given the lack of studies in the review and those methodological limitations, large scale prospective randomized clinical trials are necessary to confirm the diagnostic performances and clinical values of 68Ga-PSMA PET/CT and mpMRI. To reduce significant heterogeneity and misclassification bias, individual patient data (IPD) meta-analysis can be performed [43, 44]. Line by line patient data are collected and analyzed more similarly from the eligible studies in IPD meta-analysis rather than a standard aggregate meta-analysis and specific subgroups of patients can be assessed across studies.
Conclusions
This review provides valuable insight into the role of 68Ga-PSMA PET/CT and mpMRI in primary lymph node staging of intermediate to high-risk PCa. Both imaging techniques are useful to rule in metastatic lymph nodes due to superior specificity. 68Ga-PSMA PET/CT has a better and more certain overall diagnostic performance for imaging-guided region-based lymph node dissection. These should increase diagnostic impact of 68Ga-PSMA PET/CT in clinical practice and result in a greater acceptance of this imaging technique by molecular imaging community, physicians, patients and funding bodies. However, with the paucity of data from the included studies and all of the methodological issues considered, large scale prospective trials and IPD meta-analysis would need to further confirm the clinical values of these two imaging techniques.
Availability of data and material
The datasets supporting this study are included within the article and appendices.
Code availability
Not applicable.
References
Bray F, Ferlay J, Soerjomataram I, Siegel RL, Torre LA, Jemal A (2018) Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin 68(6):394–424. https://doi.org/10.3322/caac.21492
Bolla M, van Poppel H, Tombal B, Vekemans K, Da Pozzo L, de Reijke TM et al (2012) Postoperative radiotherapy after radical prostatectomy for high-risk prostate cancer: long-term results of a randomised controlled trial (EORTC trial 22911). Lancet 380(9858):2018–2027. https://doi.org/10.1016/S0140-6736(12)61253-7
Mottet N, Bellmunt J, Bolla M, Briers E, Cumberbatch MG, De Santis M et al (2017) EAU-ESTRO-SIOG guidelines on prostate cancer. Part 1: screening, diagnosis, and local treatment with curative intent. Eur Urol 71(4):618–629. https://doi.org/10.1016/j.eururo.2016.08.003
Dasgupta P, Davis J, Hughes S (2019) NICE guidelines on prostate cancer 2019. BJU Int 124(1):1. https://doi.org/10.1111/bju.14815
Sweat SD, Pacelli A, Murphy GP, Bostwick DG (1998) Prostate-specific membrane antigen expression is greatest in prostate adenocarcinoma and lymph node metastases. Urology 52(4):637–640. https://doi.org/10.1016/s0090-4295(98)00278-7
Huang E, Teh BS, Mody DR, Carpenter LS, Butler EB (2003) Prostate adenocarcinoma presenting with inguinal lymphadenopathy. Urology 61(2):463. https://doi.org/10.1016/s0090-4295(02)02269-0
Evans MJ, Smith-Jones PM, Wongvipat J, Navarro V, Kim S, Bander NH, Larson SM, Sawyers CL (2011) Noninvasive measurement of androgen receptor signaling with a positron-emitting radiopharmaceutical that targets prostate-specific membrane antigen. Proc Natl Acad Sci USA 108(23):9578–9582. https://doi.org/10.1073/pnas.1106383108
Demirkol MO, Acar Ö, Uçar B, Ramazanoğlu SR, Sağlıcan Y, Esen T (2015) Prostate-specific membrane antigen-based imaging in prostate cancer: impact on clinical decision making process. Prostate 75(7):748–757. https://doi.org/10.1002/pros.22956
von Eyben FE, Picchio M, von Eyben R, Rhee H, Bauman G (2018) 68Ga-Labeled prostate-specific membrane antigen ligand positron emission tomography/computed tomography for prostate cancer: a systematic review and meta-analysis. Eur Urol Focus 4(5):686–693. https://doi.org/10.1016/j.euf.2016.11.002
Perera M, Papa N, Roberts M, Williams M, Udovicich C, Vela I, Christidis D, Bolton D, Hofman MS, Lawrentschuk N, Murphy DG (2020) Gallium-68 prostate-specific membrane antigen positron emission tomography in advanced prostate cancer-updated diagnostic utility, sensitivity, specificity, and distribution of prostate-specific membrane antigen-avid lesions: a systematic review and meta-analysis. Eur Urol 77(4):403–417. https://doi.org/10.1016/j.eururo.2019.01.049
Han S, Woo S, Kim YJ, Suh CH (2018) Impact of 68Ga-PSMA PET on the management of patients with prostate cancer: a systematic review and meta-analysis. Eur Urol 74(2):179–190. https://doi.org/10.1016/j.eururo.2018.03.030
Liberati A, Altman DG, Tetzlaff J, Mulrow C, Gøtzsche PC, Ioannidis JP, Clarke M, Devereaux PJ, Kleijnen J, Moher D (2009) The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: explanation and elaboration. PLoS Med 6(7):e1000100. https://doi.org/10.1371/journal.pmed.1000100
Whiting PF, Rutjes AW, Westwood ME, Mallett S, Deeks JJ, Reitsma JB, Leeflang MM, Sterne JA, Bossuyt PM; QUADAS-2 Group (2011) QUADAS-2: a revised tool for the quality assessment of diagnostic accuracy studies. Ann Intern Med 155(8):529–536. https://doi.org/10.7326/0003-4819-155-8-201110180-00009
Moses LE, Shapiro D, Littenberg B (1993) Combining independent studies of a diagnostic test into a summary ROC curve: data-analytic approaches and some additional considerations. Stat Med 12(14):1293–1316. https://doi.org/10.1002/sim.4780121403
Rutter CM, Gatsonis CA (2001) A hierarchical regression approach to meta-analysis of diagnostic test accuracy evaluations. Stat Med 20(19):2865–2884. https://doi.org/10.1002/sim.942
Reitsma JB, Glas AS, Rutjes AW, Scholten RJ, Bossuyt PM, Zwinderman AH (2005) Bivariate analysis of sensitivity and specificity produces informative summary measures in diagnostic reviews. J Clin Epidemiol 58(10):982–990. https://doi.org/10.1016/j.jclinepi.2005.02.022
Macaskill P, Gatsonis C, Deeks JJ, Harbord RM, Takwoingi Y (2010) Chapter 10: analysing and presenting results. In: Deeks JJ, Bossuyt PM, Gatsonis C (eds) Cochrane handbook for systematic reviews of diagnostic test accuracy version 1.0. The Cochrane Collaboration. Available from: http://srdta.cochrane.org/
Lee J, Kim KW, Choi SH, Huh J, Park SH (2015) Systematic review and meta-analysis of studies evaluating diagnostic test accuracy: a practical review for clinical researchers—Part II. Statistical methods of meta-analysis. Korean J Radiol 16(6):1188–1196. https://doi.org/10.3348/kjr.2015.16.6.1188
Higgins JP, Thompson SG (2002) Quantifying heterogeneity in a meta-analysis. Stat Med 21(11):1539–1558. https://doi.org/10.1002/sim.1186
Littenberg B, Moses LE (1993) Estimating diagnostic accuracy from multiple conflicting reports: a new meta-analytic method. Med Decis Mak 13(4):313–321. https://doi.org/10.1177/0272989X9301300408
Dinnes J, Deeks J, Kirby J, Roderick P (2005) A methodological review of how heterogeneity has been examined in systematic reviews of diagnostic test accuracy. Health Technol Assess 9(12):1–113. https://doi.org/10.3310/hta9120
Song F, Khan KS, Dinnes J, Sutton AJ (2002) Asymmetric funnel plots and publication bias in meta-analyses of diagnostic accuracy. Int J Epidemiol 31(1):88–95. https://doi.org/10.1093/ije/31.1.88
Gupta M, Choudhury PS, Hazarika D, Rawal S (2017) A comparative study of 68gallium-prostate specific membrane antigen positron emission tomography-computed tomography and magnetic resonance imaging for lymph node staging in high risk prostate cancer patients: an initial experience. World J Nucl Med 16(3):186–191. https://doi.org/10.4103/1450-1147.207272
Zhang Q, Zang S, Zhang C, Fu Y, Lv X, Zhang Q, Deng Y, Zhang C, Luo R, Zhao X, Wang W, Wang F, Guo H (2017) Comparison of 68 Ga-PSMA-11 PET-CT with mpMRI for preoperative lymph node staging in patients with intermediate to high-risk prostate cancer. J Transl Med 15(1):230. https://doi.org/10.1186/s12967-017-1333-2
van Leeuwen PJ, Donswijk M, Nandurkar R, Stricker P, Ho B, Heijmink S, Wit EMK, Tillier C, van Muilenkom E, Nguyen Q, van der Poel HG, Emmett L (2019) Gallium-68-prostate-specific membrane antigen (68Ga-PSMA) positron emission tomography (PET)/ computed tomography (CT) predicts complete biochemical response from radical prostatectomy and lymph node dissection in intermediate- and high-risk prostate cancer. BJU Int 124(1):62–68. https://doi.org/10.1111/bju.14506
Franklin A, Yaxley WJ, Raveenthiran S, Coughlin G, Gianduzzo T, Kua B, McEwan L, Wong D, Delahunt B, Egevad L, Samaratunga H, Brown N, Parkinson R, Roberts MJ, Yaxley JW (2021) Histological comparison between predictive value of preoperative 3-T multiparametric MRI and 68 Ga-PSMA PET/CT scan for pathological outcomes at radical prostatectomy and pelvic lymph node dissection for prostate cancer. BJU Int 127(1):71–79. https://doi.org/10.1111/bju.15134
Pallavi UN, Gogoi S, Thakral P, Malasani V, Sharma K, Manda D, Das SS, Pant V, Sen I (2020) Incremental value of Ga-68 prostate-specific membrane antigen-11 positron-emission tomography/computed tomography scan for preoperative risk stratification of prostate cancer. Indian J Nucl Med 35(2):93–99. https://doi.org/10.4103/ijnm.IJNM_189_19
Petersen LJ, Nielsen JB, Langkilde NC, Petersen A, Afshar-Oromieh A, De Souza NM, De Paepe K, Fisker RV, Arp DT, Carl J, Haberkorn U, Zacho HD (2020) 68Ga-PSMA PET/CT compared with MRI/CT and diffusion-weighted MRI for primary lymph node staging prior to definitive radiotherapy in prostate cancer: a prospective diagnostic test accuracy study. World J Urol 38(4):939–948. https://doi.org/10.1007/s00345-019-02846-z
Yilmaz B, Turkay R, Colakoglu Y, Baytekin HF, Ergul N, Sahin S, Tugcu V, Inci E, Tasci AI, Cermik TF (2019) Comparison of preoperative locoregional Ga-68 PSMA-11 PET-CT and mp-MRI results with postoperative histopathology of prostate cancer. Prostate 79(9):1007–1017. https://doi.org/10.1002/pros.23812
Wu H, Xu T, Wang X, Yu YB, Fan ZY, Li DX, Luo L, Yang XC, Jiao W, Niu HT (2020) Diagnostic performance of 68gallium labelled prostate-specific membrane antigen positron emission tomography/computed tomography and magnetic resonance imaging for staging the prostate cancer with intermediate or high risk prior to radical prostatectomy: a systematic review and meta-analysis. World J Men’s Health 38(2):208–219. https://doi.org/10.5534/wjmh.180124
Leeflang MM, Bossuyt PM, Irwig L (2009) Diagnostic test accuracy may vary with prevalence: implications for evidence-based diagnosis. J Clin Epidemiol 62(1):5–12. https://doi.org/10.1016/j.jclinepi.2008.04.007
Willis BH (2012) Empirical evidence that disease prevalence may affect the performance of diagnostic tests with an implicit threshold: a cross-sectional study. BMJ Open 2(1):e000746. https://doi.org/10.1136/bmjopen-2011-000746
Rahbar K, Boegemann M, Yordanova A, Eveslage M, Schäfers M, Essler M, Ahmadzadehfar H (2018) PSMA targeted radioligandtherapy in metastatic castration resistant prostate cancer after chemotherapy, abiraterone and/or enzalutamide. A retrospective analysis of overall survival. Eur J Nucl Med Mol Imaging 45(1):12–19. https://doi.org/10.1007/s00259-017-3848-4
Ferdinandus J, Eppard E, Gaertner FC, Kürpig S, Fimmers R, Yordanova A, Hauser S, Feldmann G, Essler M, Ahmadzadehfar H (2017) Predictors of response to radioligand therapy of metastatic castrate-resistant prostate cancer with 177Lu-PSMA-617. J Nucl Med 58(2):312–319. https://doi.org/10.2967/jnumed.116.178228
Yadav MP, Ballal S, Tripathi M, Damle NA, Sahoo RK, Seth A, Bal C (2017) 177Lu-DKFZ-PSMA-617 therapy in metastatic castration resistant prostate cancer: safety, efficacy, and quality of life assessment. Eur J Nucl Med Mol Imaging 44(1):81–91. https://doi.org/10.1007/s00259-016-3481-7
Rathke H, Giesel FL, Flechsig P, Kopka K, Mier W, Hohenfellner M, Haberkorn U, Kratochwil C (2018) Repeated 177Lu-labeled PSMA-617 radioligand therapy using treatment activities of up to 9.3 GBq. J Nucl Med 59(3):459–465. https://doi.org/10.2967/jnumed.117.194209
Rahbar K, Afshar-Oromieh A, Seifert R, Wagner S, Schäfers M, Bögemann M, Weckesser M (2018) Diagnostic performance of 18F-PSMA-1007 PET/CT in patients with biochemical recurrent prostate cancer. Eur J Nucl Med Mol Imaging 45(12):2055–2061. https://doi.org/10.1007/s00259-018-4089-x
Rauscher I, Krönke M, König M, Gafita A, Maurer T, Horn T, Schiller K, Weber W, Eiber M (2020) Matched-pair comparison of 68Ga-PSMA-11 PET/CT and 18F-PSMA-1007 PET/CT: frequency of pitfalls and detection efficacy in biochemical recurrence after radical prostatectomy. J Nucl Med 61(1):51–57. https://doi.org/10.2967/jnumed.119.229187
Werner RA, Derlin T, Lapa C, Sheikbahaei S, Higuchi T, Giesel FL, Behr S, Drzezga A, Kimura H, Buck AK, Bengel FM, Pomper MG, Gorin MA, Rowe SP (2020) 18F-labeled, PSMA-targeted radiotracers: leveraging the advantages of radiofluorination for prostate cancer molecular imaging. Theranostics 10(1):1–16. https://doi.org/10.7150/thno.37894
Harisinghani MG, Barentsz J, Hahn PF, Deserno WM, Tabatabaei S, van de Kaa CH, de la Rosette J, Weissleder R (2003) Noninvasive detection of clinically occult lymph-node metastases in prostate cancer. N Engl J Med 348(25):2491–2499. https://doi.org/10.1056/NEJMoa022749
Wu L, Cao Y, Liao C, Huang J, Gao F (2011) Diagnostic performance of USPIO-enhanced MRI for lymph-node metastases in different body regions: a meta-analysis. Eur J Radiol 80(2):582–589. https://doi.org/10.1016/j.ejrad.2009.11.027
Fortuin AS, Brüggemann R, van der Linden J, Panfilov I, Israël B, Scheenen TWJ, Barentsz JO (2018) Ultra-small superparamagnetic iron oxides for metastatic lymph node detection: back on the block. Wiley Interdiscip Rev Nanomed Nanobiotechnol 10(1):e1471. https://doi.org/10.1002/wnan.1471
Riley RD, Lambert PC, Abo-Zaid G (2010) Meta-analysis of individual participant data: rationale, conduct, and reporting. BMJ (Clin Res Ed) 340:c221. https://doi.org/10.1136/bmj.c221
Thomas D, Radji S, Benedetti A (2014) Systematic review of methods for individual patient data meta-analysis with binary outcomes. BMC Med Res Methodol 14:79. https://doi.org/10.1186/1471-2288-14-79
Funding
All authors state that this work has not received any funding.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
All authors have no conflicts of interest to declare that are relevant to the content of this article.
Ethics approval
Not applicable. This article does not contain any studies with human or animal subjects performed by any of the authors.
Consent to participate
Not applicable.
Consent for publication
Not applicable.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Yip, K.C.J., Li, YL., Chen, S. et al. 68Ga-PSMA PET/CT and mpMRI for primary lymph node staging of intermediate to high-risk prostate cancer: a systematic review and meta-analysis of diagnostic test accuracy. Clin Transl Imaging 9, 523–537 (2021). https://doi.org/10.1007/s40336-021-00453-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40336-021-00453-w