Abstract
Radiotheragnostics represents the systematic integration of diagnostic imaging and therapeutics using radionuclides targeting specific characteristics of tumor biology. Radioiodine (131I) is the classic radiotheragnostic agent used for the diagnosis and treatment of differentiated thyroid cancer based on sodium-iodine symporter expression in normal and neoplastic thyroid tissue. Application of radiotheragnostics principles in thyroid cancer involves using pre-ablation diagnostic scans (Dx Scans) for detection of iodine-avid regional and distant metastatic disease and patient-individualized targeted 131I therapy with goal of maximizing the benefits of the first therapeutic 131I administration. Clinically available nuclear medicine imaging technology has significantly evolved over the past 10 years with the introduction of hybrid SPECT/CT and PET/CT systems, as well as advances in iterative image reconstruction with modeling of image degrading physical factors. This progress makes possible the acquisition of accurate diagnostic radioiodine scintigraphy capable of identifying regional and distant metastatic disease, which can be used for 131I treatment planning and delivery of activity adjusted 131I therapy for achieving intended treatment goals (e.g., remnant ablation, adjuvant 131I treatment and targeted 131-I treatment). The overarching aim of thyroid cancer radiotheragnostics is to optimize the balance between 131I therapeutic efficacy and potential side-effects on non-target tissues.
Similar content being viewed by others
Abbreviations
- Anti-Tg Ab:
-
Anti-thyroglobulin antibody
- ATA:
-
American Thyroid Association
- DTC:
-
Differentiated thyroid cancer
- Dx Scan:
-
Diagnostic 131I scan with single-photon emission computer tomography (SPECT) with inline computed tomography (CT) SPECT/CT
- ETE:
-
Extra-thyroidal extension
- L-T4:
-
Levothyroxine
- Post-Rx scan:
-
Post-therapy 131I scan
- PTC:
-
Papillary thyroid cancer
- Tg:
-
Thyroglobulin
- THW:
-
Thyroid hormone withdrawal
References
Pacini F, Schlumberger M, Dralle H, Elisei R, Smit JW, Wiersinga W (2006) European consensus for the management of patients with differentiated thyroid carcinoma of the follicular epithelium. Eur J Endocrinol 154(6):787–803
Schlumberger MJ, Pacini F (2009) The low utility of pretherapy scans in thyroid cancer patients. Thyroid 19(8):815–816
Deandreis D, Rubino C, Tala H, Leboulleux S, Terroir M, Baudin E, et al. (2016) Comparison of empiric versus whole body/blood clearance dosimetry-based approach to radioactive iodine treatment in patients with metastases from differentiated thyroid cancer. J Nucl Med
Beierwaltes WH, Rabbani R, Dmuchowski C, Lloyd RV, Eyre P, Mallette S (1984) An analysis of “ablation of thyroid remnants” with I-131 in 511 patients from 1947-1984: experience at University of Michigan. J Nucl Med 25(12):1287–1293
Pacini F, Schlumberger M, Harmer C, Berg GG, Cohen O, Duntas L et al (2005) Post-surgical use of radioiodine (131I) in patients with papillary and follicular thyroid cancer and the issue of remnant ablation: a consensus report. Eur J Endocrinol 153(5):651–659
Schlumberger M, Borget I, Nascimento C, Brassard M, Leboulleux S (2011) Treatment and follow-up of low-risk patients with thyroid cancer. Nat Rev Endocrinol 7(10):625–628
Cooper DS, Doherty GM, Haugen BR, Kloos RT, American Thyroid Association Guidelines Taskforce on Thyroid N, Differentiated Thyroid C et al (2009) Revised American Thyroid Association management guidelines for patients with thyroid nodules and differentiated thyroid cancer. Thyroid 19(11):1167–1214
Haugen BR, Alexander EK, Bible KC, Doherty GM, Mandel SJ, Nikiforov YE et al (2016) 2015 American Thyroid Association Management Guidelines for Adult Patients with Thyroid Nodules and Differentiated Thyroid Cancer: The American Thyroid Association guidelines task force on thyroid nodules and differentiated thyroid cancer. Thyroid. 26(1):1–133
Zerdoud S, Giraudet AL, Leboulleux S, Leenhardt L, Bardet S, Clerc J et al (2017) Radioactive iodine therapy, molecular imaging and serum biomarkers for differentiated thyroid cancer: 2017 guidelines of the French Societies of Nuclear Medicine, Endocrinology, Pathology, Biology, Endocrine Surgery and Head and Neck Surgery. Ann Endocrinol (Paris) 78(3):162–175
Jeevanram RK, Shah DH, Sharma SM, Ganatra RD (1986) Influence of initial large dose on subsequent uptake of therapeutic radioiodine in thyroid cancer patients. Int J Rad Appl Instrum B. 13(3):277–279
Huic D, Medvedec M, Dodig D, Popovic S, Ivancevic D, Pavlinovic Z et al (1996) Radioiodine uptake in thyroid cancer patients after diagnostic application of low-dose 131I. Nucl Med Commun 17(10):839–842
Yeung HW, Humm JL, Larson SM (2000) Radioiodine uptake in thyroid remnants during therapy after tracer dosimetry. J Nucl Med 41(6):1082–1085
Morris LF, Waxman AD, Braunstein GD (2001) The nonimpact of thyroid stunning: remnant ablation rates in 131I-scanned and nonscanned individuals. J Clin Endocrinol Metab 86(8):3507–3511
McDougall IR (1997) 74 MBq radioiodine 131I does not prevent uptake of therapeutic doses of 131I (i.e. it does not cause stunning) in differentiated thyroid cancer. Nucl Med Commun 18(6):505–512
Cholewinski SP, Yoo KS, Klieger PS, O’Mara RE (2000) Absence of thyroid stunning after diagnostic whole-body scanning with 185 MBq 131I. J Nucl Med 41(7):1198–1202
Karam M, Gianoukakis A, Feustel PJ, Cheema A, Postal ES, Cooper JA (2003) Influence of diagnostic and therapeutic doses on thyroid remnant ablation rates. Nucl Med Commun 24(5):489–495
Rosario PW, Barroso AL, Rezende LL, Padrao EL, Maia FF, Fagundes TA et al (2005) 5 mCi pretreatment scanning does not cause stunning when the ablative dose is administered within 72 hours. Arq Bras Endocrinol Metabol 49(3):420–424
Sisson JC, Avram AM, Lawson SA, Gauger PG, Doherty GM (2006) The so-called stunning of thyroid tissue. J Nucl Med 47(9):1406–1412
Silberstein EB (2007) Comparison of outcomes after (123)I versus (131)I pre-ablation imaging before radioiodine ablation in differentiated thyroid carcinoma. J Nucl Med 48(7):1043–1046
McDougall IR, Iagaru A (2011) Thyroid stunning: fact or fiction? Semin Nucl Med 41(2):105–112
Waxman A, Ramanna L, Chapman N, Chapman D, Brachman M, Tanasescu D et al (1981) The significance of 1-131 scan dose in patients with thyroid cancer: determination of ablation: concise communication. J Nucl Med 22(10):861–865
Schlumberger M, Arcangioli O, Piekarski JD, Tubiana M, Parmentier C (1988) Detection and treatment of lung metastases of differentiated thyroid carcinoma in patients with normal chest X-rays. J Nucl Med 29(11):1790–1794
Siddiqi A, Foley RR, Britton KE, Sibtain A, Plowman PN, Grossman AB et al (2001) The role of 123I-diagnostic imaging in the follow-up of patients with differentiated thyroid carcinoma as compared to 131I-scanning: avoidance of negative therapeutic uptake due to stunning. Clin Endocrinol (Oxf) 55(4):515–521
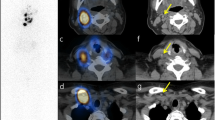
Avram AM, Fig LM, Frey KA, Gross MD, Wong KK (2013) Preablation 131-I scans with SPECT/CT in postoperative thyroid cancer patients: what is the impact on staging? J Clin Endocrinol Metab 98(3):1163–1171
Park EK, Chung JK, Lim IH, Park DJ, Lee DS, Lee MC et al (2009) Recurrent/metastatic thyroid carcinomas false negative for serum thyroglobulin but positive by posttherapy I-131 whole body scans. Eur J Nucl Med Mol Imaging. 36(2):172–179
Campenni A, Giovanella L, Pignata SA, Vento A, Alibrandi A, Sturiale L et al (2018) Undetectable or low (< 1 ng/ml) postsurgical thyroglobulin values do not rule out metastases in early stage differentiated thyroid cancer patients. Oncotarget 9(25):17491–17500
Verburg FA, Mader U, Giovanella L, Luster M, Reiners C (2018) Low or undetectable basal thyroglobulin levels obviate the need for neck ultrasound in differentiated thyroid cancer patients after total thyroidectomy and (131)I ablation. Thyroid. 28(6):722–728
Hindie E, Zanotti-Fregonara P, Keller I, Duron F, Devaux JY, Calzada-Nocaudie M et al (2007) Bone metastases of differentiated thyroid cancer: impact of early 131I-based detection on outcome. Endocr Relat Cancer 14(3):799–807
Albano D, Bertagna F, Bonacina M, Durmo R, Cerudelli E, Gazzilli M, et al. (2018) Possible delayed diagnosis and treatment of metastatic differentiated thyroid cancer by adopting the 2015 ATA guidelines. Eur J Endocrinol
Edge SB BD, Compton CC, Fritz AG, Greene FL, Trotti A (eds) (2010) AJCC cancer staging manual. 7th edon. Springer, p 646
Brierley JD, Gospodarowicz MK, Wittekind C (2016) TNM classification of malignant tumors. Wiley, Oxford
American Cancer Society I. Key Statistics Thyroid Cancer 2014
Clerc J, Verburg FA, Avram AM, Giovanella L, Hindie E, Taieb D (2017) Radioiodine treatment after surgery for differentiated thyroid cancer: a reasonable option. Eur J Nucl Med Mol Imag 44(6):918–925
Mazzaferri EL, Kloos RT (2001) Clinical review 128: current approaches to primary therapy for papillary and follicular thyroid cancer. J Clin Endocrinol Metab 86(4):1447–1463
Loh KC, Greenspan FS, Gee L, Miller TR, Yeo PP (1997) Pathological tumor-node-metastasis (pTNM) staging for papillary and follicular thyroid carcinomas: a retrospective analysis of 700 patients. J Clin Endocrinol Metab 82(11):3553–3562
Samaan NA, Schultz PN, Hickey RC, Goepfert H, Haynie TP, Johnston DA et al (1992) The results of various modalities of treatment of well differentiated thyroid carcinomas: a retrospective review of 1599 patients. J Clin Endocrinol Metab 75(3):714–720
Sawka AM, Thephamongkhol K, Brouwers M, Thabane L, Browman G, Gerstein HC (2004) Clinical review 170: a systematic review and metaanalysis of the effectiveness of radioactive iodine remnant ablation for well-differentiated thyroid cancer. J Clin Endocrinol Metab 89(8):3668–3676
Jonklaas J, Sarlis NJ, Litofsky D, Ain KB, Bigos ST, Brierley JD et al (2006) Outcomes of patients with differentiated thyroid carcinoma following initial therapy. Thyroid 16(12):1229–1242
Carhill AA, Litofsky DR, Ross DS, Jonklaas J, Cooper DS, Brierley JD et al (2015) Long-term outcomes following therapy in differentiated thyroid carcinoma: NTCTCS registry analysis 1987–2012. J Clin Endocrinol Metab 100(9):3270–3279
Avram AM, Esfandiari NH, Wong KK (2015) Preablation 131-I scans with SPECT/CT contribute to thyroid cancer risk stratification and 131-I therapy planning. J Clin Endocrinol Metab 100(5):1895–1902
Verburg FA, Mader U, Reiners C, Hanscheid H (2014) Long-term survival in differentiated thyroid cancer is worse after low-activity initial post-surgical 131I therapy in both high- and low-risk patients. J Clin Endocrinol Metab 99(12):4487–4496
Bal C, Chandra P, Kumar A, Dwivedi S (2012) A randomized equivalence trial to determine the optimum dose of iodine-131 for remnant ablation in differentiated thyroid cancer. Nucl Med Commun 33(10):1039–1047
Bal C, Padhy AK, Jana S, Pant GS, Basu AK (1996) Prospective randomized clinical trial to evaluate the optimal dose of 131 I for remnant ablation in patients with differentiated thyroid carcinoma. Cancer 77(12):2574–2580
Rosario PW, Reis JS, Barroso AL, Rezende LL, Padrao EL, Fagundes TA (2004) Efficacy of low and high 131I doses for thyroid remnant ablation in patients with differentiated thyroid carcinoma based on post-operative cervical uptake. Nucl Med Commun 25(11):1077–1081
Hodgson DC, Brierley JD, Tsang RW, Panzarella T (1998) Prescribing 131Iodine based on neck uptake produces effective thyroid ablation and reduced hospital stay. Radiother Oncol 47(3):325–330
Johansen K, Woodhouse NJ, Odugbesan O (1991) Comparison of 1073 MBq and 3700 MBq iodine-131 in postoperative ablation of residual thyroid tissue in patients with differentiated thyroid cancer. J Nucl Med 32(2):252–254
Logue JP, Tsang RW, Brierley JD, Simpson WJ (1994) Radioiodine ablation of residual tissue in thyroid cancer: relationship between administered activity, neck uptake and outcome. Br J Radiol 67(803):1127–1131
Zaman M, Toor R, Kamal S, Maqbool M, Habib S, Niaz K (2006) A randomized clinical trial comparing 50 mCi and 100 mCi of iodine-131 for ablation of differentiated thyroid cancers. J Pak Med Assoc 56(8):353–356
Cherk MH, Kalff V, Yap KS, Bailey M, Topliss D, Kelly MJ (2008) Incidence of radiation thyroiditis and thyroid remnant ablation success rates following 1110 MBq (30 mCi) and 3700 MBq (100 mCi) post-surgical 131I ablation therapy for differentiated thyroid carcinoma. Clin Endocrinol (Oxf) 69(6):957–962
Maenpaa HO, Heikkonen J, Vaalavirta L, Tenhunen M, Joensuu H (2008) Low vs. high radioiodine activity to ablate the thyroid after thyroidectomy for cancer: a randomized study. PLoS ONE 3(4):e1885
Pilli T, Brianzoni E, Capoccetti F, Castagna MG, Fattori S, Poggiu A et al (2007) A comparison of 1850 (50 mCi) and 3700 MBq (100 mCi) 131-iodine administered doses for recombinant thyrotropin-stimulated postoperative thyroid remnant ablation in differentiated thyroid cancer. J Clin Endocrinol Metab 92(9):3542–3546
Schlumberger M, Catargi B, Borget I, Deandreis D, Zerdoud S, Bridji B et al (2012) Strategies of radioiodine ablation in patients with low-risk thyroid cancer. N Engl J Med 366(18):1663–1673
Mallick U, Harmer C, Yap B, Wadsley J, Clarke S, Moss L et al (2012) Ablation with low-dose radioiodine and thyrotropin alfa in thyroid cancer. N Engl J Med 366(18):1674–1685
Du P, Jiao X, Zhou Y, Li Y, Kang S, Zhang D et al (2015) Low versus high radioiodine activity to ablate the thyroid after thyroidectomy for cancer: a meta-analysis of randomized controlled trials. Endocrine 48(1):96–105
Doi SA, Woodhouse NJ (2000) Ablation of the thyroid remnant and 131I dose in differentiated thyroid cancer. Clin Endocrinol (Oxf) 52(6):765–773
Van Nostrand D (2009) The benefits and risks of I-131 therapy in patients with well-differentiated thyroid cancer. Thyroid 19(12):1381–1391
Castagna MG, Cevenini G, Theodoropoulou A, Maino F, Memmo S, Claudia C et al (2013) Post-surgical thyroid ablation with low or high radioiodine activities results in similar outcomes in intermediate risk differentiated thyroid cancer patients. Eur J Endocrinol 169(1):23–29
Kruijff S, Aniss AM, Chen P, Sidhu SB, Delbridge LW, Robinson B et al (2013) Decreasing the dose of radioiodine for remnant ablation does not increase structural recurrence rates in papillary thyroid carcinoma. Surgery. 154(6):1337–1344 (discussion 44-5)
Maxon HR 3rd, Englaro EE, Thomas SR, Hertzberg VS, Hinnefeld JD, Chen LS et al (1992) Radioiodine-131 therapy for well-differentiated thyroid cancer–a quantitative radiation dosimetric approach: outcome and validation in 85 patients. J Nucl Med 33(6):1132–1136
Maxon HR, Thomas SR, Hertzberg VS, Kereiakes JG, Chen IW, Sperling MI et al (1983) Relation between effective radiation dose and outcome of radioiodine therapy for thyroid cancer. N Engl J Med 309(16):937–941
Maxon HR, Thomas SR, Samaratunga RC (1997) Dosimetric considerations in the radioiodine treatment of macrometastases and micrometastases from differentiated thyroid cancer. Thyroid 7(2):183–187
Jentzen W, Hoppenbrouwers J, van Leeuwen P, van der Velden D, van de Kolk R, Poeppel TD et al (2014) Assessment of lesion response in the initial radioiodine treatment of differentiated thyroid cancer using 124I PET imaging. J Nucl Med 55(11):1759–1765
Jentzen W, Verschure F, van Zon A, van de Kolk R, Wierts R, Schmitz J et al (2016) 124I PET assessment of response of bone metastases to initial radioiodine treatment of differentiated thyroid cancer. J Nucl Med 57(10):1499–1504
Benua RS, Cicale NR, Sonenberg M, Rawson RW (1962) The relation of radioiodine dosimetry to results and complications in the treatment of metastatic thyroid cancer. Am J Roentgenol Radium Ther Nucl Med 87:171–182
Lassmann M, Hanscheid H, Chiesa C, Hindorf C, Flux G, Luster M et al (2008) EANM Dosimetry Committee series on standard operational procedures for pre-therapeutic dosimetry I: blood and bone marrow dosimetry in differentiated thyroid cancer therapy. Eur J Nucl Med Mol Imag 35(7):1405–1412
Luster M, Clarke SE, Dietlein M, Lassmann M, Lind P, Oyen WJ et al (2008) Guidelines for radioiodine therapy of differentiated thyroid cancer. Eur J Nucl Med Mol Imag 35(10):1941–1959
Dewaraja YK, Frey EC, Sgouros G, Brill AB, Roberson P, Zanzonico PB et al (2012) MIRD pamphlet no. 23: quantitative SPECT for patient-specific 3-dimensional dosimetry in internal radionuclide therapy. J Nucl Med 53(8):1310–1325
Maxon HR 3rd, Smith HS (1990) Radioiodine-131 in the diagnosis and treatment of metastatic well differentiated thyroid cancer. Endocrinol Metab Clin North Am 19(3):685–718
Dewaraja YK, Ljungberg M, Green AJ, Zanzonico PB, Frey EC, Committee SM et al (2013) MIRD pamphlet no. 24: Guidelines for quantitative 131I SPECT in dosimetry applications. J Nucl Med 54(12):2182–2188
Jentzen W, Freudenberg L, Bockisch A (2011) Quantitative imaging of (124)I with PET/CT in pretherapy lesion dosimetry. Effects impairing image quantification and their corrections. Q J Nucl Med Mol Imag 55(1):21–43
Avram AM (2012) Radioiodine scintigraphy with SPECT/CT: an important diagnostic tool for thyroid cancer staging and risk stratification. J Nucl Med 53(5):754–764
Wong KK, Sisson JC, Koral KF, Frey KA, Avram AM (2010) Staging of differentiated thyroid carcinoma using diagnostic 131I SPECT/CT. AJR Am J Roentgenol 195(3):730–736
Wong KK, Zarzhevsky N, Cahill JM, Frey KA, Avram AM (2008) Incremental value of diagnostic 131I SPECT/CT fusion imaging in the evaluation of differentiated thyroid carcinoma. AJR Am J Roentgenol 191(6):1785–1794
Van Nostrand D, Aiken M, Atkins F, Moreau S, Garcia C, Acio E et al (2009) The utility of radioiodine scans prior to iodine 131 ablation in patients with well-differentiated thyroid cancer. Thyroid 19(8):849–855
Durante C, Haddy N, Baudin E, Leboulleux S, Hartl D, Travagli JP et al (2006) Long-term outcome of 444 patients with distant metastases from papillary and follicular thyroid carcinoma: benefits and limits of radioiodine therapy. J Clin Endocrinol Metab 91(8):2892–2899
Schmidt D, Linke R, Uder M, Kuwert T (2010) Five months’ follow-up of patients with and without iodine-positive lymph node metastases of thyroid carcinoma as disclosed by (131)I-SPECT/CT at the first radioablation. Eur J Nucl Med Mol Imag 37(4):699–705
Avram AM, Doherty GM, Fig LM, Wong K (2011) Diagnostic 131-I fusion SPECT-CT imaging in postoperative thyroid cancer patients: what is the impact on staging? Thyroid 21(S1):193
Sisson JC (2002) Practical dosimetry of 131I in patients with thyroid carcinoma. Cancer Biother Radiopharm 17(1):101–105
Sisson JC, Shulkin BL, Lawson S (2003) Increasing efficacy and safety of treatments of patients with well-differentiated thyroid carcinoma by measuring body retentions of 131I. J Nucl Med 44(6):898–903
Van Nostrand D, Atkins F, Yeganeh F, Acio E, Bursaw R, Wartofsky L (2002) Dosimetrically determined doses of radioiodine for the treatment of metastatic thyroid carcinoma. Thyroid 12(2):121–134
Van Nostrand D (2016) To perform or not to perform radioiodine scans prior to 131I remnant ablation? PRO. In: Wartofsky L, Van Nostrand D (eds) Thyroid cancer: a comprehensive guide to clinical management. Springer, New York, pp p245–p254
Verburg FA, Lassmann M, Mader U, Luster M, Reiners C, Hanscheid H (2011) The absorbed dose to the blood is a better predictor of ablation success than the administered 131I activity in thyroid cancer patients. Eur J Nucl Med Mol Imag 38(4):673–680
Sgouros G, Hobbs RF, Atkins FB, Van Nostrand D, Ladenson PW, Wahl RL (2011) Three-dimensional radiobiological dosimetry (3D-RD) with 124I PET for 131I therapy of thyroid cancer. Eur J Nucl Med Mol Imag 38(Suppl 1):S41–S47
Wierts R, Brans B, Havekes B, Kemerink GJ, Halders SG, Schaper NN et al (2016) Dose–response relationship in differentiated thyroid cancer patients undergoing radioiodine treatment assessed by means of 124I PET/CT. J Nucl Med 57(7):1027–1032
Hindie E, Melliere D, Lange F, Hallaj I, de Labriolle-Vaylet C, Jeanguillaume C et al (2003) Functioning pulmonary metastases of thyroid cancer: does radioiodine influence the prognosis? Eur J Nucl Med Mol Imag 30(7):974–981
Melliere D, Hindie E, Becquemin JP, Desgranges P, Allaire E, Geachan E (2006) Differentiated thyroid carcinoma—how to improve the long-term results? Twenty-five-year outcomes of 850 patients. Bull Acad Natl Med 190(1):89–106 (discussion-9)
Funding
The authors have received funding support 2-R01-EB-001994 awarded by the National Institute of Biomedical Imaging and Bioengineering, National Institute of Health, U.S. Department of Health and Human Services.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors have no conflicts of interest or financial disclosure
Ethical standard
This article does not contain any studies with human or animal subjects performed by any of the authors.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Avram, A.M., Dewaraja, Y.K. Thyroid cancer radiotheragnostics: the case for activity adjusted 131I therapy. Clin Transl Imaging 6, 335–346 (2018). https://doi.org/10.1007/s40336-018-0291-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40336-018-0291-x