Abstract
Introduction
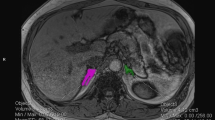
Primary aldosteronism (PA) is a common disease. Especially in unilateral PA (UPA), the risk of cardiovascular disease is high and proper localization is important. Adrenal vein sampling (AVS) is commonly used to localize PA, but its availability is limited. Therefore, it is important to predict the unilateral or bilateral PA and to choose the appropriate cases for AVS or watchful observation.
Aim
The purpose of this study is to develop a model using machine learning to predict bilateral or unilateral PA to extract cases for AVS or watchful observation.
Methods
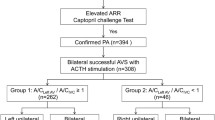
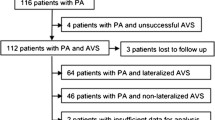
We retrospectively analyzed 154 patients diagnosed with PA and who underwent AVS at our hospital between January 2010 and June 2021. Based on machine learning, we determined predictors of PA subtypes diagnosis from the results of blood and loading tests.
Results
The accuracy of the machine learning was 88% and the top predictors of the UPA were plasma aldosterone concentration after the saline infusion test, aldosterone to renin ratio after the captopril challenge test, serum potassium and aldosterone-to-renin ratio. By using these factors, the accuracy, sensitivity, specificity and the area under the curve (AUC) were 91%, 70%, 99% and 0.91, respectively. Furthermore, we examined the surgical outcomes of UPA and found that the group diagnosed as unilateral by the predictors showed improvement in clinical findings, while the group diagnosed as bilateral by the predictors showed no improvement.
Conclusion
Our predictive model based on machine learning can support to choose the performance of adrenal vein sampling or watchful observation.





Similar content being viewed by others
References
Milliez P, Girerd X, Plouin PF, Blacher J, Safar ME, Mourad JJ. Evidence for an increased rate of cardiovascular events in patients with primary aldosteronism. J Am Coll Cardiol. 2005;45(8):1243–8.
Stowasser M, Gordon RD, Gunasekera TG, Cowley DC, Ward G, Archibald C, et al. High rate of detection of primary aldosteronism, including surgically treatable forms, after “non-selective” screening of hypertensive patients. J Hypertens. 2003;21(11):2149–57.
Calhoun DA. Resistant or difficult-to-treat hypertension. J Clin Hypertens (Greenwich). 2006;8(3):181–6.
Douma S, Petidis K, Doumas M, Papaefthimiou P, Triantafyllou A, Kartali N, et al. Prevalence of primary hyperaldosteronism in resistant hypertension: a retrospective observational study. Lancet. 2008;371(9628):1921–6.
Mulatero P, Rabbia F, Milan A, Paglieri C, Morello F, Chiandussi L, et al. Drug effects on aldosterone/plasma renin activity ratio in primary aldosteronism. Hypertension. 2002;40(6):897–902.
Muiesan ML, Salvetti M, Rizzoni D, Paini A, Agabiti-Rosei C, Aggiusti C, et al. Resistant hypertension and target organ damage. Hypertens Res. 2013;36(6):485–91.
Abad-Cardiel M, Alvarez-Álvarez B, Luque-Fernandez L, Fernández C, Fernández-Cruz A, Martell-Claros N. Hypertension caused by primary hyperaldosteronism: increased heart damage and cardiovascular risk. Rev Esp Cardiol (Engl Ed). 2013;66(1):47–52.
Savard S, Amar L, Plouin PF, Steichen O. Cardiovascular complications associated with primary aldosteronism: a controlled cross-sectional study. Hypertension. 2013;62(2):331–6.
Tanabe A, Naruse M, Naruse K, Hase M, Yoshimoto T, Tanaka M, et al. Left ventricular hypertrophy is more prominent in patients with primary aldosteronism than in patients with other types of secondary hypertension. Hypertens Res. 1997;20(2):85–90.
Hundemer GL, Curhan GC, Yozamp N, Wang M, Vaidya A. Cardiometabolic outcomes and mortality in medically treated primary aldosteronism: a retrospective cohort study. Lancet Diabetes Endocrinol. 2018;6(1):51–9.
Krug AW, Ehrhart-Bornstein M. Aldosterone and metabolic syndrome: is increased aldosterone in metabolic syndrome patients an additional risk factor? Hypertension. 2008;51(5):1252–8.
Lethielleux G, Amar L, Raynaud A, Plouin PF, Steichen O. Influence of diagnostic criteria on the interpretation of adrenal vein sampling. Hypertension. 2015;65(4):849–54.
Vonend O, Ockenfels N, Gao X, Allolio B, Lang K, Mai K, et al. Adrenal venous sampling: evaluation of the German Conn’s registry. Hypertension. 2011;57(5):990–5.
Monticone S, Satoh F, Dietz AS, Goupil R, Lang K, Pizzolo F, et al. Clinical management and outcomes of adrenal hemorrhage following adrenal vein sampling in primary aldosteronism. Hypertension. 2016;67(1):146–52.
Nishikawa T, Omura M, Satoh F, Shibata H, Takahashi K, Tamura N, et al. Guidelines for the diagnosis and treatment of primary aldosteronism–the Japan Endocrine Society 2009. Endocr J. 2011;58(9):711–21.
Shimamoto K, Ando K, Fujita T, Hasebe N, Higaki J, Horiuchi M, et al. The Japanese Society of Hypertension Guidelines for the Management of Hypertension (JSH 2014). Hypertens Res. 2014;37(4):253–390.
Funder JW, Carey RM, Fardella C, Gomez-Sanchez CE, Mantero F, Stowasser M, et al. Case detection, diagnosis, and treatment of patients with primary aldosteronism: an endocrine society clinical practice guideline. J Clin Endocrinol Metab. 2008;93(9):3266–81.
Kempers MJ, Lenders JW, van Outheusden L, van der Wilt GJ, Schultze Kool LJ, Hermus AR, et al. Systematic review: diagnostic procedures to differentiate unilateral from bilateral adrenal abnormality in primary aldosteronism. Ann Intern Med. 2009;151(5):329–37.
Rossi GP, Barisa M, Allolio B, Auchus RJ, Amar L, Cohen D, et al. The Adrenal Vein Sampling International Study (AVIS) for identifying the major subtypes of primary aldosteronism. J Clin Endocrinol Metab. 2012;97(5):1606–14.
Stowasser M, Taylor PJ, Pimenta E, Ahmed AH, Gordon RD. Laboratory investigation of primary aldosteronism. Clin Biochem Rev. 2010;31(2):39–56.
Rossi GP, Auchus RJ, Brown M, Lenders JW, Naruse M, Plouin PF, et al. An expert consensus statement on use of adrenal vein sampling for the subtyping of primary aldosteronism. Hypertension. 2014;63(1):151–60.
Li XF, Huang YZ, Tang JY, Li RC, Wang XQ. Development of a random forest model for hypotension prediction after anesthesia induction for cardiac surgery. World J Clin Cases. 2021;9(29):8729–39.
Wang Z, Zhe S, Zimmerman J, Morrisey C, Tonna JE, Sharma V, et al. Development and validation of a machine learning method to predict intraoperative red blood cell transfusions in cardiothoracic surgery. Sci Rep. 2022;12(1):1355.
Tsai IJ, Shen WC, Lee CL, Wang HD, Lin CY. Machine learning in prediction of bladder cancer on clinical laboratory data. Diagnostics (Basel). 2022;12(1):203.
Garge NR, Bobashev G, Eggleston B. Random forest methodology for model-based recursive partitioning: the mobForest package for R. BMC Bioinformatics. 2013;14:125.
Su X, Xu Y, Tan Z, Wang X, Yang P, Su Y, et al. Prediction for cardiovascular diseases based on laboratory data: an analysis of random forest model. J Clin Lab Anal. 2020;34(9): e23421.
Zhang Y, Luo F, Fan P, Meng X, Yang K, Zhou X. Is primary aldosteronism a potential risk factor for aortic dissection? A case report and literature review. BMC Endocr Disord. 2020;20(1):115.
Byun JM, Chon S, Kim SJ. A case of primary aldosteronism presenting as non-ST elevation myocardial infarction. Korean J Intern Med. 2013;28(6):739–42.
Auchus RJ, Michaelis C, Wians FH, Dolmatch BL, Josephs SC, Trimmer CK, et al. Rapid cortisol assays improve the success rate of adrenal vein sampling for primary aldosteronism. Ann Surg. 2009;249(2):318–21.
Daunt N. Adrenal vein sampling: how to make it quick, easy, and successful. Radiographics. 2005;25(Suppl 1):S143–58.
Küpers EM, Amar L, Raynaud A, Plouin PF, Steichen O. A clinical prediction score to diagnose unilateral primary aldosteronism. J Clin Endocrinol Metab. 2012;97(10):3530–7.
Nanba K, Tsuiki M, Nakao K, Nanba A, Usui T, Tagami T, et al. A subtype prediction score for primary aldosteronism. J Hum Hypertens. 2014;28(12):716–20.
Kocjan T, Janez A, Stankovic M, Vidmar G, Jensterle M. A new clinical prediction criterion accurately determines a subset of patients with bilateral primary aldosteronism before adrenal venous sampling. Endocr Pract. 2016;22(5):587–94.
Kobayashi H, Haketa A, Ueno T, Ikeda Y, Hatanaka Y, Tanaka S, et al. Scoring system for the diagnosis of bilateral primary aldosteronism in the outpatient setting before adrenal venous sampling. Clin Endocrinol (Oxf). 2017;86(4):467–72.
Kobayashi H, Abe M, Soma M, Takeda Y, Kurihara I, Itoh H, et al. Development and validation of subtype prediction scores for the workup of primary aldosteronism. J Hypertens. 2018;36(11):2269–76.
Umakoshi H, Tsuiki M, Takeda Y, Kurihara I, Itoh H, Katabami T, et al. Significance of computed tomography and serum potassium in predicting subtype diagnosis of primary aldosteronism. J Clin Endocrinol Metab. 2018;103(3):900–8.
Burrello J, Burrello A, Pieroni J, Sconfienza E, Forestiero V, Rabbia P, et al. Development and validation of prediction models for subtype diagnosis of patients with primary aldosteronism. J Clin Endocrinol Metab. 2020;105(10):e3706–17.
Kaneko H, Umakoshi H, Ogata M, Wada N, Iwahashi N, Fukumoto T, et al. Machine learning based models for prediction of subtype diagnosis of primary aldosteronism using blood test. Sci Rep. 2021;11(1):9140.
Sechi LA, Colussi G, Di Fabio A, Catena C. Cardiovascular and renal damage in primary aldosteronism: outcomes after treatment. Am J Hypertens. 2010;23(12):1253–60.
Zarnegar R, Young WF, Lee J, Sweet MP, Kebebew E, Farley DR, et al. The aldosteronoma resolution score: predicting complete resolution of hypertension after adrenalectomy for aldosteronoma. Ann Surg. 2008;247(3):511–8.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
The authors did not receive support from any organization for the submitted work.
Conflict of interest
Authors have no conflicts of interest to declare that are relevant to the content of this article.
Ethics approval
This study was performed in accordance with the principles of the Declaration of Helsinki and was approved by the ethics committee of Tokyo Medical University Hospital (T2018-0017). The need for informed patient consent was waived owing to the study’s retrospective design. Of note, at the start of the study, we used an opt-out approach to notify patients and disclose information on the purpose and implementation of the research and to guarantee opportunities to opt-out as much as possible.
Data availability
Raw data were generated at Tokyo Medical University. Derived data supporting the findings of this study are available from the corresponding author on request.
Rights and permissions
About this article
Cite this article
Tamaru, S., Suwanai, H., Abe, H. et al. Machine learning approach to predict subtypes of primary aldosteronism is helpful to estimate indication of adrenal vein sampling. High Blood Press Cardiovasc Prev 29, 375–383 (2022). https://doi.org/10.1007/s40292-022-00523-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40292-022-00523-8