Abstract
Objective
A systematic review was carried out to summarize the available evidence to assess whether circulating nucleic acids in maternal plasma and serum (CNAPS) have the potential to serve as extra and independent markers for the prediction and/or progression monitoring of the most common and severe complications of pregnancy, including preeclampsia, intrauterine growth restriction, preterm delivery, morbidly adherent placenta, gestational diabetes, antiphospholipid syndrome, threatened abortion, intrahepatic cholestasis of pregnancy, and hyperemesis gravidarum.
Method
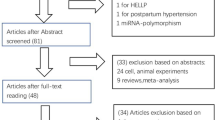
A comprehensive literature search of the MEDLINE (PubMed), EMBASE, and ISI Web of Knowledge databases was conducted to identify relevant studies that included amounts of CNAPS in the abovementioned pregnancy complications.
Results
Eighty-three studies met the eligibility criteria. The vast majority of studies were conducted on the quantity of total circulating cell free DNA (cfDNA) and cell free fetal DNA (cffDNA), and some were conducted on messenger RNA (mRNA) species. A few studies have instead evaluated the cell free DNA fetal fraction (cfDNAff), but only in a limited number of pregnancy complications. Despite the growing interest and the abundance of the papers available, little information is available for other new CNAPS, including microRNA (miRNA), long noncoding RNA (lncRNA), mitochondrial DNA (mtDNA), and circular RNA.
Conclusion
Due to the heterogeneity of the populations enrolled, the scarcity of the studies that adjusted the CNAPS values for possible confounding factors, and the difficulty in interpreting the published data, no conclusion regarding the statistical robustness and clinical relevance of the data can be made at present. If assayed at the third trimester, the CNAPS have, however, shown better performance, and could be used in populations already at risk of developing complications as suggested by the presence of other clinical features. Other CNAPS, including miRNA, are under investigation, especially for the screening of gestational diabetes mellitus, but no data about their clinical utility are available. Circulating DNA (cfDNA, cffDNA, and cfDNAff) and mRNA have not been properly evaluated yet, especially in patients asymptomatic early in pregnancy but who developed complications later, perhaps because of the high cost of these techniques and the availability of other predictors of pregnancy complications (biochemical, biophysical, and ultrasound markers). Therefore, from the analysis of the data, the positive predictive value is not available. As regards the new CNAPS, including miRNA, there are still no sufficient data to understand if they can be promising markers for pregnancy complications monitoring and screening, since CNAPS are statistically weak and expensive. It is reasonable to currently conclude that the use of the CNAPS in clinical practice is not recommended.

Similar content being viewed by others
References
Lo YMD, Corbetta N, Chamberlain PF, Rai V, Sargent IL, Redman CW, et al. Presence of fetal DNA in maternal plasma and serum. Lancet. 1997;350:485–7.
Lo YM, Lau TK, Zhang J, Leung TN, Chang AM, Hjelm NM, Elmes RS, Bianchi DW. Increased fetal DNA concentrations in the plasma of pregnant women carrying fetuses with trisomy 21. Clin Chem. 1999;45:1747–51.
Lo YM, Hjelm NM, Fidler C, Sargent IL, Murphy MF, Chamberlain PF, Poon PM, Redman CW, Wainscoat JS. Prenatal diagnosis of fetal RhD status by molecular analysis of maternal plasma. N Engl J Med. 1998;339:1734–8.
Farina A, LeShane ES, Lambert-Messerlian GM, Canick JA, Lee T, Neveux LM, Palomaki GE, Bianchi DW. Evaluation of cell-free fetal DNA as a second-trimester maternal serum marker of Down syndrome pregnancy. Clin Chem. 2003;49:239–42.
Lim JH, Kim MH, Han YJ, Lee DE, Park SY, Han JY, Kim MY, Ryu HM. Cell-free fetal DNA and cell-free total DNA levels in spontaneous abortion with fetal chromosomal aneuploidy. PLoS One. 2013;8:e56787.
Wataganara T, LeShane ES, Farina A, Messerlian GM, Lee T, Canick JA, Bianchi DW. Maternal serum cell-free fetal DNA levels are increased in cases of trisomy 13 but not trisomy 18. Hum Genet. 2003;112:204–8.
Contro E, Bernabini D, Farina A. Cell-free fetal DNA for the prediction of pre-eclampsia at the first and second trimesters: a systematic review and meta-analysis. Mol Diagn Ther. 2017;21:125–35.
Hahn S, Huppertz B, Holzgreve W. Fetal cells and cell free fetal nucleic acids in maternal blood: new tools to study abnormal placentation? Placenta. 2005;26:515–26.
Sekizawa A, Jimbo M, Saito H, Iwasaki M, Matsuoka R, Okai T, Farina A. Cell-free fetal DNA in the plasma of pregnant women with severe fetal growth restriction. Am J Obstet Gynecol. 2003;188:480–4.
Leung TN, Zhang J, Lau TK, Hjelm NM, Lo YM. Maternal plasma fetal DNA as a marker for preterm labour. Lancet. 1998;352:1904–5.
Farina A, LeShane ES, Romero R, Gomez R, Chaiworapongsa T, Rizzo N, Bianchi DW. High levels of fetal cell-free DNA in maternal serum: a risk factor for spontaneous preterm delivery. Am J Obstet Gynecol. 2005;193:421–5.
Illanes S, Gomez R, Fornes R, Figueroa-Diesel H, Schepeler M, Searovic P, Serra R, Perez A, Nien JK. Free fetal DNA levels in patients at risk of preterm labour. Prenat Diagn. 2011;31:1082–5.
Jakobsen TR, Clausen FB, Rode L, Dziegiel MH, Tabor A. High levels of fetal DNA are associated with increased risk of spontaneous preterm delivery. Prenat Diagn. 2012;32:840–5.
Sugito Y, Sekizawa A, Farina A, Yukimoto Y, Saito H, Iwasaki M, Rizzo N, Okai T. Relationship between severity of hyperemesis gravidarum and fetal DNA concentration in maternal plasma. Clin Chem. 2003;49:1667–9.
Sekizawa A, Jimbo M, Saito H, Iwasaki M, Sugito Y, Yukimoto Y, Otsuka J, Okai T. Increased cell-free fetal DNA in plasma of two women with invasive placenta. Clin Chem. 2002;48:353–4.
Cotter AM, Martin CM, O’Leary JJ, Daly SF. Increased fetal RhD gene in the maternal circulation in early pregnancy is associated with an increased risk of pre-eclampsia. BJOG. 2005;112(5):584–7.
Ng EK, Tsui NB, Lau TK, Leung TN, Chiu RW, Panesar NS, Lit LC, Chan KW, Lo YM. mRNA of placental origin is readily detectable in maternal plasma. Proc Natl Acad Sci USA. 2003;100:4748–53.
Ng EK, Leung TN, Tsui NB, Lau TK, Panesar NS, Chiu RW, Lo YM. The concentration of circulating corticotropin-releasing hormone mRNA in maternal plasma is increased in preeclampsia. Clin Chem. 2003;49:727–31.
Tsui NB, Chim SS, Chiu RW, Lau TK, Ng EK, Leung TN, Tong YK, Chan KC, Lo YM. Systematic micro-array based identification of placental mRNA in maternal plasma: towards non-invasive prenatal gene expression profiling. J Med Genet. 2004;41:461–7.
Farina A, Zucchini C, Sekizawa A, Purwosunu Y, de Sanctis P, Santarsiero G, Rizzo N, Morano D, Okai T. Performance of messenger RNAs circulating in maternal blood in the prediction of preeclampsia at 10–14 weeks. Am J Obstet Gynecol. 2010;203(575):e1–7.
Zanello M, Sekizawa A, Purwosunu Y, Curti A, Farina A. Circulating mRNA for the PLAC1 gene as a second trimester marker (14–18 weeks’ gestation) in the screening for late preeclampsia. Fetal Diagn Ther. 2014;36:196–201.
Zanello M, DeSanctis P, Pula G, Zucchini C, Pittalis MC, Rizzo N, Farina A. Circulating mRNA for epidermal growth factor-like domain 7 (EGFL7) in maternal blood and early intrauterine growth restriction. A preliminary analysis. Prenat Diagn. 2013;33:168–72.
Quezada MS, Francisco C, Dumitrascu-Biris D, Nicolaides KH, Poon LC. Fetal fraction of cell-free DNA in maternal plasma in the prediction of spontaneous preterm delivery. Ultrasound Obstet Gynecol. 2015;45:101–5.
Rolnik DL, da Silva Costa F, Lee TJ, Schmid M, McLennan AC. Association between fetal fraction on cell-free DNA testing and first-trimester markers for pre-eclampsia. Ultrasound Obstet Gynecol. 2018;52:722–7.
Morano D, Rossi S, Lapucci C, Pittalis MC, Farina A. Cell-free DNA (cfDNA) fetal fraction in early- and late-onset fetal growth restriction. Mol Diagn Ther. 2018;22:613–9.
Cai M, Kolluru GK, Ahmed A. Small molecule, big prospects: microRNA in pregnancy and its complications. J Pregnancy. 2017;2017:6972732.
Jóźwik M, Lipka A. Recent progress in human placental transcriptomics. Dev Period Med. 2019;23:104–8.
Myatt L, Muralimanoharan S, Maloyan A. Effect of preeclampsia on placental function: influence of sexual dimorphism, microRNA’s and mitochondria. Adv Exp Med Biol. 2014;814:133–46.
Yan L, Feng J, Cheng F, Cui X, Gao L, Chen Y, Wang F, Zhong T, Li Y, Liu L. Circular RNA expression profiles in placental villi from women with gestational diabetes mellitus. Biochem Biophys Res Commun. 2018;498:743–50.
Moher D, Shamseer L, Clarke M, Ghersi D, Liberati A, Petticrew M, et al. Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015 statement. Syst Rev. 2015;4:1.
Conn VS, Valentine JC, Cooper HM, Rantz MJ. Grey literature in meta-analyses. Nurs Res. 2003;52:256–61.
Lo CK-L, Mertz D, Loeb M. Newcastle-Ottawa Scale: comparing reviewers’ to authors’ assessments. BMC Med Res Methodol. 2014;14:45.
Modesti PA, Reboldi G, Cappuccio FP, Agyemang C, Remuzzi G, Rapi S, Perruolo E, Parati G; ESH Working Group on CV Risk in Low Resource Settings. Panethnic differences in blood pressure in Europe: a systematic review and meta-analysis. PLoS One. 2016;11(1):e0147601.
Cohen IT, Patel K. Peer review interrater reliability of scientific abstracts: a study of an anesthesia subspecialty society. J Educ Perioper Med JEPM. 2005;7:E035.
Abalos E, Cuesta C, Grosso AL, Chou D, Say L. Global and regional estimates of preeclampsia and eclampsia: a systematic review. Eur J Obstet Gynecol Reprod Biol. 2013;170:1–7.
Steegers EAP, von Dadelszen P, Duvekot JJ, Pijnenborg R. Pre-eclampsia. Lancet Lond Engl. 2010;376:631–44.
Jebbink J, Wolters A, Fernando F, Afink G, van der Post J, Ris-Stalpers C. Molecular genetics of preeclampsia and HELLP syndrome—a review. Biochim Biophys Acta. 2012:1960-9.
ACOG Committee Opinion No. 743: Low-dose aspirin use during pregnancy. Obstet Gynecol. 2018;132(1):e44–52.
Rolnik DL, Wright D, Poon LC, O’Gorman N, Syngelaki A, de Paco Matallana C, Akolekar R, Cicero S, Janga D, Singh M, Molina FS, Persico N, Jani JC, Plasencia W, Papaioannou G, Tenenbaum-Gavish K, Meiri H, Gizurarson S, Maclagan K, Nicolaides KH. Aspirin versus placebo in pregnancies at high risk for preterm preeclampsia. N Engl J Med. 2017;377(7):613–22. https://doi.org/10.1056/NEJMoa1704559 (Epub 2017 Jun 28).
Engel K, Tomasz P, Bilar M, Agnieszka O, Ewa B, Elzbieta R-W. Assessment of the female fetal DNA concentration in the plasma of the pregnant women as preeclampsia indicator–preliminary report. Eur J Obstet Gynecol Reprod Biol. 2009;146:165–8.
Muñoz-Hernández R, Medrano-Campillo P, Miranda ML, Macher HC, Praena-Fernández JM, Vallejo-Vaz AJ, Dominguez-Simeon MJ, Moreno-Luna R, Stiefel P. Total and fetal circulating cell-free DNA, angiogenic, and antiangiogenic factors in preeclampsia and HELLP syndrome. Am J Hypertens. 2017;30:673–82.
Farina A, Sekizawa A, Rizzo N, Concu M, Banzola I, Carinci P, Simonazzi G, Okai T. Cell-free fetal DNA (SRY locus) concentration in maternal plasma is directly correlated to the time elapsed from the onset of preeclampsia to the collection of blood. Prenat Diagn. 2004;24:293–7.
Zhong XY, Laivuori H, Livingston JC, Ylikorkala O, Sibai BM, Holzgreve W, Hahn S. Elevation of both maternal and fetal extracellular circulating deoxyribonucleic acid concentrations in the plasma of pregnant women with preeclampsia. Am J Obstet Gynecol. 2001;184:414–9.
Thurik FF, Lamain-de Ruiter M, Javadi A, Kwee A, Woortmeijer H, Page-Christiaens GC, Franx A, van der Schoot CE, Koster MP. Absolute first trimester cell-free DNA levels and their associations with adverse pregnancy outcomes. Prenat Diagn. 2016;36:1104–11.
Zamanpoor M, Rosli R, Yazid MN, Husain Z, Nordin N, Thilakavathy K. Quantitative analysis of fetal DNA in maternal plasma in gestational diabetes mellitus, iron deficiency anemia and gestational hypertension pregnancies. J Matern Fetal Neonatal Med. 2013;26:960–6.
Swinkels DW, de Kok JB, Hendriks JC, Wiegerinck E, Zusterzeel PL, Steegers EA. Hemolysis, elevated liver enzymes, and low platelet count (HELLP) syndrome as a complication of preeclampsia in pregnant women increases the amount of cell-free fetal and maternal DNA in maternal plasma and serum. Clin Chem. 2002;48:650–3.
Engel K, Płonka T, Bilar M, Orzinska A, Brojer E, Ronin-Walknowska E. The correlation between clinical characteristics of preeclampsia and the concentration of fetal DNA in maternal circulation. Eur J Obstet Gynecol Reprod Biol. 2008;139(2):256–7.
Smid M, Vassallo A, Lagona F, Valsecchi L, Maniscalco L, Danti L, et al. Quantitative analysis of fetal DNA in maternal plasma in pathological conditions associated with placental abnormalities. Ann N Y Acad Sci. 2001;945:132–7.
Sur Chowdhury C, Hahn S, Hasler P, Hoesli I, Lapaire O, Giaglis S. Elevated levels of total cell-free DNA in maternal serum samples arise from the generation of neutrophil extracellular traps. Fetal Diagn Ther. 2016;40:263–7.
Rafaeli-Yehudai T, Imterat M, Douvdevani A, Tirosh D, Benshalom-Tirosh N, Mastrolia SA, Beer-Weisel R, Klaitman V, Riff R, Greenbaum S, Alioshin A, Rodavsky Hanegbi G, Loverro G, Catalano MR, Erez O. Maternal total cell-free DNA in preeclampsia and fetal growth restriction: evidence of differences in maternal response to abnormal implantation. PLoS One. 2018;12(13):e0200360.
Sekizawa A, Farina A, Koide K, Iwasaki M, Honma S, Ichizuka K, Saito H, Okai T. Beta-globin DNA in maternal plasma as a molecular marker of pre-eclampsia. Prenat Diagn. 2004;24:697–700.
AbdelHalim RM, Ramadan DI, Zeyada R, Nasr AS, Mandour IA. Circulating maternal total cell-free DNA, cell-free fetal DNA and soluble endoglin levels in preeclampsia: predictors of adverse fetal outcome? A cohort study. Mol Diagn Ther. 2016;20:135–49.
Lázár L, Nagy B, Molvarec A, Rigó J Jr. Quantity of total cell free and cell free fetal DNA in pregnancies with no complications and with preeclampsia. Orv Hetil. 2010;151:784–7.
Farina A, Sekizawa A, Iwasaki M, Matsuoka R, Ichizuka K, Okai T. Total cell-free DNA (beta-globin gene) distribution in maternal plasma at the second trimester: a new prospective for preeclampsia screening. Prenat Diagn. 2004;24:722–6.
Zhong XY, Holzgreve W, Hahn S. Circulatory fetal and maternal DNA in pregnancies at risk and those affected by preeclampsia. Ann N Y Acad Sci. 2001;945:138–40.
Poon LC, Musci T, Song K, Syngelaki A, Nicolaides KH. Maternal plasma cell-free fetal and maternal DNA at 11-13 weeks’ gestation: relation to fetal and maternal characteristics and pregnancy outcomes. Fetal Diagn Ther. 2013;33:215–23.
Silver RM, Myatt L, Hauth JC, Leveno KJ, Peaceman AM, Ramin SM, Samuels P, Saade G, Sorokin Y, Clifton RG, Reddy UM. Cell-free total and fetal DNA in first trimester maternal serum and subsequent development of preeclampsia. Am J Perinatol. 2017;34:191–8.
Suzumori N, Sekizawa A, Ebara T, Samura O, Sasaki A, Akaishi R, Wada S, Hamanoue H, Hirahara F, Izumi H, Sawai H, Nakamura H, Yamada T, Miura K, Masuzaki H, Yamashita T, Okai T, Kamei Y, Namba A, Murotsuki J, Tanemoto T, Fukushima A, Haino K, Tairaku S, Matsubara K, Maeda K, Kaji T, Ogawa M, Osada H, Nishizawa H, Okamoto Y, Kanagawa T, Kakigano A, Kitagawa M, Ogawa M, Izumi S, Katagiri Y, Takeshita N, Kasai Y, Naruse K, Neki R, Masuyama H, Hyodo M, Kawano Y, Ohba T, Ichizuka K, Nagamatsu T, Watanabe A, Shirato N, Yotsumoto J, Nishiyama M, Hirose T, Sago H. Fetal cell-free DNA fraction in maternal plasma for the prediction of hypertensive disorders of pregnancy. Eur J Obstet Gynecol Reprod Biol. 2018;224:165–9.
Gerson KD, Truong S, Haviland MJ, O’Brien BM, Hacker MR, Spiel MH. Low fetal fraction of cell-free DNA predicts placental dysfunction and hypertensive disease in pregnancy. Pregnancy Hypertens. 2019;16:148–53.
Yuan X, Zhou L, Zhang B, Wang H, Jiang J, Yu B. Early second-trimester plasma cell free DNA levels with subsequent risk of pregnancy complications. Clin Biochem. 2019;71:46–51.
Bender WR, Koelper NC, Sammel MD, Dugoff L. Association of fetal fraction of cell-free DNA and hypertensive disorders of pregnancy. Am J Perinatol. 2019;36:311–6.
Wataganara T, Metzenbauer M, Peter I, Johnson KL, Bianchi DW. Placental volume, as measured by 3-dimensional sonography and levels of maternal plasma cell-free fetal DNA. Am J Obstet Gynecol. 2005;193:496–500.
Chan N, Smet ME, Sandow R, da Silva Costa F, McLennan A. Implications of failure to achieve a result from prenatal maternal serum cell-free DNA testing: a historical cohort study. BJOG. 2018;125:848–55.
Farina A, Chan CW, Chiu RW, Tsui NB, Carinci P, Concu M, Banzola I, Rizzo N, Lo YM. Circulating corticotropin-releasing hormone mRNA in maternal plasma: relationship with gestational age and severity of preeclampsia. Clin Chem. 2004;50:1851–4.
Galbiati S, Causarano V, Pinzani P, Francesca S, Orlando C, Smid M, Pasi F, Castiglioni MT, Cavoretto P, Rovere-Querini P, Pedroni S, Calza S, Ferrari M, Cremonesi L. Evaluation of a panel of circulating DNA, RNA and protein potential markers for pathologies of pregnancy. Clin Chem Lab Med. 2010;48:791–4.
Farina A, Sekizawa A, De Sanctis P, Purwosunu Y, Okai T, Cha DH, Kang JH, Vicenzi C, Tempesta A, Wibowo N, Valvassori L, Rizzo N. Gene expression in chorionic villous samples at 11 weeks’ gestation from women destined to develop preeclampsia. Prenat Diagn. 2008;28:956–61.
Tsui NB, Lo YM. A microarray approach for systematic identification of placental-derived RNA markers in maternal plasma. Methods Mol Biol. 2008;444:275–89.
Paiva P, Whitehead C, Saglam B, Palmer K, Tong S. Measurement of mRNA transcripts of very high placental expression in maternal blood as biomarkers of preeclampsia. J Clin Endocrinol Metab. 2011;96:E1807–15.
Farina A. The role of RNAs and microRNAs in non-invasive prenatal diagnosis. J Clin Med. 2014;6(3):440–52.
Sekizawa A, Purwosunu Y, Farina A, Shimizu H, Nakamura M, Wibowo N, Rizzo N, Okai T. Prediction of pre-eclampsia by an analysis of placenta-derived cellular mRNA in the blood of pregnant women at 15–20 weeks of gestation. BJOG. 2010;117(5):557–64.
Wright D, Wright A, Nicolaides KH. The competing risk approach for prediction of preeclampsia. Am J Obstet Gynecol. 2019 [Epub ahead of print].
Hu Y, Li P, Hao S, Liu L, Zhao J, Hou Y. Differential expression of microRNAs in the placentae of Chinese patients with severe pre-eclampsia. Clin Chem Lab Med. 2009;47:923–9.
Pineles BL, Romero R, Montenegro D, Tarca AL, Han YM, Kim YM, Draghici S, Espinoza J, Kusanovic JP, Mittal P, Hassan SS, Kim CJ. Distinct subsets of microRNAs are expressed differentially in the human placentas of patients with preeclampsia. Am J Obstet Gynecol. 2007;196(261):e1–6.
Enquobahrie DA, Abetew DF, Sorensen TK, Willoughby D, Chidambaram K, Williams MA. Placental microRNA expression in pregnancies complicated by preeclampsia. Am J Obstet Gynecol. 2011;204(178):e12–21.
Mayor-Lynn K, Toloubeydokhti T, Cruz AC, Chegini N. Expression profile of microRNAs and mRNAs in human placentas from pregnancies complicated by preeclampsia and preterm labor. Reprod Sci. 2011;18:46–56.
Yang Q, Lu J, Wang S, Li H, Ge Q, Lu Z. Application of next-generation sequencing technology to profile the circulating microRNAs in the serum of preeclampsia versus normal pregnant women. Clin Chim Acta. 2011;412:2167–73.
Wu L, Zhou H, Lin H, Qi J, Zhu C, Gao Z, Wang H. Circulating microRNAs are elevated in plasma from severe preeclamptic pregnancies. Reproduction. 2012;143:389–97.
Zhao Z, Moley KH, Gronowski AM. Diagnostic potential for miRNAs as biomarkers for pregnancy-specific diseases. Clin Biochem. 2013;46:953–60.
Luque A, Farwati A, Crovetto F, Crispi F, Figueras F, Gratacós E. Aran Usefulness of circulating microRNAs for the prediction of early preeclampsia at first-trimester of pregnancy. JM Sci Rep. 2014;4:4882.
Gunel T, Zeybek YG, Akçakaya P, Kalelioğlu I, Benian A, Ermis H, Aydınlı K. Serum microRNA expression in pregnancies with preeclampsia. Genet Mol Res. 2011;10(4):4034–40.
Li H, Ge Q, Guo L, Lu Z. Maternal plasma miRNAs expression in preeclamptic pregnancies. Biomed Res Int. 2013;970265.
Hromadnikova I, Dvorakova L, Kotlabova K, Krofta L. The prediction of gestational hypertension, preeclampsia and fetal growth restriction via the first trimester screening of plasma exosomal C19MC microRNAs. Int J Mol Sci. 2019;20:E2972.
Smid M, Galbiati S, Lojacono A, Valsecchi L, Platto C, Cavoretto P, Calza S, Ferrari A, Ferrari M, Cremonesi L. Correlation of fetal DNA levels in maternal plasma with Doppler status in pathological pregnancies. Prenat Diagn. 2006;26:785–90.
Alberry MS, Illanis S, Maddocks DG, Fattah SA, Zimmermann BG, Avent ND, et al. Maternal levels of free fetal DNA are elevated in pregnancies with growth restriction due to placental dysfunction: a preliminary study. South Afr J Obstet Gynaecol. 2007;13:60–3.
Alberry MS, Maddocks DG, Hadi MA, Metawi H, Hunt LP, Abdel-Fattah SA, et al. Quantification of cell free fetal DNA in maternal plasma in normal pregnancies and in pregnancies with placental dysfunction. Am J Obstet Gynecol. 2009;200(98):e1–6.
Al Nakib M, Desbrière R, Bonello N, Bretelle F, Boubli L, Gabert J, et al. Total and fetal cell-free DNA analysis in maternal blood as markers of placental insufficiency in intrauterine growth restriction. Fetal Diagn Ther. 2009;26:24–8.
Hromadnikova I, Zejskova L, Kotlabova K, Cuskova T, Doucha J, Dlouha K, et al. Quantification of extracellular DNA using hypermethylated RASSF1A, SRY, and GLO sequences–evaluation of diagnostic possibilities for predicting placental insufficiency. DNA Cell Biol. 2010;29:295–301.
Crowley A, Martin C, Fitzpatrick P, Sheils O, O’Herlihy C, O’Leary JJ, et al. Free fetal DNA is not increased before 20 weeks in intrauterine growth restriction or pre-eclampsia. Prenat Diagn. 2007;27:174–9.
Ershova E, Sergeeva V, Klimenko M, Avetisova K, Klimenko P, Kostyuk E, et al. Circulating cell-free DNA concentration and DNase I activity of peripheral blood plasma change in case of pregnancy with intrauterine growth restriction compared to normal pregnancy. Biomed Rep. 2017;7:319–24.
Caramelli E, Rizzo N, Concu M, Simonazzi G, Carinci P, Bondavalli C, et al. Cell-free fetal DNA concentration in plasma of patients with abnormal uterine artery Doppler waveform and intrauterine growth restriction–a pilot study. Prenat Diagn. 2003;23:367–71.
Gordijn SJ, Beune IM, Thilaganathan B, Papageorghiou A, Baschat AA, Baker PN, Silver RM, Wynia K, Ganzevoort W. Consensus definition of fetal growth restriction: a Delphi procedure. Ultrasound Obstet Gynecol. 2016;48:333–9.
Shook LL, Clapp MA, Roberts PS, Bernstein SN, Goldfarb IT. High Fetal fraction on first trimester cell-free DNA aneuploidy screening and adverse pregnancy outcomes. Am J Perinatol. 2020;37:8–13.
Whitehead CL, Walker SP, Ye L, Mendis S, Kaitu’u-Lino TJ, Lappas M, Tong S. Placental specific mRNA in the maternal circulation are globally dysregulated in pregnancies complicated by fetal growth restriction. J Clin Endocrinol Metab. 2013;98:E429–36.
Whitehead CL, McNamara H, Walker SP, Alexiadis M, Fuller PJ, Vickers DK, Hannan NJ, Hastie R, Tuohey L, Kaitu’u-Lino TJ, Tong S. Identifying late-onset fetal growth restriction by measuring circulating placental RNA in the maternal blood at 28 weeks’ gestation. Am J Obstet Gynecol. 2016;214:521.e1–8.
Ayala Ramírez P, García Robles R, Rojas JD, Bermúdez M, Bernal J. Identification of messenger RNA of fetoplacental source in maternal plasma of women with normal pregnancies and pregnancies with intrauterine growth restriction. Colomb Medica Cali Colomb. 2012;43:184–8.
Luo SS, Ishibashi O, Ishikawa G, Ishakawa T, Katayama A, Mishima MR, et al. Human villous trophoblasts express and secrete placenta-specific MicroRNAs into maternal circulation via Exosomes1. Biol Reprod. 2009;81:717–29.
Awamleh Z, Gloor GB, Han VKM. Placental microRNAs in pregnancies with early onset intrauterine growth restriction and preeclampsia: potential impact on gene expression and pathophysiology. BMC Med Genomics. 2019;12:91.
Mouillet JF, Chu T, Hubel CA, Nelson DM, Parks WT, Sadovsky Y. The levels of hypoxia-regulated microRNAs in plasma of pregnant women with fetal growth restriction. Placenta. 2010;31:781–4.
Hromadnikova I, Kotlabova K, Ondrackova M, Kestlerova A, Novotna V, Hympanova L, Doucha J, Krofta L. Circulating C19MC microRNAs in preeclampsia, gestational hypertension, and fetal growth restriction. Mediators Inflamm. 2013;2013:186041.
Hromadnikova I, Kotlabova K, Ivankova K, Krofta L. First trimester screening of circulating C19MC microRNAs and the evaluation of their potential to predict the onset of preeclampsia and IUGR. PLoS One. 2017;12:e0171756.
Goldenberg RL, Culhane JF, Iams JD, Romero R. Epidemiology and causes of preterm birth. Lancet. 2008;371:75–84.
Fűri I, Kalmár A, Wichmann B, Spisák S, Schöller A, Barták B, Tulassay Z, Molnár B. Cell free DNA of tumor origin induces a ‘metastatic’ expression profile in HT-29 cancer cell line. PLoS One. 2015;10:e0131699.
Krieg AM. Therapeutic potential of toll-like receptor 9 activation. Nat Rev Drug Discov. 2006;5:471–84.
Barber GN. STING: infection, inflammation and cancer. Nat Rev Immunol. 2015;15:760–70.
van Boeckel SR, Davidson DJ, Norman JE, Stock SJ. Cell-free fetal DNA and spontaneous preterm birth. Reproduction. 2018;155:R137–45.
Darghahi R, Mobaraki-Asl N, Ghavami Z, Pourfarzi F, Hosseini-Asl S, Jalilvand F. Effect of cell-free fetal DNA on spontaneous preterm labor. J Adv Pharm Technol Res. 2019;10:117–20.
Stein W, Müller S, Gutensohn K, Emons G, Legler T. Cell-free fetal DNA and adverse outcome in low risk pregnancies. Eur J Obstet Gynecol Reprod Biol. 2013;166:10–3.
Guo FF, Yang JX, Huang YL, Qi YM, Hou YP, Peng HS, Wang DM, Wang YX, Luo XH, Li Y, Yin AH. Association between fetal fraction at the second trimester and subsequent spontaneous preterm birth. Prenat Diagn. 2019;39:1191–7.
Dugoff L, Barberio A, Whittaker PG, Schwartz N, Sehdev H, Bastek JA. Cell-free DNA fetal fraction and preterm birth. Am J Obstet Gynecol. 2016;215(231):e1–7.
Krishna I, Badell M, Loucks TL, Lindsay M, Samuel A. Adverse perinatal outcomes are more frequent in pregnancies with a low fetal fraction result on noninvasive prenatal testing. Prenat Diagn. 2016;36:210–5.
Ngo TTM, Moufarrej MN, Rasmussen MH, Camunas-Soler J, Pan W, Okamoto J, Neff NF, Liu K, Wong RJ, Downes K, Tibshirani R, Shaw GM, Skotte L, Stevenson DK, Biggio JR, Elovitz MA, Melbye M, Quake SR. Noninvasive blood tests for fetal development predict gestational age and preterm delivery. Science. 2018;360:1133–6.
Menon R, Debnath C, Lai A, Guanzon D, Bhatnagar S, Kshetrapal PK, Sheller-Miller S, Salomon C, Garbhini Study Team. Circulating exosomal miRNA profile during term and preterm birth pregnancies: a longitudinal study. Endocrinology. 2019;160:249–75.
Wommack JC, Trzeciakowski JP, Miranda RC, Stowe RP, Ruiz RJ. Micro RNA clusters in maternal plasma are associated with preterm birth and infant outcomes. PLoS One. 2018;13:e0199029.
Cook J, Bennett PR, Kim SH, Teoh TG, Sykes L, Kindinger LM, Garrett A, Binkhamis R, MacIntyre DA, Terzidou V. First trimester circulating microRNA biomarkers predictive of subsequent preterm delivery and cervical shortening. Sci Rep. 2019;9:5861.
Elovitz MA, Anton L, Bastek J, Brown AG. Can microRNA profiling in maternal blood identify women at risk for preterm birth? Am J Obstet Gynecol. 2015;212(782):e1–5.
Bhide A, Sebire N, Abuhamad A, Acharya G, Silver R. Morbidly adherent placenta: the need for standardization. Ultrasound Obstet Gynecol. 2017;49:559–63.
Wertaschnigg D, Lucovnik M, Klieser E, Huber-Kata J, Moertl MG. Increased cell-free fetal DNA fraction in the first trimester: a sign of abnormally invasive placenta? Ultraschall Med. 2018 [Epub ahead of print].
Samuel A, Bonanno C, Oliphant A, Batey A, Wright JD. Fraction of cell-free fetal DNA in the maternal serum as a predictor of abnormal placental invasion-a pilot study. Prenat Diagn. 2013;33:1050–3.
El Behery MM, Rasha LE, El Alfy Y. Cell-free placental mRNA in maternal plasma to predict placental invasion in patients with placenta accreta. Int J Gynaecol Obstet. 2010;109:30–3.
Masuzaki H, Miura K, Yoshiura K, Yamasaki K, Miura S, Yoshimura S, Nakayama D, Mapendano CK, Niikawa N, Ishimaru T. Placental mRNA in maternal plasma and its clinical application to the evaluation of placental status in a pregnant woman with placenta previa-percreta. Clin Chem. 2005;51:923–5.
Miura K, Miura S, Yamasaki K, Yoshida A, Yoshiura K, Nakayama D, Niikawa N, Masuzaki H. Increased level of cell-free placental mRNA in a subgroup of placenta previa that needs hysterectomy. Prenat Diagn. 2008;28:805–9.
Li J, Zhang N, Zhang Y, Hu X, Gao G, Ye Y, Peng W, Zhou J. Human placental lactogen mRNA in maternal plasma play a role in prenatal diagnosis of abnormally invasive placenta: yes or no? Gynecol Endocrinol. 2019;35:631–4.
Zhou J, Li J, Yan P, Ye YH, Peng W, Wang S, Wang XT. Maternal plasma levels of cell-free β-HCG mRNA as a prenatal diagnostic indicator of placenta accrete. Placenta. 2014;35:691–5.
Naghshineh E, Khorvash E, Kamali S. A comparison of cell-free placental messenger ribonucleic acid and color Doppler ultrasound for the prediction of placental invasion in patients with placenta accreta. Adv Biomed Res. 2015;4:31.
Simonazzi G, Farina A, Curti A, Pilu G, Santini D, Zucchini C, Sekizawa A, Rizzo N. Higher circulating mRNA levels of placental specific genes in a patient with placenta accreta. Prenat Diagn. 2011;31:827–9.
Long Y, Chen Y, Fu XQ, Yang F, Chen ZW, Mo GL, Lao DY, Li MJ. Research on the expression of MRNA-518b in the pathogenesis of placenta accreta. Eur Rev Med Pharmacol Sci. 2019;23:23–8.
Jayawardena L, McNamara E. Diagnosis and management of pregnancies complicated by haemolysis, elevated liver enzymes and low platelets syndrome in the tertiary setting. Intern Med J. 2019;50(3):342–9.
Guarino E, Delli Poggi C, Grieco GE, Cenci V, Ceccarelli E, Crisci I, Sebastiani G, Dotta F. Circulating microRNAs as biomarkers of gestational diabetes mellitus: updates and perspectives. Int J Endocrinol. 2018;2018(12):6380463.
Dias S, Pheiffer C, Abrahams Y, Rheeder P, Adam S. Molecular biomarkers for gestational diabetes mellitus. Int J Mol Sci. 2018;19(10):2926.
Zhao C, Dong J, Jiang T, Shi Z, Yu B, Zhu Y, Chen D, Xu J, Huo R, Dai J, Xia Y, Pan S, Hu Z, Sha J. Early second-trimester serum miRNA profiling predicts gestational diabetes mellitus. PLoS One. 2011;6:e23925.
Wander PL, Boyko EJ, Hevner K, Parikh VJ, Tadesse MG, Sorensen TK, Williams MA, Enquobahrie DA. Circulating early- and mid-pregnancy microRNAs and risk of gestational diabetes. Diabetes Res Clin Pract. 2017;132:1–9.
Pheiffer C, Dias S, Rheeder P, Adam S. Decreased expression of circulating miR-20a-5p in South African women with gestational diabetes mellitus. Mol Diagn Ther. 2018;22:345–52.
Yoffe L, Polsky A, Gilam A, Raff C, Mecacci F, Ognibene A, Crispi F, Gratacós E, Kanety H, Mazaki-Tovi S, Shomron N, Hod M. Early diagnosis of gestational diabetes mellitus using circulating microRNAs. Eur J Endocrinol. 2019;181:565–77.
Lamadrid-Romero M, Solís KH, Cruz-Reséndiz MS, Pérez JE, Díaz NF, Flores-Herrera H, García-López G, Perichart O, Reyes-Muñoz E, Arenas-Huertero F, Eguía-Aguilar P, Molina-Hernández A. Central nervous system development-related microRNAs levels increase in the serum of gestational diabetic women during the first trimester of pregnancy. Neurosci Res. 2018;130:8–22.
Ibarra A, Vega-Guedes B, Brito-Casillas Y, Wägner AM. Diabetes in pregnancy and microRNAs: promises and limitations in their clinical application. Noncoding RNA. 2018;4(4):32.
Hristoskova S, Holzgreve W, Hahn S. Anti-phospholipid and anti-DNA antibodies are not associated with the elevated release of circulatory fetal DNA in pregnancies affected by preeclampsia. Hypertens Pregnancy. 2004;23:257–68.
Korabecna M, Ulcova-Gallova Z, Horinek A, Pazourková E, Calda P. Quantification of circulating fetal DNA as a tool for potential monitoring of pregnant patients with antiphospholipid antibodies. Autoimmunity. 2014;47:473–7.
Farina A, Rizzo N, Concu M, Banzola I, Sekizawa A, Grotti S, Carinci P. Lower maternal PLAC1 mRNA in pregnancies complicated with vaginal bleeding (threatened abortion <20 weeks) and a surviving fetus. Clin Chem. 2005;51:224–7.
Yi P, Yin N, Zheng Y, Jiang H, Yu X, Yan Y, Liu Q, Xiao F, Li L. Elevated plasma levels of hypermethylated RASSF1A gene sequences in pregnant women with intrahepatic cholestasis. Cell Biochem Biophys. 2013;67:977–81.
Sekizawa A, Sugito Y, Iwasaki M, Watanabe A, Jimbo M, Hoshi S, et al. Cell-free fetal DNA is increased in plasma of women with hyperemesis gravidarum. Clin Chem. 2001;47:2164–5.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors, Ilma Floriana Carbone, Alessandro Conforti, Silvia Picarelli, Danila Morano, Carlo Alviggi, and Antonio Farina, do not have any conflict of interest.
Funding
No funding was used in the preparation of this review.
Rights and permissions
About this article
Cite this article
Carbone, I.F., Conforti, A., Picarelli, S. et al. Circulating Nucleic Acids in Maternal Plasma and Serum in Pregnancy Complications: Are They Really Useful in Clinical Practice? A Systematic Review. Mol Diagn Ther 24, 409–431 (2020). https://doi.org/10.1007/s40291-020-00468-5
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40291-020-00468-5