Abstract
Background
European Pharmacovigilance regulatory guidance recommends the evaluation of additional risk minimisation measures (aRMMs) with process indicators and outcomes. Evaluation of both measures within the same evaluation helps to establish the relationship between the implementation of aRMMs (across process indicators) and the impact on drug safety-related outcomes. The term risk minimisation evaluation (RMEv) was used to describe a study or group of studies that assesses the effectiveness of aRMMs for one specific product.
Objectives
The objective of this systematic review was to describe the characteristics and results of RMEv that include both process indicators and outcomes as well as those of studies that conform the RMEv in Europe.
Methods
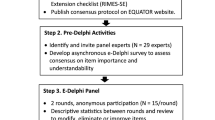
We conducted a systematic search in the European Union Register of Post-Authorization Studies, PubMed and grey literature (Google and abstracts of the International Conference on Pharmacoepidemiology and Therapeutic Risk Management) to identify studies that assessed the effectiveness of aRMMs including at least one European country, from 1 January, 2011 to 12 October, 2019. Identified studies linked to one product were considered part of the product RMEv. Only RMEv that included both process indicators and outcomes (behavioural and/or health/safety outcomes) were eligible. Data were abstracted from reports, manuscripts and abstracts.
Results
Eighteen of 102 (18%) RMEv had both process indicators and outcomes, and were included in this review. Of the 18 RMEv, ten consisted of one study only, five of two studies, and three of three or more studies. A total of 30 studies were included within the 18 RMEv. The designs of the studies were: 19 (63%) cross-sectional surveys (47% targeted patients and 89% healthcare professionals), 17 (57%) retrospective studies (47% using pre/post approach) and 3 (10%) prospective studies. Nineteen studies included process indicators that were receipt (n = 14), use (n = 12), knowledge (n = 17) and self-reported behaviour (n = 15). Regarding outcomes, 67% of the 18 RMEv evaluated behavioural outcomes and 50% health/safety outcomes. Three of the 18 RMEv evaluated both behavioural and health/safety outcomes. For five RMEv, correlations between process indicators and outcomes were performed, two at the patient level. Results were available for 14 of the 18 RMEv. In healthcare professional surveys, the median percentage was 57% for receipt, 92% for reading, 80% for use, 77% for knowledge and 74% for behaviour. In patient surveys, the median percentage was 56% for receipt, 87% for reading, 65% for use, 47% for knowledge and 69% for behaviour. Knowledge was better in healthcare professionals than patients (p < 0.05). Of the three RMEv with a correlation analysis, only one found a positive trend for a lower occurrence of outcomes as process indicators improved, though this was not statistically significant.
Conclusions
A minority of RMEv assessed both process indicators and outcomes. More RMEv require approaches that correlate process indicators and outcomes at the patient level to evaluate more comprehensively the implementation of aRMMs.


Similar content being viewed by others
References
Rubino A, Artime E. A descriptive review of additional risk minimisation measures applied to EU centrally authorised medicines 2006–2015. Expert Opin Drug Saf. 2017;16:877–84.
European Medicines Agency. Guideline on good pharmacovigilance practices (GVP). Module VIII: post-authorisation safety studies (Rev 2). 2016. https://www.ema.europa.eu/en/documents/scientific-guideline/guideline-good-pharmacovigilance-practices-gvp-module-viii-post-authorisation-safety-studies-rev-2_en.pdf
European Medicines Agency. Guideline on good pharmacovigilance practices (GVP). Module XVI: risk minimisation measures: selection of tools and effectiveness indicators (Rev 2). 2017. https://www.ema.europa.eu/en/documents/scientific-guideline/guideline-good-pharmacovigilance-practices-module-xvi-risk-minimisation-measures-selection-tools_en-3.pdf
Rubino A, Artime E. A descriptive review of additional risk minimisation measures applied to EU centrally authorised medicines 2006-2015. Expert Opin Drug Saf. 2017; p. 1–8.
Artime E, Qizilbash N, Garrido-Estepa M, Vora P, Soriano-Gabarró M, Asiimwe A, et al. Are risk minimization measures for approved drugs in Europe effective? A systematic review. Expert Opin Drug Saf. 2019;18:443–54.
Vora P, Artime E, Soriano-Gabarró M, Qizilbash N, Singh V, Asiimwe A. A review of studies evaluating the effectiveness of risk minimisation measures in Europe using the European Union electronic Register of Post-Authorization Studies. Pharmacoepidemiol Drug Saf. 2018;27:695–706.
Mazzaglia G, Straus SMJ, Arlett P, da Silva D, Janssen H, Raine J, et al. Study design and evaluation of risk minimization measures: a review of studies submitted to the European Medicines Agency for cardiovascular, endocrinology, and metabolic drugs. Drug Saf. 2018;41:191–202.
YERVOY® risk minimization tool evaluation survey. https://www.encepp.eu/encepp/viewResource.htm?id=6951. Accessed 16 Oct 2020.
Evaluation of the effectiveness of Eliquis® (apixaban) risk minimization tools in European Economic Area (EEA) countries. https://www.encepp.eu/encepp/viewResource.htm?id=19658. Accessed 16 Oct 2020.
Evaluation of the effectiveness of the abatacept (Orencia®) intravenous and subcutaneous formulation patient alert Cards in patients with rheumatoid arthritis in a sample of European Economic Area countries. Available from: https://www.encepp.eu/encepp/viewResource.htm?id=31062. Accessed 16 Oct 2020.
Evaluation of the effectiveness of the belatacept (Nulojix®) patient alert card in patients following renal transplantation in European Economic Area countries. https://www.encepp.eu/encepp/viewResource.htm?id=22739. Accessed 16 Oct 2020.
Post Authorisation Safety Study (PASS) to evaluate the risks of hepatotoxicity and nephrotoxicity from administration of methoxyflurane (Penthrox®) for pain relief in hospital accident & emergency departments in the United Kingdom. https://www.encepp.eu/encepp/viewResource.htm?id=30864. Accessed 16 Oct 2020.
Evaluation of the effectiveness of Penthrox® (methoxyflurane) educational tools adopted as additional risk minimisation measures: healthcare professional and Patient Survey. https://www.encepp.eu/encepp/viewResource.htm?id=29622. Accessed 16 Oct 2020.
Jacquot E, Collin E, Ladner A, Tormos A, Hamm L, Perez-Gutthann S, et al. Agomelatine drug utilisation study in selected European countries: a multinational, observational study to assess effectiveness of risk-minimisation measures. Pharmaceut Med. 2019;33:311–9.
Objective assessment of metabolic monitoring in patients treated with Seroquel® or Seroquel® XR/quetiapine fumarate: use of IMS Disease Analyzer to assess physician behaviour in the UK and Germany. https://www.encepp.eu/encepp/viewResource.htm?id=20619. Accessed 16 Oct 2020.
Drug utilization study on the prescribing indications for CPA/EE in 5 European countries. https://www.encepp.eu/encepp/viewResource.htm?id=30829. Accessed 16 Oct 2020.
Nyeland ME, Laursen MV, Callréus T. Evaluating the effectiveness of risk minimisation measures: the application of a conceptual framework to Danish real-world dabigatran data. Pharmacoepidemiol Drug Saf. 2017;26:607–14.
Quinn D, Donegan K. Usage of valproate in women in the UK. Pharmacoepidemiol Drug Saf. 2016;25(Suppl.):3–680.
Mabthera drug utilisation study and patient alert card evaluation in non-oncology patients in Europe: an infusion centre based approach. https://www.encepp.eu/encepp/viewResource.htm?id=24913. Accessed 16 Oct 2020.
A drug utilization study in patients treated with Exelon®/Prometax® (rivastigmine) transdermal patch. https://www.encepp.eu/encepp/viewResource.htm?id=27280. Accessed 16 Oct 2020.
A drug utilisation study of domperidone in Europe using databases. https://www.encepp.eu/encepp/viewResource.htm?id=22405. Accessed 16 Oct 2020.
Drug utilisation study, in five European countries, using cross sectional analysis, to assess the extent of prescriptions of trimetazidine for its withdrawn ophthalmological and ENT indications among general practitioners, ophthalmologists and ENT special. https://www.encepp.eu/encepp/viewResource.htm?id=18050. Accessed 16 Oct 2020.
Evaluation of the effectiveness of risk minimization measures: trimetazidine drug utilization study in European countries using databases: analysis for France, Hungary, Romania and Spain. https://www.encepp.eu/encepp/viewResource.htm?id=28831. Accessed 16 Oct 2020.
Drug utilization study of cyproterone/ethinylestradiol (Diane®-35 and generics) in the Netherlands, UK and Italy. https://www.encepp.eu/encepp/viewResource.htm?id=31117. Accessed 16 Oct 2020.
Agyemang E, Bailey L, Talbot J. Additional risk minimisation measures for medicinal products in the European Union: a review of the implementation and effectiveness of measures in the United Kingdom by one marketing authorisation holder. Pharmaceut Med. 2017;31:101–12.
A joint Drug Utilisation Study (DUS) of valproate and related substances, in Europe, using databases. https://www.encepp.eu/encepp/viewResource.htm?id=32834. Accessed 16 Oct 2020.
Goedecke T, Morales DR, Pacurariu A, Kurz X. Measuring the impact of medicines regulatory interventions: systematic review and methodological considerations. Br J Clin Pharmacol. 2018;84:419–33.
Farcas A, Huruba M, Mogosan C. Study design, process and outcome indicators of post-authorization studies aimed at evaluating the effectiveness of risk minimization measures in the EU PAS Register. Br J Clin Pharmacol. 2019;85:476–91.
CIOMS Working Group IX. Practical approaches to risk minimisation for medicinal products: report of CIOMS Working Group IX. Geneva, Switzerland: Council for International Organizations of Medical Sciences (CIOMS); 2014.
Charlton RA, Bettoli V, Bos HJ, Engeland A, Garne E, Gini R, et al. The limitations of some European healthcare databases for monitoring the effectiveness of pregnancy prevention programmes as risk minimisation measures. Eur J Clin Pharmacol. 2018;74:513–20.
Goedecke T, Morales DR, Pacurariu A, Kurz X. Measuring the impact of medicines regulatory interventions: systematic review and methodological considerations. Br J Clin Pharmacol. 2018;84:419–33.
Pacurariu A, Plueschke K, McGettigan P, Morales DR, Slattery J, Vogl D, et al. Electronic healthcare databases in Europe: descriptive analysis of characteristics and potential for use in medicines regulation. BMJ Open. 2018;8:1–10.
The European Network of Centres for Pharmacoepidemiology and Pharmacovigilance (ENCePP). Guide on methodological standards in pharmacoepidemiology (Revision 7). EMA/95098/2010. https://www.encepp.eu/standards_and_guidances. Accessed 16 Oct 2020.
Møllebæk M, Kaae S, De Bruin ML, Callréus T, Jossan S, Hallgreen CE. The effectiveness of direct to healthcare professional communication: a systematic review of communication factor studies. Res Soc Adm Pharm. 2019;15:475–82.
European Network of Centres for Pharmacoepidemiology and Pharmacovigilance. ENCePP guide on methodological standards in pharmacoepidemiology. https://www.encepp.eu/standards_and_guidances/methodologicalGuide4_1_1.shtml. Accessed 19 Aug 2017.
Smith MY, Russell A, Bahri P, Mol PGM, Frise S, Freeman E, Morrato EH. The RIMES statement: a checklist to assess the quality of studies evaluating risk minimization programs for medicinal products. Drug Saf. 2018;41(4):389–401.
Russell AM, Morrato EH, Lovett RM, Smith MY. Quality of reporting on the evaluation of risk minimization programs: a systematic review. Drug Saf. 2020; p. 1–20.
The European Network of Centres for Pharmacoepidemiology and Pharmacovigilance (ENCePP). Annex 2 to the guide on methodological standards in pharmacoepidemiology. https://www.encepp.eu/standards_and_guidances. Accessed 16 Oct 2020.
Brosch S, de Ferran AM, Newbould V, Farkas D, Lengsavath M, Tregunno P. Establishing a framework for the use of social media in pharmacovigilance in Europe. Drug Saf. 2019;42:921–30.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
No funding was received for the preparation of this article.
Conflicts of interest/Competing interests
Nawab Qizilbash is an employee of OXON Epidemiology, a scientific service provider to the pharmaceutical industry that conducts PASS risk minimisation studies sponsored by companies. Esther Artime is an employee of Lilly Spain; however, this work was carried out as part of her doctoral thesis at Universidad Autónoma de Madrid, and therefore is not linked to her current work at Lilly. Rafael Herruzo and Macarena Garrido-Estepa have no conflicts of interest that are directly related to the content of this article.
Ethics approval
As this study was a review of existing literature, no ethical approval was required.
Consent to participate
Not applicable.
Consent for publication
Not applicable.
Availability of data and material
All data were extracted from existing study reports and publications that can be accessed on-line.
Code availability
Not applicable.
Authors’ contributions
EA, M-GE and NQ contributed to the conception and design of the article. The systematic search, data extraction and analysis were performed by EA and M-GE. The first draft of the manuscript was written by EA and all authors critically revised the work. All authors read and approved the final manuscript.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Artime, E., Qizilbash, N., Herruzo, R. et al. Risk Minimisation Evaluation with Process Indicators and Behavioural or Health Outcomes in Europe: Systematic Review. Pharm Med 34, 387–400 (2020). https://doi.org/10.1007/s40290-020-00361-w
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40290-020-00361-w