Abstract
Background
Cyproterone acetate 2 mg/ethinylestradiol 35 µg, an estrogen/progestogen treatment with anti-androgenic properties, shares a thromboembolism risk with combined hormonal contraceptives. Educational materials (i.e., direct healthcare professional communication, patient information card, prescriber checklist) were distributed to physicians to increase risk awareness.
Objective
The objective of this study was to measure physician knowledge of thromboembolism risk of cyproterone acetate 2 mg/ethinylestradiol 35 µg and ascertain whether physicians received the educational materials.
Methods
A cross-sectional web-based physician survey of recent prescribers of cyproterone acetate 2 mg/ethinylestradiol 35 µg in Austria, the Czech Republic, France, the Netherlands, and Spain was conducted. Sampling targets for physician specialty were based on country-specific prescribing patterns. Frequency of correct responses was calculated for 14 knowledge questions.
Results
Among 759 physician respondents (37% of obstetricians/gynecologists, 42% of general practitioners, 20% of dermatologists), 51% received one or more of three educational materials. Knowledge was highest (≥80%) for symptoms of possible deep vein thrombosis, pulmonary embolism, and cerebrovascular accident; most important risk factors for thrombosis; use in smokers; indication for moderate-to-severe acne; and understanding that cyproterone acetate 2 mg/ethinylestradiol 35 µg should not be used for contraception alone. Knowledge varied for contraindications, myocardial infarction symptoms, other risk factors for thrombosis, instructions regarding anticipated prolonged immobilization, and selected concomitant medical conditions. Knowledge was lower regarding prescribing cyproterone acetate 2 mg/ethinylestradiol 35 µg for acne only after failure of topical therapy or systemic antibiotics. Generally, knowledge did not vary by physician specialty, receipt of educational materials, number of patients prescribed cyproterone acetate 2 mg/ethinylestradiol 35 µg in the previous 3 months, and years in practice.
Conclusions
Knowledge was generally high for thromboembolism risk and varied for more complex or infrequent topics.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Physicians were surveyed to evaluate the receipt and understanding of educational materials on the safe use of cyproterone acetate 2 mg/ethinylestradiol 35 µg. |
Although physicians’ receipt of the materials varied, their knowledge of key safety information for cyproterone acetate 2 mg/ethinylestradiol 35 µg was high. |
Future research should explore optimal means of disseminating key safety information in the context of risk-minimization activities. |
1 Introduction
Diane®-35 [cyproterone acetate 2 mg/ethinylestradiol 35 µg (CPA/EE)], a combined estrogen/progestogen treatment with anti-androgenic properties, was first authorized in Europe in 1985 to treat androgenic conditions (i.e., acne, seborrhea, hirsutism, and alopecia) [1]. In 2013, the French National Agency for the Safety of Medicine and Health Products suspended the marketing of Diane®-35 and its generics, having attributed 125 cases of thrombosis and four deaths to CPA/EE products during a review of 25 years of historical data in France [1, 2]. The suspension of CPA/EE medications in France occurred in the midst of more general controversy over the use of third- and fourth-generation combined hormonal contraceptives [2, 3].
At the request of the French National Agency for the Safety of Medicine and Health Products [4], the European Medicines Agency’s Pharmacovigilance Risk Assessment Committee (PRAC) reviewed data related to the risks of thromboembolic events based on results from clinical studies, pharmacoepidemiological studies, published literature, post-marketing experience on the safety of these medications, and submissions from stakeholders [1]. The PRAC determined that the risk of venous thromboembolism with CPA/EE medications is 1.5–2.0 times higher than for combined oral contraceptives containing levonorgestrel and may be similar to the risk associated with contraceptives containing gestodene, desogestrel, or drospirenone [1, 5]. Information on the risks of arterial thromboembolism associated with these medications is sparse but indicates that this risk is lower than the risk of venous thromboembolism [5]. The review also identified widespread off-label use of CPA/EE as a contraceptive only and use of CPA/EE concomitantly with other hormonal contraceptives in multiple European countries [1].
Based on the review, the Coordination Group for Mutual Recognition and Decentralised Procedures—Human endorsed the recommendation of the PRAC, which concluded that the benefits of CPA/EE outweigh the risks, provided that several measures were taken to minimize the risk of venous thromboembolism [6]. The indication for CPA/EE was revised to the treatment of moderate-to-severe acne related to androgen sensitivity (with or without seborrhea) and/or hirsutism in women of reproductive age [1]. For the treatment of acne, CPA/EE should be used only after topical therapy or systemic antibiotic treatments have failed [1]. Cyproterone acetate 2 mg/ethinylestradiol 35 µg should not be used in combination with other hormonal contraceptives [1].
The PRAC also recommended that educational materials [i.e., a direct healthcare professional communication (DHPC), patient information card, and prescriber checklist] be distributed to physicians focusing on thromboembolism and its risks factors, signs, and symptoms and contraindications relevant to thromboembolism. Marketing authorization holders were required to evaluate the effectiveness of these risk-minimization communications and to publish the results of the evaluation. Five European countries were selected for this evaluation: Austria, the Czech Republic, France, the Netherlands, and Spain. No evaluations were conducted outside of the European Union.
After the outcome of the PRAC referral procedure and finalization of the educational materials, translation and country-specific dissemination of the educational materials, as well as the target groups of healthcare providers in each country, were subsequently agreed with the respective national competent authorities. The national competent authority approval timelines varied between member states; first approvals were gained in July 2014 in Austria and the Czech Republic, whereas there was a delay in approval in Spain owing to the regulatory review, which was received in April 2015. Educational materials were disseminated through various channels (e.g., post-mailed hard copies, sales representatives, country websites). The timing of dissemination varied by country, from July 2014 in the Czech Republic to April 2015 in Spain. The time from distribution of the educational materials to the start-up of data collection ranged from approximately 5 months in Spain to 13 months in France.
The current study was classified as a post-authorization safety study conducted to address the European Medicine Agency’s requests for an evaluation of the effectiveness of the educational materials related to the risk-minimization measures for CPA/EE and to communicate the findings of this evaluation. Specifically, the objectives of this study were to assess whether physicians received the educational materials and to measure physicians’ knowledge of the risk factors of thromboembolism, signs and symptoms of thromboembolism, and contraindications for prescribing CPA/EE.
2 Methods
2.1 Study Design
The study was an observational cross-sectional survey of the knowledge, understanding, and self-reported behavior among a sample of physicians with recent experience with CPA/EE in Austria, the Czech Republic, France, the Netherlands, and Spain. These countries were selected for their diversity in size, geographic location, and the volume of CPA/EE use in each country. These decisions were discussed and agreed on with the PRAC before the studies were initiated.
Based on CPA/EE prescribing patterns in each country, the study specifically targeted gynecologists and dermatologists in Austria and the Czech Republic; general practitioners (GPs) and dermatologists in the Netherlands; and GPs, gynecologists, and dermatologists in France and Spain. Inclusion of up to 25% dermatologists was targeted in each country. In France, Spain, and the Netherlands, a random sample of potentially eligible physicians in each specialty of interest was recruited by e-mail from an online physician panel. In Austria and the Czech Republic, where the physician panel sizes were limited, all physicians in each specialty of interest on the panels were invited to participate, and additional physicians were recruited via telephone from a proprietary database and publicly available sources.
The study aimed to recruit 60–120 physicians each in Austria, the Czech Republic, and the Netherlands and 100–200 physicians each in France and Spain, for a total of at least 500 participating physicians. These sample sizes, which were approved by the PRAC, were anticipated to be sufficient to support the planned analyses and to allow reasonable precision around estimates of knowledge and understanding of the key safety information for the total sample and within each country to the extent possible. To participate, physicians must have been a licensed and practicing dermatologist, gynecologist, or GP (i.e., general medicine, family practice, internal medicine) and prescribed CPA/EE to at least one patient in the previous 6 months. The study complied with all local regulatory and ethical requirements and was approved by the RTI International Institutional Review Board. All participants who completed the survey provided informed consent.
2.2 Survey Design and Administration
The 24-item questionnaire was developed using best practices for instrument development [7]. The questionnaire was tested through in-person cognitive interviews with physicians in each country before data collection to optimize the questionnaire items, wording, and response choices and to ensure consistency across cultures and languages.
The questionnaire contained screener questions to confirm eligibility; an informed consent question; closed-ended multiple-choice questions to measure study objectives; questions to characterize the physicians and their practices; and questions to investigate physician receipt and use of educational materials related to CPA/EE. The questionnaire, which is included in the study protocol, is posted in the European Union Post-Authorisation Studies register [8]. The questionnaire items are included as ‘Online Resource 1’ in the Electronic Supplementary Material (ESM) accompanying this article.
Invitations to complete the web-based survey were sent via e-mail to the selected sample of physicians. Interested physicians logged into the study website by entering a unique identification number and password.
Physicians were not able to modify answers to previous questions, which minimized their likelihood of searching for answers or changing responses based on content in subsequent questions. The physician survey was initiated in each country after a period sufficient to allow prescribers to have received the educational materials and use the information in their practice. Data collection ran from 26 June, 2015 to 21 February, 2016.
2.3 Statistical Methods
Data analyses were descriptive and focused on summarizing the frequencies and percentages of survey responses in eligible participants who provided informed consent. The percentages for individual questionnaire responses were based on the number of participants, which included missing responses for those who did not answer the question. No imputation of missing responses was performed.
Descriptive responses were generated for all countries combined and stratified by country. Stratifications were also conducted by physician specialty, years practicing medicine, receipt of educational materials, and number of patients prescribed to in the previous 3 months. Although eligibility to complete the survey was based on prescribing CPA/EE in the past 6 months, the specific question regarding how many patients had been prescribed CPA/EE was limited in duration to the previous 3 months to minimize the effect of recall bias in the response to this question.
Demographic (sex and age) and practice characteristics (physician specialty, type of practice, years practicing medicine, number of patients prescribed to in the previous 3 months) were collected for physicians who completed the survey and were compared with those of non-participants (see ‘Online Resource 2’ in the ESM accompanying this article). All analyses were performed using SAS software, Version 9.4 (SAS Institute, Inc., Cary, NC, USA, 2002–2012).
3 Results
3.1 Demographics and Clinical Practice Characteristics
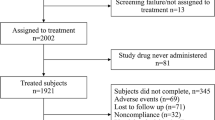
Of the 11,102 physicians invited to participate, 759 physicians completed the survey. Data-collection efforts were stopped once the country-specific targets were met. Table 1 presents the sample characteristics. The percentage of physicians completing the survey ranged from 3.9% in France to 12.5% in the Netherlands (Table 2).
3.2 Knowledge Questions
3.2.1 Summary of Key Concepts with High Knowledge
Across countries, physicians’ knowledge was high with regard to the individual symptoms of deep vein thrombosis, pulmonary embolism, or cerebrovascular accident; the most important risk factors for thrombosis; the recommendation that women aged older than 35 years should stop smoking or use non-hormonal treatment for acne or hirsutism; the fact that CPA/EE is approved for moderate-to-severe acne; and the fact that CPA/EE should not be used for contraception alone. Most physicians (≥80%) reported correct responses to questions on these topics.
3.2.2 Knowledge of Risks of Thrombosis
Physicians’ knowledge of the time periods during which the risk of thrombosis is highest varied (question 10). Overall, 89.3% of physicians (and a generally consistent proportion of physicians across countries) correctly indicated that the risk was greatest during the first year of use (Fig. 1). In contrast, 65.2% of physicians overall correctly indicated that the risk was greatest after a break of 1 month or more.
Physicians’ knowledge of situations when a patient may show symptoms of a thrombosis (question 12) was high overall (95.5–98.9%) for three of the four situations: just after having an operation, when the patient has been off her feet for a long time, and during or after a long journey (Fig. 2). Knowledge was lower, 75.5% overall, for the situation of initiating treatment with CPA/EE within a few weeks after having a baby.
Physicians’ knowledge of medical conditions and other factors that can increase the risk of thrombosis varied (Figs. 3, 4). Physicians’ knowledge of the six medical conditions that can increase the risk of thrombosis (question 17) was highest for cancer (95.5% overall) and systemic lupus erythematosus (86.0% overall) (Fig. 3). Knowledge was 68.0% overall for diabetes mellitus and ranged from 44.7 to 59.8% overall for the other three medical conditions (i.e., hemolytic uremic syndrome, chronic inflammatory bowel disease, sickle cell disease). The percentage of physicians who selected five of the six correct responses for this question was 42.4% overall. Regarding the 12 risk factors associated with the potential development of thrombosis (question 15), physicians’ knowledge ranged from 81.4 to 96.8% for eight of the possible risk factors (Fig. 4). Overall, physicians’ knowledge of the other risk factors was variable (diabetes mellitus, 62.2%; having given birth in the previous few weeks, 74.3%; patient or immediate family member has dyslipidemia, 42.2%; history of migraines, 54.9%). Approximately three quarters (71.0%) of physicians overall selected at least nine of the 12 correct responses.
Correct responses to question 15: Which of the following risk factors for the development of thrombosis should be considered prior to prescribing CPA/EE? BMI body mass index, CPA/EE cyproterone acetate 2 mg/ethinylestradiol 35 µg. aHypertension defined as systolic blood pressure of 140–159 mmHg or diastolic blood pressure of 90–99 mmHg. bAnswer choice was worded as “The patient has a close relative (e.g., parent or sibling) who has had a thromboembolic event at a young age (e.g., before 50)”. cFamily was described as “immediate family”. dCardiovascular conditions included atrial fibrillation, arrhythmia, coronary heart disease, and cardiac valve disease. eMedical conditions included cancer, systemic lupus erythematosus, sickle cell disease, Crohn’s disease, ulcerative colitis, and hemolytic uremic syndrome. fMedicines included corticosteroids, neuroleptics, antipsychotics, antidepressants, and chemotherapy
3.2.3 Knowledge of Symptoms of Myocardial Infarction
Physicians’ knowledge of the three specific myocardial infarction symptoms (i.e., chest pain; chest discomfort, pressure, or heaviness; radiating upper body discomfort together with a feeling of fullness associated with indigestion or choking) [question 20] was high: 95.7–98.8% overall (Fig. 5). Knowledge of the three unspecific symptoms (i.e., sweating, nausea or vomiting, dizziness) ranged from 42.8 to 51.9% overall. Approximately 47% of physicians selected at least five of six correct responses.
Correct responses to question 20: A patient should be advised to seek immediate medical attention for which of the following symptoms of a possible myocardial infarction? aUpper body discomfort described as radiating to the back, jaw, throat, and arm together with a feeling of fullness associated with indigestion or choking
3.2.4 Knowledge of Instructions for Patients
Physicians’ knowledge varied overall and across countries with regard to the four instructions that should be provided to patients when a patient might need major surgery or experience an injury or condition that may require a period of prolonged immobilization (question 13) (Fig. 6). Knowledge was high overall (97.2%) for informing patients to tell their doctor, nurse, or surgeon that they are taking CPA/EE. Physicians’ knowledge was lower for instructing patients to use a non-hormonal treatment for their skin condition and, if necessary, a non-hormonal method of contraception during this time (67.1% overall). Physicians’ knowledge of instructing a patient to stop using CPA/EE for at least 4 weeks before a major surgery or prolonged immobilization was 47% overall. Similarly, physicians’ knowledge of instructing patients to resume treatment with CPA/EE at least 2 weeks or later after complete remobilization was 59.9% overall. The percentage of physicians who selected at least three of the four correct responses for this question was 58.4% overall.
3.2.5 Knowledge of Indications and Contraindications
Correct knowledge that CPA/EE is indicated for moderate-to-severe acne related to androgen sensitivity (with or without seborrhea) in women of reproductive age (question 8) was reported by 92.0% of physicians (Fig. 7). Approximately half of physicians (47.7%) were aware that CPA/EE should be prescribed for acne only after topical therapy or systemic antibiotics have failed. Correct knowledge that CPA/EE should not be used for contraception alone in women of reproductive age was reported by 81.4%. A smaller percentage of physicians (69.2%) were aware that CPA/EE was indicated for hirsutism, and approximately one third of physicians (34.0%) were aware that androgenic alopecia was no longer an indication.
Physicians’ knowledge varied for contraindications for CPA/EE (question 14). Knowledge was high overall (92.2–98.8%) for three of the nine contraindications: patients who have a current event or history of a thromboembolic event, patients who have knowledge of a predisposition for a blood clotting disorder, and patients who are experiencing or expected to experience a period of prolonged immobilization (Fig. 8). Knowledge was lower overall (71.0–78.7%) for three of the nine contraindications: patients with diabetes mellitus and concurrent vascular complications, patients with hypertension, and patients who have had a recent major surgery. Knowledge regarding contraindications for patients who are currently using another hormonal contraceptive, for patients with a history of migraine with aura, and for patients with dyslipidemia was 68.0, 59.9, and 59.3%, respectively.
Percentage of physicians reporting correct responses to question 14: CPA/EE are contraindicated in which of the following patient populations? CPA/EE cyproterone acetate 2 mg/ethinylestradiol 35 µg. aBlood clotting disorders included deep vein thrombosis, pulmonary embolism, myocardial infarction, cerebrovascular accident, transient ischemic attack, and angina pectoris. bHypertension is defined as systolic blood pressure of 160 mmHg or diastolic blood pressure of 100 mmHg
3.3 Additional Stratifications
Knowledge did not vary for most questions based on the additional stratifications by physician specialty, years practicing medicine, number of patients prescribed to in the previous 3 months, and receipt of educational materials, with a few exceptions. Knowledge did vary by physician specialty for three questions (i.e., 9, 13, and 14). For question 9 (i.e., treatment of acne only after topical therapy or systemic antibiotic treatments have failed), the percentage of correct responses was highest among GPs (59.2%) and dermatologists (45.8%) compared with obstetricians/gynecologists (OBs/GYNs) (35.6%). For question 13 (i.e., instructions regarding major surgery, or an injury or condition that may require a period of prolonged immobilization), the percentage of physicians who selected at least three of the four correct responses was highest for OBs/GYNs (70.8%) compared with GPs (53.0%) and dermatologists (47.1%). For question 14 (contraindications), the percentage of physicians who selected at least seven of the nine correct responses was highest among OBs/GYNs (76.5%) compared with GPs (64.3%) and dermatologists (52.9%).
Knowledge was higher for physicians who reported receipt of the educational materials for two questions (i.e., 13 and 14). Knowledge varied by the number of patients prescribed CPA/EE in the previous 3 months for question 9 and by years practicing medicine for question 13. Specifically, a larger percentage of physicians who had prescribed CPA/EE to 0 to 3 patients in the previous 3 months vs. more than three patients reported correct responses to question 9 (54.7 vs. 39.6%). The percentage of physicians who selected at least three of the four correct responses to question 13 was higher for physicians who had been practicing medicine longer (65.5% for physicians practicing >25 years and 61.3% for 16–25 years vs. 47.0% for 0–15 years).
3.4 Receipt of Educational Materials
The percentage of physicians who reported receiving at least one of the three educational materials was 51.0% overall. Specifically, 45.5% of physicians overall [range, 17.8% (Austria) to 86.7% (Czech Republic)] reported receiving the DHPC. In addition, 16.2% of physicians overall [range, 7.4% (the Netherlands) to 41.7% (Czech Republic)] reported receiving the patient card, and 16.9% of physicians overall [range, 9.0% (Spain) to 27.5% (Czech Republic)] reported receiving the prescriber checklist. In the overall sample, a larger percentage of OBs/GYNs reported receiving any of the three CPA/EE educational materials (from 27.0% for the prescriber checklist to 54.8% for the DHPC) compared with dermatologists (from 13.5% for the prescriber checklist and patient card to 41.3% for the DHPC) and GPs (from 7.2% for the patient card to 39.2% for the DHPC). Most physicians (81.0%) who received at least one of the CPA/EE materials reported finding it helpful or extremely helpful.
4 Discussion
This study sought to evaluate physicians’ receipt of educational materials regarding safe use of CPA/EE and their understanding of key safety information. One of the most important factors in prescribing a combined estrogen/progestogen treatment is the physician’s knowledge of the risks associated with the potential development of thromboembolism and their subsequent communication of these risks to patients. The questions with the greatest percentage of correct responses (≥80%) were (1) symptoms of possible deep vein thrombosis, pulmonary embolism, and cerebrovascular accident; (2) most important risk factors for thrombosis; and (3) instructions for use in smokers. Knowledge regarding the indicated use of CPA/EE for moderate-to-severe acne related to androgen sensitivity (with or without seborrhea) was 92%, and knowledge about the avoidance of its use for contraception alone in women of reproductive age was 81.4%. A smaller percentage of physicians (69.2%) was aware of the indicated use of CPA/EE for hirsutism. Approximately one third of physicians (34.0%) were aware of the revised indication related to removal of the androgenic alopecia indication, and approximately half of physicians (47.7%) were aware of prescribing for acne only after failure of topical therapy or systemic antibiotics. The percentage of physicians who responded correctly was variable for contraindications (59.3–98.8% across specific contraindications), symptoms of possible myocardial infarction (42.8–98.8% across specific symptoms), other general risk factors for thrombosis (42.2–96.8% across specific risk factors), instructions related to immobilization (47.0–97.2% across specific instructions), and selected concomitant medical conditions (44.7–95.5% across specific concomitant medical conditions). Physicians’ receipt of CPA/EE educational materials varied; however, most physicians who received at least one of the materials reported that they found it helpful or extremely helpful.
The relatively low level of reported receipt of the educational material may reflect poor recall, if the material had indeed been received, or various reasons for not receiving the educational material. Variability across countries could reflect inherent differences in physician behavior or different intensities of educational efforts. Little information is in the public domain regarding the percentage of physicians who report receipt of educational materials based on results from post-authorization safety studies. A recent publication reported the results of a multi-national survey of 800 European physicians assessing the receipt of educational materials: for that study, physicians’ reported receipt of the educational materials ranged from 16.0 to 69.0% across the participating countries [9]. Of the 37.4% physicians overall who reported having received the educational materials, 90.6% reported that they had read the materials, whereas 4.0% had not read them and 5.4% could not recall whether they had read them [9]. Our study found that more than half (51.0%) of physicians had received at least one of the three CPA/EE educational materials (but did not evaluate whether physicians had read the materials).
The high level of knowledge of risks despite the low reported receipt of the educational material may indicate that other sources of information are effective in risk communication. The high visibility of the marketing suspension of CPA/EE in France and the long-standing controversies on the safety of oral contraceptives may have increased knowledge about this product, even though CPA/EE is not indicated as a contraceptive.
In addition, there is no consensus within the research community on a priori thresholds for acceptable levels of knowledge and behavior to be able to determine the success of risk-minimization plans. A recent publication reported on patient understanding of medication guides from a review of 66 assessment reports submitted to the US Food and Drug Administration [10]. A total of 30.3% of reports achieved an 80% knowledge level (percentage correct) for the single most important risk communicated in the medication guide, for a mean knowledge level of 63.8% [10].
Several studies have proposed conceptual frameworks or models to assess the effectiveness of risk-minimization measures and have identified many challenges and methodological gaps [11,12,13,14,15,16]. Banerjee and colleagues [11] proposed a five-level hierarchical model, where “distribution of educational material” and “knowledge” are at the lower end and “prescriber behaviour” and “safety outcomes” are at the higher end and are considered most relevant for the evaluation of the effectiveness of risk-minimization measures. In addition to physicians’ knowledge of key safety information for CPA/EE and their use of educational materials, as described in the current study, research has evaluated prescriber behavior in the context of risk-minimization measures for CPA/EE [17, 18].
This study is characterized by several strengths. The targeted enrollment in each country was achieved, and the sample was diverse. The physician survey was conducted after physicians had the opportunity to receive and use the CPA/EE educational materials, allowing for evaluation of their understanding of key safety information and application of the educational materials in clinical practice. Accuracy of responses among physicians was facilitated by cognitive pretesting of the questionnaire.
Some limitations inherent to cross-sectional physician surveys must also be considered. Although the study aimed to select a diverse and representative sample of prescribers, there exists no exhaustive list of all prescribers of CPA/EE from which to draw a sample, and random sampling was not possible. Thus, the study participants may not necessarily represent all relevant prescribers. Moreover, it is possible that participants who completed the questionnaire differed from non-participants in characteristics that were not measured in the questionnaire. Physician response rates for surveys historically have been somewhat low, and low response rates may increase the likelihood that participating physicians are not representative of all prescribing physicians. In this study, the completion percentages reflected early responses and truncation of the survey once target numbers had been met. Thus, the resulting estimates of physician understanding about CPA/EE may be biased. In addition, physicians’ knowledge of the key safety information for CPA/EE before distribution of the educational materials was not evaluated; therefore, changes in knowledge and awareness prompted by distribution of the educational materials could not be evaluated. Finally, there was heterogeneity of some results by country; it is unknown how generalizable the results are to other countries.
5 Conclusions
The observed patterns of knowledge among surveyed physicians regarding the safe use of CPA/EE were as expected, with the greatest knowledge on the indicated use and most important risks emphasized in the educational material and other product information. Although almost half of the physicians did not report receiving the educational materials, their high level of knowledge suggests that the key safety information may be available to them elsewhere. Additional research should explore the optimal format and channels for educational materials (e.g., e-mail, social media, educational sessions) to improve physicians’ receipt and retention of information on safe use.
References
European Medicines Agency. Assessment report cyproterone acetate/ethinylestradiol (2 mg/0.035 mg) containing medicinal products; 2013. http://www.ema.europa.eu/docs/en_GB/document_library/Referrals_document/cyproterone_ethinylestradiol_107i/Recommendation_provided_by_Pharmacovigilance_Risk_Assessment_Committee/WC500144130.pdf. Accessed 4 May 2016.
Cox L. The bitter pill. J Fam Plann Reprod Health Care. 2015;41:81–3.
Arie S. French doctors are told to restrict use of third and fourth generation oral contraceptives. BMJ. 2013;346:f121.
European Medicines Agency. PRAC recommendations on Diane®-35; 2013. http://www.ema.europa.eu/docs/en_GB/document_library/Referrals_document/cyproterone_ethinylestradiol_107i/Recommendation_provided_by_Pharmacovigilance_Risk_Assessment_Committee/WC500143491.pdf. Accessed 4 May 2016.
European Medicines Agency. Benefits of Diane®-35 and its generics outweigh risks in certain patient groups; 2013. http://www.ema.europa.eu/docs/en_GB/document_library/Referrals_document/cyproterone_ethinylestradiol_107i/Position_provided_by_CMDh/WC500143778.pdf. Accessed 21 March 2016.
European Medicines Agency. Cyproterone and ethinylestradiol containing medicinal products; 2013. http://www.ema.europa.eu/ema/index.jsp?curl=pages/medicines/human/referrals/Cyproterone_and_ethinylestradiol_containing_medicinal_products/human_referral_prac_000017.jsp&mid=WC0b01ac05805c516f. Accessed 4 May 2016.
Pew Research Center. Questionnaire design. http://www.pewresearch.org/methodology/u-s-survey-research/questionnaire-design/. Accessed 21 June 2017.
Andrews E, Perez-Gutthann S, Davis K, Zografos L, Hollis K. Study to evaluate physician knowledge of safety and safe use information for Diane-35 and its generics in Europe: an observational post-authorisation safety study. Protocol version 2.0; 2015. Prepared for marketing authorisation holder: Bayer AG. http://www.encepp.eu/encepp/openAttachment/fullProtocolLatest/9674. Accessed 22 Sept 2016.
Brody RS, Liss CL, Wray H, Iovin R, Michaylira C, Muthutantri A, et al. Effectiveness of a risk-minimization activity involving physician education on metabolic monitoring of patients receiving quetiapine: results from two postauthorization safety studies. Int Clin Psychopharmacol. 2016;31:34–41.
Knox CA, Hampp C, Willy M, Winterstein AG, Dal Pan G. Patient understanding of drug risks: an evaluation of medication guide assessments. Pharmacoepidemiol Drug Saf. 2015;24:518–25.
Banerjee AK, Zomerdijk IM, Wooder S, Ingate S, Mayall SJ. Post-approval evaluation of effectiveness of risk minimisation: methods, challenges and interpretation. Drug Saf. 2014;37:33–42.
Council for International Organizations of Medical Sciences (CIOMS). Chapter V. Evaluating effectiveness of risk minimisation. In: Practical approaches to risk minimisation for medicinal products: report of CIOMS Working Group IX. Geneva: Council for International Organizations of Medical Sciences; 2014. pp. 53–74.
Kesselheim AS, Campbell EG, Schneeweiss S, Rausch P, Lappin BM, Zhou EH, et al. Methodological approaches to evaluate the impact of FDA drug safety communications. Drug Saf. 2015;38:565–75.
Prieto L, Spooner A, Hidalgo-Simon A, Rubino A, Kurz X, Arlett P. Evaluation of the effectiveness of risk minimization measures. Pharmacoepidemiol Drug Saf. 2012;21:896–9.
Nyeland ME, Laursen MV, Callréus T. Evaluating the effectiveness of risk minimisation measures: the application of a conceptual framework to Danish real-world dabigatran data. Pharmacoepidemiol Drug Saf. 2017;26(6):607–14.
Gridchyna I, Cloutier A-M, Nkeng L, Craig C, Frise S, Moride Y. Methodological gaps in the assessment of risk minimization interventions: a systematic review. Pharmacoepidemiol Drug Saf. 2014;23:572–9.
European Network of Centres for Pharmacoepidemiology and Pharmacovigilance. Drug utilization study on the prescribing indications for CPA/EE in 5 European countries. http://www.encepp.eu/encepp/viewResource.htm?id=16974. Accessed 14 July 2017.
European Network of Centres for Pharmacoepidemiology and Pharmacovigilance. Drug utilization study on Diane®-35 (and generics) in European healthcare databases. http://www.encepp.eu/encepp/viewResource.htm?id=16504. Accessed 14 July 2017.
Acknowledgements
The authors thank Alexander Michel, Ulrike Wissinger-Graefenhahn, Mary Murphy, Suzanne Frankfort, Hissba Tus Saboor Khan, Michael Kunz, and Vita Beckert of Bayer AG for their assistance with the review of study documents and other study activities. Kate Lothman of RTI Health Solutions provided medical writing services, which were funded by Bayer AG.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
This study and preparation of this article were funded by Bayer AG.
Conflict of interest
Kimberly H. Davis, Laurie J. Zografos, David J. McSorley, and Elizabeth B. Andrews are employees of RTI Health Solutions, which received funding from Bayer AG to conduct this study. The contract between RTI Health Solutions and the sponsor includes independent publication rights. RTI International, of which RTI Health Solutions is a part, conducts work for government, public, and private organizations, including pharmaceutical companies. Alex Asiimwe is a full-time employee of Bayer AG.
Ethics approval
All procedures performed in this study involving human participants were in accordance with the ethical standards of the applicable institutional review board and ethics committees and with the 1964 Declaration of Helsinki and its later amendments or comparable ethical standards.
Consent to participate
Informed consent was obtained from all individual participants included in the study.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution-NonCommercial 4.0 International License (http://creativecommons.org/licenses/by-nc/4.0/), which permits any noncommercial use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
About this article
Cite this article
Davis, K.H., Asiimwe, A., Zografos, L.J. et al. Evaluation of Risk-Minimization Activities for Cyproterone Acetate 2 mg/Ethinylestradiol 35 µg: A Cross-Sectional Physician Survey. Pharm Med 31, 339–351 (2017). https://doi.org/10.1007/s40290-017-0203-9
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40290-017-0203-9