Abstract
Background
Mechanisms underlying safety events may be heterogeneous and depend on conditions of development and marketing, including the populations studied in clinical trials and the amount of data required for approval, especially under pathways for accelerated access.
Objective
This study was conducted to investigate possible factors affecting the first post-marketing safety-related regulatory actions (SRRAs) after launch of new drugs in Japan.
Methods
We studied 338 new molecular entities (NMEs) approved in Japan between 2004 and 2014. We focused on three different types of SRRAs: (1) all-SRRAs (i.e. SRRAs from domestic cases and other countries), (2) domestic-SRRAs (i.e. SRRAs from domestic cases) and (3) domestic unknown-SRRAs (i.e. SRRAs of unknown risks from domestic cases). Occurrences of the three types of SRRAs were analyzed using Kaplan–Meier analysis and Cox-regression.
Results
SRRAs tended to occur sooner for NMEs launched in recent years versus those launched towards the beginning of the study period. Risk of SRRA was high for antineoplastics. Drugs for cardiovascular diseases, central nervous system, and diabetes had positive associations with all-SRRAs, but the associations were weaker with domestic-SRRAs. Domestic-SRRAs were more likely for drugs with relatively novel modes of action (MOAs). Longer lag to Japanese launch after first global launch significantly lowered SRRA risks. While most of the variables showed similar associations across the three types of SRRAs, adoption of bridging strategies showed higher risks only for domestic-SRRAs, not for all-SRRAs. FDA safety labeling changes and non-orphan priority review drugs presented higher domestic-SRRA risks. The number of adverse drug reactions (ADRs) from spontaneous reports had positive correlations with the three types of SRRAs, whereas the number from company-led surveillance showed no association.
Conclusions
Our results indicated that global clinical development pathways and marketing status should be considered more seriously in implementing locally optimized pharmacovigilance activities. Caution may be needed not only for drugs with novel MOAs, but also for drugs for which local dose-finding studies have been skipped, expedited review status has been given, timing of launch is close to those in the USA and the EU, and spontaneous reports rather than company-lead surveillance suggest possible safety risks.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Regulatory agencies and drug companies take safety-related regulatory actions (SRRAs) based on domestic and global information available and potential global impact. |
Occurrences of SRRAs after marketing of new drugs are closely connected with accumulation of information. |
Clinical development background (e.g. bridging strategy) and global marketing status (e.g. global launch sequence and lag) should be considered in post-marketing surveillance plans. |
1 Introduction
The safety risks after launching innovative new drugs have historically been a focal issue in pharmaceutical regulation [1, 2]. This is because the safety profiles of drugs with new modes of action (MOAs) are not fully characterized at approval due to limited patient exposure during clinical development. Furthermore, accelerated approval pathways recently implemented, such as “breakthrough therapy designation” in the USA [3], “PRIME” status in the European Medicines Agency (EMA) [4], and the “SAKIGAKE designation” in Japan [5], potentially compound the issue by facilitating access to innovative drugs with even less available data.
In light of these recent regulatory trends that might realize tradeoffs between early access and safety, post-marketing safety measures have become increasingly important. Regulations for pharmacovigilance were harmonized by ICH E2E Pharmacovigilance Planning in 2005, and post-marketing safety measures have been strengthened by the enforcement of the Risk Management Plan (RMP) in Europe in 2005 and Risk Evaluation and Mitigation Strategies in the USA in 2008. Japan was early in adopting new drug surveillance programs for marketing authorization holders, such as post-marketing surveillance (PMS) in 1993, all-case surveillance, and early post-marketing phase vigilance in 2001. The RMP has been mandatory since 2014 [6, 7].
In previous studies, associations between post-marketing risks and related factors, such as drug characteristics, drug development background, and regulations, were discussed using safety-related regulatory actions (SRRAs) as an index of safety risks [1, 8]. Studies generally suggested that unexplained safety profiles related to new MOAs, drug class, seriousness of diseases targeted by new drugs, small numbers of trial subjects, and insufficient overseas safety information at approval may yield frequent SRRAs. It has been reported that rich post-marketing safety information in other countries decreases the frequency of SRRAs in Japan [8, 9]. Employing bridging strategies performed according to ICH-E5 or global clinical trials may mean less safety data is required for approval. The new drug application review period was reported to be associated with safety events [10, 11]. New drugs receiving priority review may have benefit/risk balances at approval different from those receiving standard review, resulting in a greater number of SRRAs. From the perspective of post-marketing, the increase of patient exposures and the number of patients with diverse backgrounds by expansion of indication may yield more SRRAs. However, the SRRAs are issued as safety measures for risks, which can be identified as known or unknown according to the information on adverse drug reactions (ADRs) collected by domestic pharmacovigilance activities, information from other countries, and safety data of similar drugs, including class-effects.
Safety risks tend to appear in increasingly complicated ways in this age of globalization. As drug companies usually implement clinical development for new drugs worldwide, a typical clinical data package consists of clinical data obtained in several countries. Regulatory approval decisions sometimes depend on the decisions of other countries/regions. Marketing strategy is orchestrated globally, and safety information, both pre- and post-marketing, transcends national borders and affects safety measures in other countries [12]. Even when our interest is on safety measures in a specific country, we somehow need to consider information from all of these sources in a rigorous way.
We took notice of the fact that SRRAs are heterogeneous; some reflect domestic cases, and others reflect foreign cases and/or changes in labeling. They have different triggers and serve different purposes. Therefore, instead of handling SRRAs as one single target, as in previous studies, we classified SRRAs into three groups according to where the ADRs were observed and whether they were known or unknown (see Table 1). Since these three SRRA groups were expected to represent different types of risks, we hypothesized that analysis of these SRRAs may lead to important clues as to how safety measures are taken under different conditions.
We used each SRRA as the objective variable and investigated the relationships between the SRRAs and various factors, including drug characteristics, development background and approval review, surveillance program, types of ADR reports, and regulatory environments. The association between SRRAs and first-in-class drugs, and the accumulation of the safety information on the new MOA, were also of interest, as it has been reported that clinically significant ADRs are more commonly added to package inserts between two and three years after the launch of new molecular entities (NMEs) in Japan [9].
2 Methods
Safety information on NMEs approved in Japan between 2004 and 2014 was collected from the Pharmaceutical and Medical Devices Agency (PMDA) website. A SRRA was defined as the issuance of a ‘Yellow letter (urgent safety information)’, a ‘Blue letter (rapid safety information)’, or an official notification from the Ministry of Health, Labour and Welfare (MHLW), as was defined in a previous study [8]. In Japan, major revision(s) of warning, contraindications, precautions, and clinically significant adverse reactions in package inserts are conveyed to healthcare professionals through the three documents above, depending on urgency and seriousness of safety risks. No ‘Yellow letters’ were issued during our observation period. Information on SRRAs was available on the PMDA website.
Drug characteristics (e.g. new MOA, drug class), drug development background (e.g. subject size, development plan), review and post-marketing regulation (e.g. review period, priority review status, all-case surveillance), post-marketing activities (e.g. indication expansion) were obtained from the review reports and common technical documents on the PMDA website. Japanese ADRs were extracted from the Japanese Adverse Drug Event Report database (JADER). Launch lag and patient exposure were estimated using QuintilesIMS Life-cycle® and IMS-JPM®, QuintilesIMS Health Japan, respectively. Changes in drug labels in the USA were collected from the FDA website.
We first investigated whether the frequency and timing of all observed SRRAs changed in the past decade using the Kaplan–Meier analysis. Then, by using the Cox proportional hazard regression model, we analyzed the follow-up period from the launch of a new drug until the issue of the first SRRA related to each of the three types of events as mentioned below.
Three types of events were independently investigated in the Cox regression; (1) all-SRRAs (i.e. SRRAs of observed risks of any kind from domestic cases and other countries), (2) domestic-SRRAs (i.e. SRRAs of risks of any kind detected from domestic cases) and (3) domestic unknown-SRRAs (i.e. SRRAs of unknown risks identified from domestic cases), as shown in Table 1. We classified them using the “summary of investigation results” from the revision of precautions in package inserts and the “Pharmaceuticals and Medical Devices Safety Information” on the PMDA website. “Unlabeled” ADRs in the first-version package inserts were treated as “unknown” ADRs in this study.
We applied several groups of explanatory variables in the Cox regression.
2.1 Drug Characteristics
We coded NMEs with new MOA launched first in Japan as “new MOA-first”. We coded all the drugs with new MOAs, including follow-on drugs, into “new MOA-early”. These variables may reflect accumulation of safety information concerning drugs with new MOAs.
According to the Japanese drug tariff code, which is similar to the Anatomical Therapeutic Classification System, we classified new drugs into the following eight categories: antineoplastics, antivirals, biologics, cardiovascular system, central nervous system, metabolism1 (e.g. antidiabetics), metabolism2 (e.g. anti-TNF-alpha antibody), and other drugs (Table 2).
2.2 Drug Development Background
The number of participants included in clinical trials was regarded as an index of safety evidence [8]. The numbers of domestic and foreign subjects in the clinical data package were available in common technical documents. Development plans were coded into bridging strategy, global clinical trial, and standard strategy. The Japanese launch lag was selected as a variable to describe the level of accumulation of overseas safety information. We also examined whether drugs for which Japan was the first country in which they were launched showed higher safety risks.
2.3 Foreign Information
We collected the accumulated quarterly number of alerts of FDA boxed warnings and contraindications as indices of foreign regulatory information, in case overseas alerts may have increased domestic SRRAs. It was used as a time-dependent variable.
2.4 Review and Post-Marketing Regulations
Japanese priority review has two categories: for orphan-designated diseases and for non-orphan serious diseases. These categories were treated as dummy variables.
We included a variable indicating all-case surveillance, in which drug companies are obligated to collect safety data from all patients who use the drugs. We were interested in the hypothesis that the accumulation of serious ADR case reports would increase the probability of SRRAs. We collected the quarterly accumulated number of serious ADRs reported as suspected drug from PMS/clinical studies and spontaneous reports in the JADER as time-dependent variables.
2.5 Exposure and Post-Marketing Setting
The accumulated quarterly number of patient exposures was estimated by dividing post-marketing sales by the daily per-unit drug price. The patient exposure was treated as a time-dependent variable. We used the quarterly number of approvals regarding indication expansion in Japan as an index of product life-cycle management as a time-dependent variable.
There remained trends and year effects that could not be fully explained by the variables above. We used approval year dummy variables as in previous studies [8].
Several regression models were applied to avoid possible multicollinearity problems. Model A contained a basic set of variables and was used for all three types of SRRAs. Model B was to investigate whether follow-on drugs with MOAs were risky. In Model C, we examined the hypothesis that the world’s first launch occurring in Japan would increase domestic risks. Model D was to check the impact of the patient exposure and life-cycle management. Statistical analyses were performed using STATA/IC13.
3 Results
From a total of 363 drugs approved as NMEs between 2004 and 2014, a dataset of 338 new drugs was created. Twenty-five drugs were excluded; for 13, the launch performance could not be confirmed; for 9, the sales volume could not be confirmed; for 2, the reason for approval was related to changes in the manufacturing method of the bioengineered active substance; and for 1, because two drugs were used in combination.
Table 2 displays the descriptive statistics of the NMEs and first SRRAs. During the observation period among the total of 338 NMEs, SRRAs for any reasons were issued for 119 drugs. Eighty-nine SRRAs were issued for domestic cases (i.e. domestic-SRRAs). Fifty-six SRRAs were issued for unknown ADRs (i.e. domestic unknown-SRRAs). One hundred and forty-six drugs were coded as new MOA-first and 173 drugs as new MOA-early.
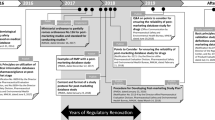
Figure 1 shows the Kaplan–Meier survival curve by approval year, indicating how first SRRAs were issued between 2004 and 2014. This confirmed the fact that the timing of first SRRAs was becoming earlier, especially for NMEs approved after 2008. SRRAs without domestic ADR cases were found in 32% of all-SRRAs (38/119) (Fig. 2). Among the SRRAs without domestic ADR cases, 9 SRRAs were for antidiabetics and 12 SRRAs were for central nervous system drugs.
Frequency of first SRRAs with and without domestic ADRs for NMEs approved between 2004 to 2014. First SRRAs without domestic ADRs indicate those for which no Japanese ADR cases were reported in the “summary of investigation results” of the revision of precautions in a package insert or “Pharmaceuticals and Medical Devices Safety Information". NMEs new molecular entities, SRRAs safety-related regulatory actions, ADRs adverse drug reactions
Table 3 shows the results of the Cox proportional hazard regression analysis. A significant positive correlation was found between drugs with new MOAs (including follow-ons) and domestic unknown-SRRAs [hazard ratio (HR) 2.76, p < 0.01]. The first drugs with new MOAs (i.e. follow-on drugs excluded) showed positive associations (HR 2.19–2.25, p < 0.05) when first Japanese launch in the world, instead of launch lag, was selected as an explanatory variable.
Positive associations were demonstrated between all-SRRAs and the following drug classes: central nervous system (HR 5.78, p < 0.001), antineoplastics (HR 4.40, p < 0.01), metabolism1 (HR 4.25, p < 0.001), and cardiovascular system (HR 3.52, p < 0.01). Interestingly, some of these classes did not show clear associations with domestic-SRRAs, but antineoplastic agents showed consistently significant associations with all the types of SRRAs.
Concerning the population size in clinical trials, the number of domestic subjects showed a positive HR only with domestic-SRRAs (HR 1.05, p < 0.01) and not with the other two types of SRRAs. Adoption of bridging strategy tended to reveal higher HRs in domestic unknown-SRRAs, but global clinical trials did not. Negative correlations were consistently observed between the launch lag and SRRAs (HR 0.87–0.92; p < 0.05). No significant association was observed with Japan being the first market into which the drug was launched.
The number of drug safety labeling changes in boxed warnings and contraindications in the USA was associated with all-SRRAs (HR 1.41, p < 0.05) and domestic-SRRAs (HR 1.60, p < 0.05), but not with domestic unknown-SRRAs.
The review period did not indicate significant correlation with SRRAs. Orphan drugs tended to show lower risks for all-SRRAs (HR 0.41, p < 0.05). Priority-review drugs for serious non-orphan diseases showed high risks for domestic unknown-SRRAs (HR 3.70, p < 0.05).
As for post-marketing regulation, no clear relationship was revealed between the all-case surveillance and SRRAs. The number of ADRs from drug companies’ PMS was not associated with SRRAs, but the number of ADRs from spontaneous reports was positively correlated with SRRAs; all-SRRAs (HR 1.04, p < 0.01), domestic-SRRAs (HR 1.07, p < 0.001), and domestic unknown-SRRAs (HR 1.03–1.05, p < 0.05).
The patient exposure was strongly associated with domestic unknown-SRRAs (HR 1.02, p < 0.001). The expansion of indication was associated positively with domestic unknown-SRRAs (HR 1.93, p < 0.01).
There was an obvious trend indicating that, other conditions being the same, overall numbers of SRRAs were on the rise, as was indicated by approval year dummies.
4 Discussion
Post-marketing safety alerts to protect patients’ health are triggered by various signals, events, and decisions at home and abroad. In this research, we aimed to show what conditions triggered official SRRAs in Japan by exploring possible associations between different types of SRRAs and various factors related to drugs, regulations, and global development backgrounds.
We first found that the time to the Japanese regulatory authority issuing a SRRA was decreasing (Fig. 1). This was also supported by the Cox regression (Table 3). This trend was observed more clearly for all-SRRAs than for domestic-SRRAs. These findings suggest that SRRAs based on external safety information on the potential risks of new drugs (e.g. class effects of similar drugs and risks identified in other countries) were more frequently implemented in recent years. This explanation is supported by the increasing number of SRRAs without domestic ADR cases in Fig. 2, which accounts for 32% of all-SRRAs. The political environment surrounding pharmaceutical safety regulation in Japan seems to play some role in this trend. In 2008, a government committee was established to discuss issues related to drug-related hepatitis scandals in Japan [13]. The committee proposed several reform plans for new drug approval and pharmacovigilance, and these historical situations might have made the regulator and drug companies more sensitive to identifying safety events of any variety.
Concerning the relationship between the innovation of new drugs and post-marketing safety, Mol et al. reported that there was no clear association between the frequency of post-marketing serious safety issues and innovative new drugs approved by the EMA between 1999 and 2011 [1]. On the other hand, Yamada et al. showed a significant association between the frequency of SRRA issues and the novelty of NMEs approved between 2000 and 2005 in Japan [8]. In our analysis, the dummy variable indicating only the first single NME in a new MOA showed positive associations with domestic unknown-SRRAs, as was expected, but did not show significant associations with all-SRRAs. The dummy variable indicating both the first and several follow-on drugs in the same MOA, showed a significant positive association in the same model. It has been reported that clinically significant ADRs are added to package inserts at higher frequencies between two and three years after the launch of NMEs in Japan [9]. All these suggest that decisions on SRRAs are likely to be prompted by a group of drugs with the same MOA, as class effects are identified. Information related to ADRs is commonly shared by drugs with the same MOA in the summary of product characteristics [14]. Together with the finding that launch lags seem to decrease SRRA risks, our results suggest that managing the risk of novel new drugs on new markets is a vital issue.
A previous study showed that the frequency of SRRAs for NMEs approved in Japan during 2000–2005 was not clearly associated with the number of subjects in clinical trials or the length of the approval review period; however, it was negatively associated with launch lag [8,9,10]. Similar results were obtained in our study. Our data indicate that a one-year increase in launch lag yields an approximately 10% reduction in the risk of issuing SRRAs. Interestingly, the number of domestic clinical trial participants was positively correlated with domestic-SRRAs and not with domestic unknown-SRRAs. If drugs are tested exhaustively in a domestic population, then rarer adverse events are more likely to be picked up during clinical trials, e.g. the ADR becomes ‘known’, and likelihood of ‘unknown’ ADRs remaining undiscovered by the time of approval decreases, which could shift the balance towards domestic-SRRA risks versus domestic unknown-SRRA risks.
Foreign information seems to have substantial impact on domestic-SRRAs, other conditions being the same. The frequency of drug safety labeling changes in the USA had a positive association with SRRAs. In addition to these direct exchanges of post-marketing safety information, drug safety is influenced by global drug development pathways. Simultaneous global development and the use of bridging strategies reduce delay to launch in global markets. However, this may reduce the safety information available in local patient populations upon approval. Tradeoffs between them are a controversial public health issue.
Our results suggested that new drugs developed under bridging strategies, which allow data to be extrapolated from foreign clinical trials to Japanese populations, tend to have a higher risk of first SRRAs related to unknown ADRs than those developed under a traditional development strategy, with local pivotal trials. Although this was in line with a previous report [8], it is difficult to ascribe this to specific causes, because many confounders exist in and around the observed association. One possibility would be that dose setting for Japanese patients under a bridging strategy might be related to an increased safety risk [15]. It is interesting to note that drugs with global clinical trials in their data packages did not show an increased risk of SRRAs compared with drugs having a traditional domestic package. The number of drugs approved based on large global trials has drastically increased since 2010, and further studies are needed to clarify the impact of this trend.
Antineoplastics and drugs designated for the priority review of non-orphan diseases showed a tendency toward higher risks of domestic unknown-SRRAs. Studies reported no association between rare diseases and post-marketing safety risk [1, 8], but a recent study focusing on drug-related death reported somewhat higher risks for orphan drugs [15].
There are several mandatory pharmacovigilance mechanisms, some of which are unique to Japan. All-case surveillance, which is part of PMS activities, is sometimes imposed on drug companies as an approval condition when the drug exerts potentially higher risks and the number of Japanese subjects in clinical data package is too small to assess safety profiles [16]. There was no clear correlation between SRRAs and all-case surveillance, however. This was somewhat counter-intuitive, but was consistent with a previous report [8]. There are at least two possible explanations for this. One might be a signaling effect of all-case surveillance. When physicians use a drug with all-case surveillance, they use it more cautiously and appropriately because they are obliged to report every case, which inevitably decreases the occurrence of ADRs [8, 17, 18]. Another possibility is a statistical implication related to multicollinearity. In our regression analysis, several variables used in each model are obviously associated with the variable “all-case surveillance.” Such variables include drug class, clinical trial population size, and orphan status. Relationships between these variables are so complicated that it would be difficult to isolate only the effect of all-case surveillance, if it actually exists.
Our analysis demonstrated that domestic unknown-SRRAs had positive associations with the number of ADRs from spontaneous reports, but not with that of ADRs from drug companies’ PMS. It has been reported that PMS does not necessarily result in identifying unknown risks [19], partly because PMS activities of drug companies commonly cover a limited number of medical institutions. Our observation suggests that collecting spontaneous reports of ADRs from a variety of medical institutions through monitoring activities has still been a cornerstone of PMS to minimize unknown risks.
A greater number of patient exposures and indication expansion could result in a higher risk of the first SRRA issue. Both facts seem to imply the SRRA risks would increase with diversification of patient populations for new drugs and thus demonstrate the importance of implementing risk management throughout the product life cycle.
There are limitations in this research. Although this research identified a number of associations between safety alerts and various factors, most of the associations are “ecological” in a real-world setting. We are not able to intervene or set many of the factors independently and/or prospectively. The purpose of this study was to explore possible mechanisms behind SRRAs, which would serve prediction, rather than intervention, in post-marketing surveillance. It should also be emphasized that what we have found are associations and not causalities per se. Our regression models do not reveal causal pathways, nor possible interactions between players in the decisions of SRRAs. SRRAs in a country reflect both safety risks in its patient population and societal sensitivity to such risks, but our study did not delve into this complicated interaction.
Notwithstanding these limitations, the observed associations may be used to inform the implementation of effective and efficient risk management for drug safety on a daily basis, or utilized in critical safety problems in the future.
5 Conclusions
We found several interesting associations among the three types of first SRRAs and drug characteristics, drug development background, regulation, and post-marketing setting. New MOA, serious diseases such as cancer, FDA safety label changes, and the number of domestic study participants, and indication expansion showed a positive association with SRRAs, and launch lag showed a negative association with SRRAs. The comparison of the three types of SRRAs showed that external and domestic information have somewhat different impact on domestic SRRAs. Among the three SRRAs, SRRAs caused by domestic unknown ADRs seem to be the most sensitive indicator that reflects potential insufficiency of safety information in local populations.
Our results indicated that global clinical development pathways and marketing status should be considered more seriously in implementing locally optimized pharmacovigilance activities. Caution may be needed not only for drugs with novel MOAs, but also for drugs for which local dose-finding studies have been skipped, expedited review status has been given, timing of launch is close to those in the USA and the EU, and spontaneous reports rather than company-lead surveillance suggest possible safety risks. These provide a list of practical considerations when drug companies establish risk-management plans and regulatory agencies revise current pharmacovigilance guidelines.
References
Mol PG, Arnardottir AH, Motola D, et al. Post-approval safety issues with innovative drug: a European cohort study. Drug Saf. 2013;36:1105–15.
Schultz WB. Bolstering the FDA’s drug-safety authority. NEJM. 2007;357(22):2217–9.
FDA. Breakthrough therapy designation. http://www.fda.gov/forpatients/approvals/fast/ucm405397.htm. Accessed 1 May 2017.
EMA. PRIME: priority medicines. http://www.ema.europa.eu/ema/index.jsp?curl=pages/regulation/general/general_content_000660.jsp&mid=WC0b01ac05809f8439. Accessed 1 May 2017.
MHLW. Strategy of SAKIGAKE. http://www.mhlw.go.jp/english/policy/health-medical/pharmaceuticals/140729-01.html. Accessed 1 May 2017.
JPMA, Chapter 4 post-marketing surveillance of drugs. In: Pharmaceutical Administration and Regulations in Japan, Japan Pharmaceutical Manufacturers Association; 2017. http://www.jpma.or.jp/english/parj/pdf/2017.pdf. Accessed 14 June 2017.
Tomita T, Ono Y, Nejihashi K, Taogoshi T, Matsuo H. Description of important potential risks of Japanese risk management plan on each package insert. Iyakuhin Johogaku. 2016;18(3):214–7 (in Japanese).
Yamada T, Kusama M, Hirai Y, Arnold F, Sugiyama Y, Ono S. Analysis of pharmaceutical safety-related regulatory actions in Japan: do tradeoffs exist between safer drugs and launch delay? Ann Pharmacother. 2010;44:1976–85.
Ogami T, Imaizumi T, Ishiguro C, Matsuda T. Assessment of postmarketing safety-related regulatory actions in Japan. Pharm Med. 2012;26(6):395–403.
Olson MK. The risk we bear: The effects of review speed and industry user fees on new drug safety. J Health Econ. 2008;27(2):175–200.
Carpenter D, Zucker EJ, Avorn J. Drug-review deadlines and safety problems. N Engl J Med. 2008;358:1354–61.
Jayaputra K, Ono S. Differences between the United States and Japan in labels of oncological drugs. Pharmacoepidemiol Drug Saf. 2017;26(2):143–51.
MHLW. Review on the Pharmaceutical Administration to Prevent Recurrence of Yakugai (Drug-induced suffering) (final proposal). Committee for Investigation of Drug-induced Hepatitis Cases and Appropriate Regulatory Administration to Prevent Recurrence of Yakugai Similar Sufferings; 2010. http://www.mhlw.go.jp/shingi/2010/04/s0428-8.html. Accessed 1 May 2017 (in Japanese).
Stefansdottir G, Knol MJ, Arnardottir AH, et al. Safety learning from drugs of the same class: room for improvement. Clin Pharmacol Ther. 2012;91(5):872–80.
Okubo TK, Ono S. Exploratory analysis of associations between postmarketing safety events and approved doses of new drugs in Japan. Clin Transl Sci. 2017. doi:10.1111/cts.12462.
MHLW. Re: Q&A on use-results surveys conducted as all-case surveillance and early post-marketing phase vigilance (EPPV) for prescription drugs. Tokyo: MHLW/PFSB/Safety Division; 2009. https://www.pmda.go.jp/files/000153521.pdf. Accessed 1 May 2017.
Narukawa M. Research on the situation and implications of the post-marketing all-case surveillance study in Japan—considerations based on a questionnaire survey (in Japanese). RSMP. 2014;4(3):199–206.
Yamada T, Watanabe Y, Kusama M, Sugiyama Y, Ono S. Factors associated with spontaneous reporting of adverse drug reactions in Japan. Pharmacoepidemiol Drug Saf. 2013;22:468–76.
Narukawa M. Research on the situation and implications of the post-marketing surveillance study in Japan—considerations based on a questionnaire survey (in Japanese). RSMP. 2014;4(1):11–9.
Acknowledgements
Makoto Fujikawa, an employee of Daiichi Sankyo Co. Ltd, was affiliated with the JPMA, but the views expressed in this article do not necessarily reflect the official views of JPMA.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
Shunsuke Ono received a research grant from the JPMA for the conduct and publication of this study.
Conflict of interest
Makoto Fujikawa has been an Employee of Daiichi Sankyo Co. Ltd since 2007. Shunsuke Ono declares no conflict of interest.
Ethical approval
Ethical approval was not required for this study.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution-NonCommercial 4.0 International License (http://creativecommons.org/licenses/by-nc/4.0/), which permits any noncommercial use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
About this article
Cite this article
Fujikawa, M., Ono, S. Analysis of Safety-Related Regulatory Actions for New Drugs in Japan by Nature of Identified Risks. Pharm Med 31, 317–327 (2017). https://doi.org/10.1007/s40290-017-0198-2
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40290-017-0198-2