Abstract
Background and Objectives
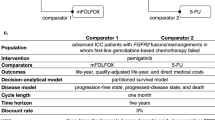
The National Comprehensive Cancer Network recommends a second-line treatment of pemigatinib for patients with intrahepatic cholangiocarcinoma with fibroblast growth factor receptor 2 (FGFR2) fusions/rearrangements and modified FOLFOX (mFOLFOX) for those without FGFR2 alterations. However, these regimens are not yet covered by Taiwa’s National Health Insurance. This cost-effectiveness analysis evaluated the cost-effectiveness of the pemigatinib/mFOLFOX regimen as the second-line treatment for advanced intrahepatic cholangiocarcinoma based on FGFR2 status in comparison with the regimen of fluorouracil chemotherapy and provided a cost-effectiveness analysis-based reference price for pemigatinib.
Methods
A three-state partitioned survival model with a 5-year time horizon was constructed for patients with advanced intrahepatic cholangiocarcinoma who did not respond to first-line therapy. Overall and progression-free survival functions of pemigatinib, mFOLFOX, and fluorouracil were estimated from the FIGHT-202, ABC-06, and NIFTY trials, respectively. The utility of health states and disutility of adverse events were obtained from the literature. The genetic testing fee and price of pemigatinib were set as the market price. Other costs related to advanced intrahepatic cholangiocarcinoma were calculated using National Health Insurance claims data. The willingness-to-pay threshold was three times the gross domestic product per capita in 2021 (NT$2,889,684). A 3% discount rate was applied to quality-adjusted life-years and costs. Scenario analyses included a gradual price reduction of pemigatinib, alternative survival models, application of a National Health Insurance payment conversion factor to non-medication costs, and consideration of life-years as effectiveness. A deterministic sensitivity analysis, probabilistic sensitivity analysis, and a value of information analysis were performed.
Results
The new regimen provided an incremental 0.13 quality-adjusted life-years, with incremental costs of NT$459,697, yielding an incremental cost-effectiveness ratio of NT$3,411,098 per quality-adjusted life-year and an incremental net monetary benefit of − NT$70,268. The new regimen was found to be 53.2% cost effective in the probabilistic sensitivity analysis. The expected value of uncertainty measured by the expected value of perfect information was NT$80,695/person. In scenario analyses, the incremental net monetary benefit was positive when the price of pemigatinib was reduced by 40% or more. When applying a conversion factor to non-medical costs, the probability of the new regimen being cost effective was slightly increased from 53.2 to 56.5% compared with the base-case analysis. The utility and the cost of the new regimen were the main drivers of uncertainty.
Conclusions
Although the new second-line genetic-based and biomarker-driven regimen of pemigatinib/mFOLFOX appears not cost effective for patients with advanced intrahepatic cholangiocarcinoma in the base-case analysis, our analysis suggests it is highly likely to be cost effective in the case of a 40% price reduction on pemigatinib.





Similar content being viewed by others
References
Banales JM, Marin JJG, Lamarca A, Rodrigues PM, Khan SA, Roberts LR, et al. Cholangiocarcinoma 2020: the next horizon in mechanisms and management. Nat Rev Gastroenterol Hepatol. 2020;17(9):557–88.
Cardinale V, Bragazzi MC, Carpino G, Matteo SD, Overi D, Nevi L, et al. Intrahepatic cholangiocarcinoma: review and update. Hepatoma Res. 2018;4:20.
Health Promotion Administration, Ministry of Health and Welfare, Taiwan. Cancer Registry Annual Report, 2019. Taipei: Health Promotion Administration, Ministry of Health and Welfare, Taiwan; 2021.
Farshidfar F, Zheng S, Gingras M-C, Newton Y, Shih J, Robertson AG, et al. Integrative genomic analysis of cholangiocarcinoma identifies distinct IDH-mutant molecular profiles. Cell Rep. 2017;18(11):2780–94.
Cao J, Hu J, Liu S, Meric-Bernstam F, Abdel-Wahab R, Xu J, et al. Intrahepatic cholangiocarcinoma: genomic heterogeneity between Eastern and Western patients. JCO Precis Oncol. 2020;4:557–69.
Lamarca A, Barriuso J, McNamara MG, Valle JW. Molecular targeted therapies: ready for “prime time” in biliary tract cancer. J Hepatol. 2020;73(1):170–85.
Abou-Alfa GK, Sahai V, Hollebecque A, Vaccaro G, Melisi D, Al-Rajabi R, et al. Pemigatinib for previously treated, locally advanced or metastatic cholangiocarcinoma: a multicentre, open-label, phase 2 study. Lancet Oncol. 2020;21(5):671–84.
Valle J, Wasan H, Palmer DH, Cunningham D, Anthoney A, Maraveyas A, et al. Cisplatin plus gemcitabine versus gemcitabine for biliary tract cancer. N Engl J Med. 2010;362(14):1273–81.
Lamarca A, Palmer DH, Wasan HS, Ross PJ, Ma YT, Arora A, et al. Second-line FOLFOX chemotherapy versus active symptom control for advanced biliary tract cancer (ABC-06): a phase 3, open-label, randomised, controlled trial. Lancet Oncol. 2021;22(5):690–701.
Yoo C, Kim K-P, Jeong JH, Kim I, Kang MJ, Cheon J, et al. Liposomal irinotecan plus fluorouracil and leucovorin versus fluorouracil and leucovorin for metastatic biliary tract cancer after progression on gemcitabine plus cisplatin (NIFTY): a multicentre, open-label, randomised, phase 2b study. Lancet Oncol. 2021;22(11):1560–72.
Rizzo A, Ricci AD, Brandi G. Pemigatinib: Hot topics behind the first approval of a targeted therapy in cholangiocarcinoma. Cancer Treat Res Commun. 2021;27: 100337.
National Institute for Health and Care Excellence (NICE). Pemigatinib for treating relapsed or refractory advanced cholangiocarcinoma with FGFR2 fusion or rearrangement [Technology appraisal guidance TA722]. London: NICE; 2021.
Reimbursement Team. Pemigatinib (Pemazyre). Can J Health Technol. 2022;2:4.
Husereau D, Drummond M, Augustovski F, de Bekker-Grob E, Briggs AH, Carswell C, et al. Consolidated Health Economic Evaluation Reporting Standards 2022 (CHEERS 2022) statement: updated reporting guidance for health economic evaluations. Pharmacoeconomics. 2022;40(6):601–9.
Husereau D, Drummond M, Augustovski F, de Bekker-Grob E, Briggs AH, Carswell C, et al. Consolidated Health Economic Evaluation Reporting Standards (CHEERS) 2022 explanation and elaboration: a report of the ISPOR CHEERS II Good Practices Task Force. Value Health. 2022;25(1):10–31.
Woods BS, Sideris E, Palmer S, Latimer N, Soares M. Partitioned survival and state transition models for healthcare decision making in oncology: where are we now? Value Health. 2020;23(12):1613–21.
Pahuta MA, Werier J, Wai EK, Patchell RA, Coyle D. A technique for approximating transition rates from published survival analyses. Cost Eff Resour Alloc. 2019;17(1):12.
Rohatgi A. WebPlotDigitizer. 2021. https://automeris.io/WebPlotDigitizer/. Accessed 30 Jun 2022.
Guyot P, Ades AE, Ouwens MJ, Welton NJ. Enhanced secondary analysis of survival data: reconstructing the data from published Kaplan-Meier survival curves. BMC Med Res Methodol. 2012;1(12):9.
Mohammed S. Introduction to survival analysis using R. Workshop on Computational Biostatistics and Survival Analysis. 2022. https://shariq-mohammed.github.io/files/cbsa2019/1-intro-to-survival.html. Accessed 3 Jul 2022.
Sestelo M. 3.6 How to evaluate the PH assumption? A short course on survival analysis applied to the financial industry. In: Madrid: BBVA Data & Analytics; 2017.
Su D, Wu B, Shi L. Cost-effectiveness of atezolizumab plus bevacizumab vs sorafenib as first-line treatment of unresectable hepatocellular carcinoma. JAMA Netw Open. 2021;4(2): e210037.
National Institute for Health and Care Excellence (NICE). Sorafenib for treating advanced hepatocellular carcinoma [technology appraisal guidance TA474]. London: NICE; 2017.
Chiang N-J, Tan KT, Zhuo D-W, Chen M-H, Chen S-J, Chiu T-J, et al. Comprehensive genomic profiling of 157 Taiwanese intrahepatic cholangiocarcinoma and its correlation with survival [poster presentation]. In: The 25th Taiwan Joint Cancer Conference; 4-5 September, 2021; Taipei.
Amdahl J, Diaz J, Park J, Nakhaipour HR, Delea TE. Cost-effectiveness of pazopanib compared with sunitinib in metastatic renal cell carcinoma in Canada. Curr Oncol. 2016;23(4):340–54.
National Institute for Health and Care Excellence (NICE). Pomalidomide for multiple myeloma previously treated with lenalidomide and bortezomib [technology appraisal guidance TA427]. London: NICE; 2017.
ACT Genomics. ACTFusion™. 2022. https://www.actgenomics.com/professional_product.php?id=3. Accessed 20 Oct 2022.
Robinson LA, Hammitt JK, Chang AY, Resch S. Understanding and improving the one and three times GDP per capita cost-effectiveness thresholds. Health Policy Plan. 2017;32(1):141–5.
World Health Organization. Office of World Health R. The world health report: 2002: reducing risks, promoting healthy life: overview. Geneva: World Health Organization; 2002.
Vemer P, Corro Ramos I, Van Voorn GAK, Al MJ, Feenstra TL. AdViSHE: a validation-assessment tool of health-economic models for decision makers and model users. Pharmacoeconomics. 2016;34(4):349–61.
National Institute for Health and Care Excellence (NICE). Pemigatinib for treating relapsed or refractory advanced cholangiocarcinoma with FGFR2 alterations [ID3730]. Committee papers. London: NICE; 2021.
Cranmer H, Shields GE, Bullement A. A comparison of partitioned survival analysis and state transition multi-state modelling approaches using a case study in oncology. J Med Econ. 2020;23(10):1176–85.
Center for Drug Evaluation, Taiwan (CDE). Methodology guide for health technology assessment. Taipei: CDE; 2013.
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Funding
This study received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Conflicts of Interest/Competing Interests
Nai-Jung Chiang has received payment for lectures from Eli Lilly and Company, TTY Biopharm Company Limited, Ono Pharmaceutical Co., Ltd., Bristol Myers Squibb, PharmaEngine, Inc., and Roche. Chen-Han Chueh, Zi-Rong Chen, Ming-Neng Shiu, Yu-Wen Wen, and Yi-Wen Tsai have no conflicts of interest that are directly relevant to the content of this article.
Ethics Approval
The Institutional Review Board of National Yang Ming Chiao Tung University, Taiwan approved this study (YM111012E).
Availability of Data and Material
The data that support the findings of this study are available from the Ministry of Health and Welfare, Taiwan, but restrictions apply to the availability of these data, which were used under license for the current study and are not publicly available.
Consent to Participate
The Institutional Review Board of National Yang Ming Chiao Tung University (IRB) agreed to waive the consent to participate for this research because this research is low risk. Furthermore, the possible risk to the research subjects is no more than that of those who did not participate in the research, and the exemption from obtaining prior consent does not affect the rights and interests of the research subjects.
Consent to Publish
Consent to publish is not required because the IRB agreed that this research did not require consent to participate.
Code Availability
The code supporting the findings of this study is available from the corresponding authors upon request.
Authors’ Contributions
Conceptualization: Y-WW, Y-WT, N-JC; data curation: Z-RC; formal analysis: C-HC, Z-RC; methodology: M-NS, Y-WW, Y-WT; project administration: M-NS, Y-WT, N-JC; resources: Y-WT; software: C-HC, Z-RC; supervision: M-NS, Y-WW, Y-WT, N-JC; validation: C-HC; visualization: C-HC, Z-RC; writing, original draft: C-HC, Z-RC, Y-WT; writing, review and editing: C-HC, M-NS, Y-WW, Y-WT, N-JC. All authors read and approved the final manuscript.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Chueh, CH., Tsai, YW., Chen, ZR. et al. Cost-Effectiveness Analysis of a New Second-Line Treatment Regimen for Advanced Intrahepatic Cholangiocarcinoma: Biomarker-Driven Targeted Therapy of Pemigatinib Versus 5-FU Chemotherapy. PharmacoEconomics 41, 307–319 (2023). https://doi.org/10.1007/s40273-022-01227-6
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40273-022-01227-6