Abstract
Objective
The aim of this study was to review analytical methods that enable the incorporation of equity concerns within economic evaluation.
Methods
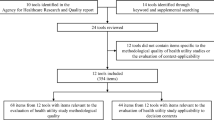
A systematic search of PubMed, Embase, and EconLit was undertaken from database inception to February 2021. The search was designed to identify methodological approaches currently employed to evaluate health-related equity impacts in economic evaluation studies of healthcare interventions. Studies were eligible if they described or elaborated on a formal quantitative method used to integrate equity concerns within economic evaluation studies. Cost-utility, cost-effectiveness, cost-benefit, cost-minimisation, and cost-consequence analyses, as well as health technology appraisals, budget impact analyses, and any relevant literature reviews were included. For each of the identified methods, we provided summaries of the scope of equity considerations covered, the methods employed and their key attributes, data requirements, outcomes, and strengths and weaknesses. A traffic light assessment of the practical suitability of each method was undertaken, alongside a worked example applying the different methods to evaluate the same decision problem. Finally, the review summarises the typical trade-offs arising in cost-effectiveness analyses and discusses the extent to which the evaluation methods are able to capture these.
Results
In total, 68 studies were included in the review. Methods could broadly be grouped into equity-based weighting (EBW) methods, extended cost-effectiveness analysis (ECEA), distributional cost-effectiveness analysis (DCEA), multi-criteria decision analysis (MCDA), and mathematical programming (MP). EBW and MP methods enable equity consideration through adjustment to incremental cost-effectiveness ratios, whereas equity considerations are represented through financial risk protection (FRP) outcomes in ECEA, social welfare functions (SWFs) in DCEA, and scoring/ranking systems in MCDA. The review identified potential concerns for EBW methods and MCDA with respect to data availability and for EBW methods and MP with respect to explicitly measuring changes in inequality. The only potential concern for ECEA related to the use of FRP metrics, which may not be relevant for all healthcare systems. In contrast, DCEA presented no significant concerns but relies on the use of SWFs, which may be unfamiliar to some audiences and requires societal preference elicitation. Consideration of typical cost-effectiveness and equity-related trade-offs highlighted the flexibility of most methods with respect to their ability to capture such trade-offs. Notable exceptions were trade-offs between quality of life and length of life, for which we found DCEA and ECEA unsuitable, and the assessment of lost opportunity costs, for which we found only DCEA and MP to be suitable. The worked example demonstrated that each method is designed with fundamentally different analytical objectives in mind.
Conclusions
The review emphasises that some approaches are better suited to particular decision problems than others, that methods are subject to different practical requirements, and that significantly different conclusions can be observed depending on the choice of method and the assumptions made. Further, to fully operationalise these frameworks, there remains a need to develop consensus over the motivation for equity assessment, which should necessarily be informed with stakeholder involvement. Future research of this topic should be a priority, particularly within the context of equity evaluation in healthcare policy decisions.


Similar content being viewed by others
Notes
Typically, unemployed citizens or those in poverty cannot pay and so receive limited healthcare coverage; exceptions exist where governments opt to fund healthcare for those in impoverished circumstances.
Some studies described multiple methods, so the reported totals sum to more than the number of studies; systematic literature reviews were not included in these totals.
References
The World Health Organisation. Equity. https://www.who.int/healthsystems/topics/equity/en/. Published 2020. Accessed Nov 2020.
The World Health Organisation. Social determinants of health. https://www.who.int/health-topics/social-determinants-of-health#tab=tab_1. Published 2020. Accessed Nov 2020.
Mackenbach JP, Valverde JR, Bopp M, et al. Determinants of inequalities in life expectancy: an international comparative study of eight risk factors. Lancet Public Health. 2019;4(10):e529–37.
National Academies of Sciences, Engineering and Medicine; Health and Medicine Division; Board on Population Health and Public Health Practice; Committee on Community-Based Solutions to Promote Health Equity in the United States. The root causes of health inequity. In: Baciu A, Negussie Y, Geller A, ed. Communities in action: pathways to health equity. 2017.
Mackenbach JP, Kulhánová I, Artnik B, et al. Changes in mortality inequalities over two decades: register based study of European countries. BMJ. 2016;353:1732.
Essink-Bot M-L, Dekker E. Equal access to colorectal cancer screening. Lancet. 2016;387(10020):724–6.
Or Z, Cases C, Lisac M, Vrangbaek K, Winblad U, Bevan G. Are health problems systemic? Politics of access and choice under Beveridge and Bismarck systems. Health Econ Policy Law. 2010;5(3):269–93.
Ministry of Health, Consumption and Social Welfare, Spain. Health care systems in the European Union countries: Health characteristics and indicators 2019. 2019. https://www.mscbs.gob.es/estadEstudios/estadisticas/docs/presentacion_en.pdf. Accessed Jan 2021.
The National Institute for Health and Care Excellence. NICE technology appraisal guidance. https://www.nice.org.uk/about/what-we-do/our-programmes/nice-guidance/nice-technology-appraisal-guidance. Published 2020. Accessed Nov 2020.
Ward T, Medina-Lara A, Mujica-Mota RE, Spencer AE. Accounting for heterogeneity in resource allocation decisions: methods and practice in UK cancer technology appraisals. Value in Health (in press). 2021.
Sassi F, Archard L, Le Grand J. Equity and the economic evaluation of healthcare. Health Technol Assess. 2001;5(3):1–138.
Johri M, Norheim OF. Can cost-effectiveness analysis integrate concerns for equity? Systematic review. Int J Technol Assess Health Care. 2012;28(2):125–32.
Lal A, Moodie M, Peeters A, Carter R. Inclusion of equity in economic analyses of public health policies: systematic review and future directions. Aust N Z J Public Health. 2018;42(2):207–13.
Dukhanin V, Searle A, Zwerling A, Dowdy DW, Taylor HA, Merritt MW. Integrating social justice concerns into economic evaluation for healthcare and public health: a systematic review. Soc Sci Med. 2018;198:27–35.
Avanceña ALV, Prosser LA. Examining equity effects of health interventions in cost-effectiveness analysis: a systematic review. Value Health. 2021;24(1):136–43.
Moher D, Liberati A, Tetzlaff J, Altman DG. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. BMJ. 2009;339:2535.
Ward T M-LA, Mujica-Mota RE, Spencer AE. The incorporation of equity considerations in cost-effectiveness analyses: a systematic literature review. PROSPERO 2020 CRD42020180904 2020. https://www.crd.york.ac.uk/PROSPERO/display_record.php?RecordID=180904. Published July 2020.
Williams A. Intergenerational equity: an exploration of the ‘Fair Innings’ argument. Health Econ. 1997;6(2):117–32.
Atkinson AB. On the measurement of inequality. J Econ Theory. 1970;2(3):244–63.
Kolm S-C. Unequal inequalities I. J Econ Theory. 1976;12(3):416–42.
Regidor E. Measures of health inequalities: part 2. J Epidemiol Community Health. 2004;58(11):900–3.
Gini CW. Variability and mutability, contribution to the study of statistical distributions and relations. studi cconomico-giuridici della r. universita de cagliari (1912). Reviewed in: Light RJ, Margolin BH. An analysis of variance for categorical data. J Am Stat Assoc. 1971;66:534–544.
The National Institute for Health and Care Excellence. Improving health and social care through evidence-based guidance. https://www.nice.org.uk/. Published 2020. Accessed Nov 2020.
Paulden M. Recent amendments to NICE’s value-based assessment of health technologies: implicitly inequitable? Expert Rev Pharmacoecon Outcomes Res. 2017;17(3):239–42.
OECD. Health inequalities. https://www.oecd.org/health/inequalities-in-health.htm. Published 2020. Accessed Dec 2020, 2020.
The Kings Fund. What are health inequalities? https://www.kingsfund.org.uk/publications/what-are-health-inequalities?gclid=EAIaIQobChMI3Zbo0rux6gIVDNiyCh3_gQklEAAYASAAEgI7ffD_BwE. Published 2020. Accessed Nov 2020.
Exworthy M, Blane D, Marmot M. Tackling health inequalities in the United Kingdom: the progress and pitfalls of policy. Health Serv Res. 2003;38(6 Pt 2):1905–21.
National Institute for Health and Care Excellence. Glossary. Health inequalities. https://www.nice.org.uk/glossary?letter=h. Published 2020. Accessed Dec 2020, 2020.
Daems R, Maes E, Glaetzer C. Equity in pharmaceutical pricing and reimbursement: crossing the income divide in Asia Pacific. Value Health Region Issues. 2013;2(1):160–6.
Versteegh MM, Ramos IC, Buyukkaramikli NC, Ansaripour A, Reckers-Droog VT, Brouwer WBF. Severity-adjusted probability of being cost effective. Pharmacoeconomics. 2019;37(9):1155–63.
Haaland OA, Lindemark F, Johansson KA. A flexible formula for incorporating distributive concerns into cost-effectiveness analyses: priority weights. PLoS ONE. 2019;14(10):e0223866.
Bleichrodt H. Health utility indices and equity considerations. J Health Econ. 1997;16(1):65–91.
Bleichrodt H, Diecidue E, Quiggin J. Equity weights in the allocation of health care: the rank-dependent QALY Model. J Health Econ. 2004;23(1):157–71.
Cookson R, Drummond M, Weatherly H. Explicit incorporation of equity considerations into economic evaluation of public health interventions. Health Econ Policy Law. 2009;4(2):231–45.
Cookson R, Mirelman AJ, Griffin S, et al. Using cost-effectiveness analysis to address health equity concerns. Value Health. 2017;20(2):206–12.
Dolan P. The measurement of individual utility and social welfare. J Health Econ. 1998;17(1):39–52.
Gafni A, Birch S. Equity considerations in utility-based measures of health outcomes in economic appraisals: an adjustment algorithm. J Health Econ. 1991;10(3):329–42.
Nord E, Pinto JL, Richardson J, Menzel P, Ubel P. Incorporating societal concerns for fairness in numerical valuations of health programmes. Health Econ. 1999;8(1):25–39.
Nord E. Towards cost-value analysis in health care? Health Care Anal. 1999;7(2):167–75.
Nord E. Concerns for the worse off: fair innings versus severity. Soc Sci Med. 2005;60(2):257–63.
Rodríguez E, Pinto-Prades J-L. The social value of health programmes: is age a relevant factor? Health Econ. 2000;9(7):611–21.
Round J, Paulden M. Incorporating equity in economic evaluations: a multi-attribute equity state approach. Eur J Health Econ. 2018;19(4):489–98.
Sussex J, Towse A, Devlin N. Operationalizing value-based pricing of medicines: a taxonomy of approaches. Pharmacoeconomics. 2013;31(1):1–10.
Tsuchiya A. Age-related preferences and age weighting health benefits. Soc Sci Med. 1999;48(2):267–76.
Ubel PA, Nord E, Gold M, Menzel P, Prades JL, Richardson J. Improving value measurement in cost-effectiveness analysis. Med Care. 2000;38(9):892–901.
Lindemark F, Haaland ØA, Kvåle R, Flaatten H, Norheim OF, Johansson KA. Costs and expected gain in lifetime health from intensive care versus general ward care of 30,712 individual patients: a distribution-weighted cost-effectiveness analysis. Crit Care. 2017;21(1):220.
Ong KS, Kelaher M, Anderson I, Carter R. A cost-based equity weight for use in the economic evaluation of primary health care interventions: case study of the Australian Indigenous population. Int J Equity Health. 2009;8:34.
Karnon J, Partington A. Cost-value analysis and the SAVE: a work in progress, but an option for localised decision making? Pharmacoeconomics. 2015;33(12):1281–8.
Carr VJ, Lewin TJ, Neil AL. What is the value of treating schizophrenia? Aust N Z J Psychiatry. 2006;40(11–12):963–71.
Baeten SA, Baltussen RMPM, Uyl-De Groot CA, Bridges J, Niessen LW. Incorporating equity-efficiency interactions in cost-effectiveness analysis—three approaches applied to breast cancer control. Value Health. 2010;13(5):573–9.
Bleichrodt H, Doctor J, Stolk E. A nonparametric elicitation of the equity-efficiency trade-off in cost-utility analysis. J Health Econ. 2005;24(4):655–78.
Stolk EA, van Donselaar G, Brouwer WB, Busschbach JJ. Reconciliation of economic concerns and health policy: illustration of an equity adjustment procedure using proportional shortfall. Pharmacoeconomics. 2004;22(17):1097–107.
Luyten J, van Hoek AJ. Integrating alternative social value judgments into cost-effectiveness analysis of vaccines: an application to varicella-zoster virus vaccination. Value Health. 2021;24(1):41–9.
Love-Koh J, Cookson R, Gutacker N, Patton T, Griffin S. Aggregate distributional cost-effectiveness analysis of health technologies. Value Health. 2019;22(5):518–26.
Love-Koh J, Pennington B, Owen L, Taylor M, Griffin S. How health inequalities accumulate and combine to affect treatment value: A distributional cost-effectiveness analysis of smoking cessation interventions. Soc Sci Med. 2020;265:113339.
Griffin S, Love-Koh J, Pennington B, Owen L. Evaluation of intervention impact on health inequality for resource allocation. Med Decis Mak Int J Soc Med Decis Mak. 2019;39(3):171–82.
Allen K, Pearson-Stuttard J, Hooton W, Diggle P, Capewell S, O’Flaherty M. Potential of trans fats policies to reduce socioeconomic inequalities in mortality from coronary heart disease in England: cost effectiveness modelling study. BMJ. 2015;351:h4583.
Kypridemos C, Collins B, McHale P, et al. Future cost-effectiveness and equity of the NHS Health Check cardiovascular disease prevention programme: microsimulation modelling using data from Liverpool, UK. PLoS Med. 2018;15(5):e1002573.
Asaria M, Griffin S, Cookson R, Whyte S, Tappenden P. Distributional cost-effectiveness analysis of health care programmes—a methodological case study of the UK bowel cancer screening programme. Health Econ (UK). 2015;24(6):742–54.
Asaria M, Griffin S, Cookson R. Distributional cost-effectiveness analysis: a tutorial. Med Decis Mak Int J Soc Med Decis Mak. 2016;36(1):8–19.
Collins B, Kypridemos C, Cookson R, et al. Universal or targeted cardiovascular screening? Modelling study using a sector-specific distributional cost effectiveness analysis. Prev Med. 2020;130:105879.
Olsen M, Norheim OF, Memirie ST. Reducing regional health inequality: a sub-national distributional cost-effectiveness analysis of community-based treatment of childhood pneumonia in Ethiopia. Int J Equity Health. 2021;20(1):9.
Dawkins BR, Mirelman AJ, Asaria M, Johansson KA, Cookson RA. Distributional cost-effectiveness analysis in low- and middle-income countries: illustrative example of rotavirus vaccination in Ethiopia. Health Policy Plan. 2018;33(3):456–63.
Ngalesoni FN, Ruhago GM, Mori AT, Robberstad B, Norheim OF. Equity impact analysis of medical approaches to cardiovascular diseases prevention in Tanzania. Soc Sci Med. 2016;170:208–17.
Robberstad B, Norheim OF. Incorporating concerns for equal lifetime health in evaluations of public health programs. Soc Sci Med. 2011;72(10):1711–6.
Lee TH, Kim W, Shin J, Park EC, Park S, Kim TH. Strategic distributional cost-effectiveness analysis for improving national cancer screening uptake in cervical cancer: a focus on regional inequality in South Korea. Cancer Res Treat. 2018;50(1):212–21.
Lee KS, Park EC. Cost effectiveness of colorectal cancer screening interventions with their effects on health disparity being considered. Cancer Res Treat. 2016;48(3):1010–9.
Oosterhoff M, Over EAB, van Giessen A, et al. Lifetime cost-effectiveness and equity impacts of the Healthy Primary School of the Future initiative. BMC Public Health. 2020;20(1):1887.
Arnold M, Nkhoma D, Griffin S. Distributional impact of the Malawian essential health package. Health Policy Plan. 2020;35(6):646–56.
Love-Koh J, Mirelman A, Suhrcke M. Equity and economic evaluation of system-level health interventions: a case study of Brazil’s Family Health Program. Health Policy Plan. 2020;36(3):229–38.
Pitt AL, Goldhaber-Fiebert JD, Brandeau ML. Public health interventions with harms and benefits: a graphical framework for evaluating tradeoffs. Med Decis Making. 2020;40(8):978–89.
Pecenka CJ, Johansson KA, Memirie ST, Jamison DT, Verguet S. Health gains and financial risk protection: an extended cost-effectiveness analysis of treatment and prevention of diarrhoea in Ethiopia. BMJ Open. 2015;5(4):e006402.
Driessen J, Olson ZD, Jamison DT, Verguet S. Comparing the health and social protection effects of measles vaccination strategies in Ethiopia: an extended cost-effectiveness analysis. Soc Sci Med. 2015;139:115–22.
Johansson KA, Strand KB, Fekadu A, Chisholm D. Health gains and financial protection provided by the ethiopian mental health strategy: an extended cost-effectiveness analysis. Health Policy Plan. 2017;32(3):376–83.
Johansson KA, Memirie ST, Pecenka C, Jamison DT, Verguet S. Health gains and financial protection from pneumococcal vaccination and pneumonia treatment in ethiopia: results from an extended cost-effectiveness analysis. PLoS ONE. 2015;10(12):e0142691.
De Neve JW, Andriantavison RL, Croke K, et al. Health, financial, and education gains of investing in preventive chemotherapy for schistosomiasis, soil-transmitted helminthiases, and lymphatic filariasis in Madagascar: a modeling study. PLoS Negl Trop Dis. 2018;12(12):7002.
Watkins DA, Olson ZD, Verguet S, Nugent RA, Jamison DT. Cardiovascular disease and impoverishment averted due to a salt reduction policy in South Africa: an extended cost-effectiveness analysis. Health Policy Plan. 2016;31(1):75–82.
Saxena A, Stacey N, Puech PDR, Mudara C, Hofman K, Verguet S. The distributional impact of taxing sugar-sweetened beverages: findings from an extended cost-effectiveness analysis in South Africa. BMJ Glob Health. 2019;4(4):1317.
Levin CE, Sharma M, Olson Z, et al. An extended cost-effectiveness analysis of publicly financed HPV vaccination to prevent cervical cancer in China. Vaccine. 2015;33(24):2830–41.
Nandi A, Megiddo I, Ashok A, Verma A, Laxminarayan R. Reduced burden of childhood diarrheal diseases through increased access to water and sanitation in India: a modeling analysis. Soc Sci Med. 2017;180:181–92.
Megiddo I, Colson A, Chisholm D, Dua T, Nandi A, Laxminarayan R. Health and economic benefits of public financing of epilepsy treatment in India: an agent-based simulation model. Epilepsia. 2016;57(3):464–74.
Nandi A, Colson AR, Verma A, Megiddo I, Ashok A, Laxminarayan R. Health and economic benefits of scaling up a home-based neonatal care package in rural India: a modelling analysis. Health Policy Plan. 2016;31(5):634–44.
Raykar N, Nigam A, Chisholm D. An extended cost-effectiveness analysis of schizophrenia treatment in India under universal public finance. Cost Effect Resour Alloc C/E. 2016;14:9–9.
Verguet S, Laxminarayan R, Jamison DT. Universal public finance of tuberculosis treatment in India: an extended cost-effectiveness analysis. Health Econ. 2015;24(3):318–32.
Verguet S, Nandi A, Filippi V, Bundy DAP. Maternal-related deaths and impoverishment among adolescent girls in India and Niger: findings from a modelling study. BMJ Open. 2016;6(9):11586.
Verguet S, Murphy S, Anderson B, Johansson KA, Glass R, Rheingans R. Public finance of rotavirus vaccination in India and Ethiopia: an extended cost-effectiveness analysis. Vaccine. 2013;31(42):4902–10.
Banham D, Lynch J, Karnon J. An equity-Effectiveness framework linking health programs and healthy life expectancy. Aust J Prim Health. 2011;17(4):309–19.
Golan O, Hansen P. Which health technologies should be funded? A prioritization framework based explicitly on value for money. Israel J Health Policy Res. 2012;1(1):44.
Cleary S, Mooney G, McIntyre D. Equity and efficiency in HIV-treatment in South Africa: the contribution of mathematical programming to priority setting. Health Econ. 2010;19(10):1166–80.
Potoglou D, Burge P, Flynn T, et al. Best–worst scaling vs discrete choice experiments: an empirical comparison using social care data. Soc Sci Med. 2011;72(10):1717–27.
Saksena P, Hsu J, Evans DB. Financial risk protection and universal health coverage: evidence and measurement challenges. PLoS Med. 2014;11(9):e1001701–e1001701.
Phelps CE, Lakdawalla DN, Basu A, Drummond MF, Towse A, Danzon PM. Approaches to aggregation and decision making-a health economics approach: an ISPOR special task force report [5]. Value Health. 2018;21(2):146–54.
Baltussen R, Niessen L. Priority setting of health interventions: the need for multi-criteria decision analysis. Cost Eff Resour Alloc. 2006;4:14–14.
Marsh K, Thokala P, et al. Multiple criteria decision analysis for health care decision making emerging good practices: report 2 of the ISPOR MCDA emerging good practices task force. Value Health. 2016;19(2):125–37.
Zopounidis C, Doumpos M. Multi-criteria decision aid in financial decision making: methodologies and literature review. J Multi Criteria Decis Anal. 2002;11(4–5):167–86.
Karvetski CW, Lambert JH, Linkov I. Emergent conditions and multiple criteria analysis in infrastructure prioritization for developing countries. J Multi Criteria Decis Anal. 2009;16(5–6):125–37.
Mardani A, Jusoh A, Md Nor K, Khalifah Z, Zakwan N, Valipour A. Multiple criteria decision-making techniques and their applications—a review of the literature from 2000 to 2014. Econ Res Ekonomska Istraživanja. 2015;28(1):516–71.
Epstein D, Chalabi Z, Claxton K, Sculpher M. Mathematical programming for the optimal allocation of healthcare resources. 2005.
National Institute for Health Research. Clinical Practice Research Datalink. In: National Institute for Health Research, ed. Vol 20202020.
NHS Digital. Hospital episode statistics. In: NHS Digital, ed2020.
The World Health Organization. Research for universal health coverage: World health report 2013. 2013.
Reckers-Droog V, van Exel J, Brouwer W. Equity weights for priority setting in healthcare: severity, age, or both? Value Health. 2019;22(12):1441–9.
McCabe C, Claxton K, Culyer AJ. The NICE cost-effectiveness threshold. Pharmacoeconomics. 2008;26(9):733–44.
Thokala P, Duenas A. Multiple criteria decision analysis for health technology assessment. Value Health. 2012;15(8):1172–81.
Wailoo A, Tsuchiya A, McCabe C. Weighting must wait: incorporating equity concerns into cost-effectiveness analysis may take longer than expected. Pharmacoeconomics. 2009;27(12):983–9.
Skedgel C, Wailoo A, Akehurst R. Societal preferences for distributive justice in the allocation of health care resources: a latent class discrete choice experiment. Med Decis Making. 2015;35(1):94–105.
Chang W-C. The meaning and goals of equity in health. J Epidemiol Community Health. 2002;56(7):488–91.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
This research was supported by a PhD studentship grant for Thomas Ward from the Dennis and Mereille Gillings Foundation.
Conflict of interest
Mr Ward received grants from the Dennis and Mereille Gillings Foundation during the conduct of the study. Dr Medina-Lara was a member of the National Institute for Health Research HTA Committee 2020–2024, the South West Research for Patient Benefit Programme 2021–2023, the NIHR Global Health Units Research Funding Committee 2021–2025, and the NIHR Global Health Groups Research Funding Committee 2021–2025. Dr Spencer and Dr Mujica-Mota have no conflicts of interest that are directly relevant to the content of this article.
Ethical approval
This article does not contain any studies with human participants and, as such, no ethical approval was required.
Consent to participate
Not applicable.
Consent for publication
Not applicable.
Availability of data and material
Not applicable
Code availability
Not applicable
Author contributions
All authors contributed to the concept and design, drafting, and critical revision of the manuscript. TW and AML contributed to the acquisition of data and the provision of study materials. AS, AML, and RMM provided supervision to TW throughout the manuscript development. AS assisted with attaining funding through TW’s PhD grant, and TW contributed to the analysis and interpretation of data as well as administrative support.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Ward, T., Mujica-Mota, R.E., Spencer, A.E. et al. Incorporating Equity Concerns in Cost-Effectiveness Analyses: A Systematic Literature Review. PharmacoEconomics 40, 45–64 (2022). https://doi.org/10.1007/s40273-021-01094-7
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40273-021-01094-7